Chapter: Medical Surgical Nursing: Pain Management
Characteristics of Pain
CHARACTERISTICS
OF PAIN
The factors to consider in a complete pain assessment are the
in-tensity, timing, location, quality, personal meaning, aggravating and
alleviating factors, and pain behaviors. The pain assessment begins by
observing the patient carefully, noting the patient’s overall posture and
presence or absence of overt pain behaviors and asking the person to describe,
in his or her own words, the specifics of the pain. The words used to describe
the pain may point toward the etiology. For example, the classic description of
chest pain that results from a myocardial infarction includes pres-sure or
squeezing on the chest. A detailed history should follow the initial
description of pain.
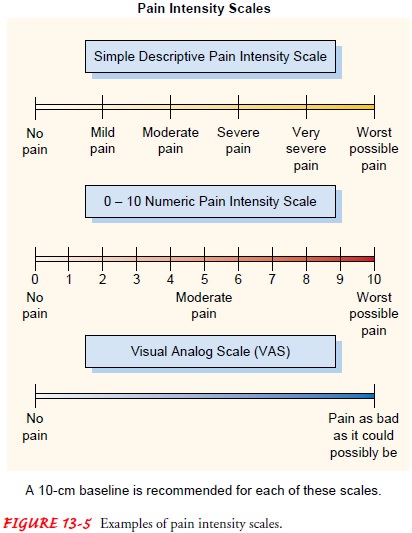
Intensity
The intensity of pain
ranges from none to mild discomfort to ex-cruciating. There is no correlation
between reported intensity and the stimulus that produced it. The reported
intensity is influ-enced by the person’s pain
threshold and pain tolerance.
Pain threshold is the smallest stimulus for which a person reports pain, and
the tolerance is the maximum amount of pain a person can tolerate. To
understand variations, the nurse can ask about the present pain intensity as
well as the least and the worst pain in-tensity. Various tools and surveys are
helpful to patients trying to describe pain intensity. Examples of pain scales
appear in Fig-ure 13-5.
Timing
Sometimes the etiology of pain can be determined when time aspects are known. Therefore, the nurse inquires about the onset,duration, relationship between time and intensity, and whether there are changes in rhythmic patterns. The patient is asked if thepain began suddenly or increased gradually. Sudden pain that rapidly reaches maximum intensity is indicative of tissue rupture,and immediate intervention is necessary. Pain from ischemia gradually increases and becomes intense over a longer time. Thechronic pain of arthritis illustrates the usefulness of determining the relationship between time and intensity, because people witharthritis usually report that pain is worse in the morning.
Location
The location of pain is
best determined by having the patient point to the area of the body involved.
Some general assessment forms have drawings of human figures, and the patient
is asked to shade in the area involved. This is especially helpful if the pain
radiates (referred pain). The shaded
figures are helpful in deter-mining the effectiveness of treatment or change in
the location of pain over time.
Quality
The nurse asks the
patient to describe the pain in his or her own words without offering clues.
For example, the patient is askedto describe what the pain feels like.
Sufficient time must be al-lowed for the patient to describe the pain and for
the nurse to carefully record all words that are used. If the patient cannot
de-scribe the quality of the pain, words such as burning, aching, throbbing, or
stabbing can be offered. It is important to docu-ment the exact words used to
describe the pain and which words were suggested by the nurse conducting the
assessment.
Personal Meaning
Patients experience pain differently, and the pain experience can mean many different things. It is important to ask how the pain has affected the person’s daily life. Some people can continue to work or study, while others may be disabled. The patient is asked if family finances have been affected. For others, the recurrence of pain may mean worsening of the disease, such as the spread of cancer. The meaning attached to the pain experience helps the nurse understand how the patient is affected and assists in plan-ning treatment.
Aggravating and Alleviating Factors
The nurse asks the patient what if anything makes the pain worse and
what makes it better and asks specifically about the relation-ship between
activity and pain. This helps detect factors associ-ated with pain. For
example, in a patient with advanced metastatic cancer, pain with coughing may
signal spinal cord compression. The nurse ascertains whether environmental
factors influence pain since they may easily be changed to help the patient.
For ex-ample, making the room warmer may help the patient relax and may improve
the patient’s pain. Finally, the patient is asked if pain is influenced by or
affects the quality of sleep or anxiety. Both can significantly affect pain
intensity and the quality of life.
Knowledge of alleviating
factors assists the nurse in develop-ing a treatment plan. Therefore, it is
important to ask about the patient’s use of medication (prescribed and over the
counter) and the amount and frequency. In addition, the nurse asks if herbal
remedies, nonpharmacologic interventions, or alternative thera-pies have been
used with success. This information assists the nurse in determining teaching
needs.
Pain Behaviors
When experiencing pain, people express pain with many differ-ent behaviors. These nonverbal and behavioral expressions of pain are not consistent or reliable indicators of the quality or in-tensity of pain, and they should not be used to determine the presence of or the degree of pain experienced. Patients may gri-mace, cry, rub the affected area, guard the affected area, or im-mobilize it. Others may moan, groan, grunt, or sigh. Not all patients exhibit the same behaviors, and there may be different meanings associated with the same behavior.
Sometimes in the
nonverbal patient, pain behaviors are used as a proxy to assess pain. It is
unwise to make judgments and for-mulate treatment plans based on behaviors that
may or may not indicate pain. In the case of an unconscious person, pain should
always be assumed to be present and treated. All patients have a right to
adequate pain management.
Physiologic responses to
pain, such as tachycardia, hyperten-sion, tachypnea, pallor, diaphoresis,
mydriasis, hypervigilance, and increased muscle tone, are related to
stimulation of the autonomic nervous system. These responses are short-lived as
the body adapts to the stress. These physiologic signs could be the re-sult of
a change in the patient’s condition, such as the onset of hypovolemia. Using
physiologic signs to indicate pain is unreliable. Although it is important to
observe for any and all pain behav-iors, the absence of these behaviors does
not indicate an absence of pain.
Related Topics