Chapter: Medical Surgical Nursing: Pain Management
Instruments for Assessing the Perception of Pain
INSTRUMENTS
FOR ASSESSING THE PERCEPTION OF PAIN
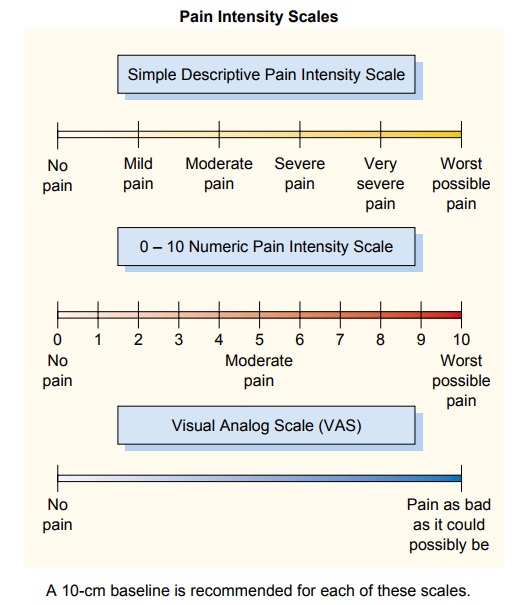
Only the patient can accurately describe and assess his or her pain. Clinicians consistently underestimate a patient’s level of pain (McCaffery & Ferrell, 1997; McCaffery, Ferrell & Pasaro, 2000; Puntillo, Miaskowski, Kehrle et al., 1997; Thomas et al., 1998). Therefore, a number of pain assessment instruments have been developed to assist in the assessment of a patient’s percep-tion of pain (see Fig. 13-5). Such instruments may be used to document the need for intervention, to evaluate the effectiveness of the intervention, and to identify the need for alternative or ad-ditional interventions if the initial intervention is ineffective in relieving the pain. For a pain assessment instrument to be useful, it must require little effort on the part of the patient, be easy to understand and use, be easily scored, and be sensitive to small changes in the characteristic being measured.
Figure 13-6 shows a pain assessment algorithm that
can be used at the time of as-sessment to direct clinical decisions for pain
management.
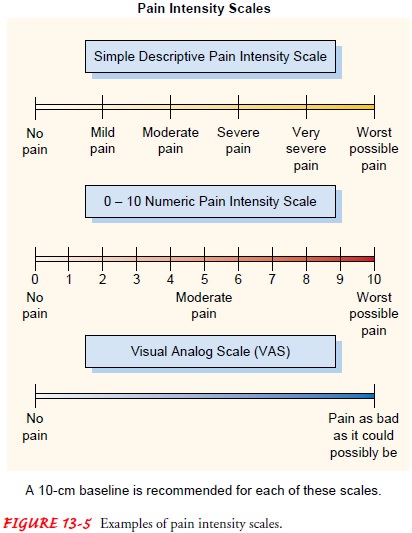
Visual Analogue Scales
Visual analogue scales (VAS; see Fig. 13-5) are useful in assessing the
intensity of pain. One version of the scale includes a hori-zontal 10-cm line,
with anchors (ends) indicating the extremes of pain. The person is asked to
place a mark indicating where the current pain lies on the line. The left
anchor usually represents “none” or “no pain,” whereas the right anchor usually
represents “severe” or “worst possible pain.” To score the results, a ruler is
placed along the line and the distance the person marked from the left or low
end is measured and reported in millimeters or centimeters.
Some patients (eg,
children, elderly patients, and visually or cognitively impaired patients) may
find it difficult to use an un-marked VAS. In those circumstances, ordinal
scales (simple de-scriptive pain intensity scale, or 0 to 10 numeric pain
intensity scale) may be used.
Faces Pain Scale, Revised
This instrument has seven faces depicting expressions that range from
contented to obvious distress. The patient is asked to point to the face that
most closely resembles the pain intensity felt. Evidence for reliability and
validity has been established (Hicks, van Baeyer, Spafford et al., 2001;
Hunter, McDowell, Hennessy et al., 2000). Figure 13-7 shows the Faces Pain
Scale, Revised.
Guidelines for Using Pain Assessment Scales
Using a written scale to assess pain may not be possible if the per-son
is seriously ill, is in severe pain, or has just returned from surgery. In
these cases, the nurse can ask the patient, “On a scale of 0 to 10, 0 being no
pain and 10 being pain as bad as it can be, how bad is your pain now?” For
patients who have difficulty with a 0 to 10 scale, a 0 to 5 scale may be tried.
Whichever scale is used, it should be used consistently. Most patients usually
can respond without difficulty. Ideally, the nurse teaches the patient how to
use the pain scale before the pain occurs (eg, before surgery). The patient’s
numerical rating is documented and used to assess the effectiveness of pain
relief interventions.
If the person does not speak English or cannot communicate clearly
information needed to manage pain, an interpreter, trans-lator, or family
member familiar with the person’s method of communication should be consulted
and a method established for pain assessment. Often a chart can be constructed
with Eng-lish words on one side and the foreign language on the other. The
patient can then point to the corresponding word to tell the clini-cian about
the pain.
When a person with pain is cared for at home by family care-givers or the home care nurse, a pain scale may help in assess-ing the effectiveness of the interventions, if the scale is used before and after the interventions are administered. Scales that address the location and pattern of pain may be useful to the home care nurse in identifying new sources or sites of pain in the chronically or terminally ill patient and in monitoring changes in the patient’s level of pain. The patient and family caregivers can be taught to use a pain assessment scale to assess and manage the patient’s pain. The home care nurse who sees the patient only at intervals may thus benefit from consulting the patient’s or family’s written record of the pain scores to eval-uate how effective the pain management strategies have been over time.
On occasion, a person
will deny having pain when most peo-ple in similar circumstances would report significant
pain. For example, it is not uncommon for a patient recovering from a total
joint replacement to deny feeling “pain,” but on further questioning will
readily admit to having a “terrible ache, but I wouldn’t call it pain.” From
then on, when evaluating this per-son’s pain, the nurse would use the patient’s
words rather than the word “pain.”
Related Topics