Chapter: Modern Medical Toxicology: Neurotoxic Poisons: Drugs Used in Psychiatry
Monoamine Oxidase Inhibitors (MAOIs) - Antidepressants
Monoamine Oxidase Inhibitors (MAOIs)
·
Today MAOIs have been largely replaced by the cyclic
antide-pressants for the treatment of a variety of psychiatric disorders, but
continue to be used in certain types of anxiety and phobias as well as
treatment-resistant depression.
·
Examples of MAOIs include clorgyline, isocarboxacid,
iproniazid, lazabemide, moclobemide, pargyline, phenel-zine, pimozide,
selegiline, toloxatone, and tranylcypromine. Irreversible MAOIs such as
clorgyline, isocarboxacid, phenel-zine, tranylcypromine, and selegiline are
used in the treatment of Parkinsonism. Procarbazine, an antineoplastic agent
used in Hodgkin’s disease has weak MAOI activity.
Uses
Monoamine
oxidase inhibitors (MAOIs) are useful in the treat-ment of depression,
agoraphobia, anxiety disorders, bulimia, migraine, panic disorders,
obsessive-compulsive disorders, phobic disorders, narcolepsy and Parkinson’s
disease.
Toxicokinetics
Monoamine
oxidase inhibitors (MAOIs) are rapidly absorbed on oral administration and are
metabolised by acetylation, followed by urinary excretion.
Mode of Action
·
The MAOIs act (obviously) by
inhibiting monoamine oxidase which is a flavin-containing enzyme located in the
mitochondrial membrane of liver and central as well as peripheral sympathetic
nerve terminals. Monoamine oxidase oxidatively deaminates and inactivates
mono-amines, some of which are essential as neurotransmit-ters or modulators of
nervous system transmission, e.g.noradrenaline, dopamine, adrenaline, and
serotonin. As a result of MAO inhibition, the pool of noradrenaline in the
presynaptic sympathetic nerve terminal is expanded which causes the elevation
of CNS noradrenaline and dopamine. This is presumed to be the reason for the
antidepressant effect of MAOIs.
·
Some MAOIs are selective for the monoamine
oxidase-A enzyme, located primarily in the placenta, intestines and liver.
Others are selective for the monoamine oxidase enzyme B, located primarily in
the platelets, brain and liver.
·
Others are non-selective.
Selectivity is lost in overdose.
o Meclobemide
(reversible) and clorgyline (irreversible) are selective MAO-A inhibitors.
o Lazabemide,
pargyline and selegiline are selective MAO B inhibitors.
o Phenelzine,
tranylcypromine and isocarboxazid are non-selective MAOIs.
Adverse Effects and Drug Interactions
·
Patients taking MAOIs are prone for multiple food and drug
interactions some of which are life-threatening. Many such reported instances
involve the concomitant intake of sympathomimetic agents such as ephedrine and
phenylpro- panolamine, or the ingestion of foods containing tyramine.*
Sympathomimetic agents act by causing the release of noradrenaline stored in
the peripheral sympathetic nerve terminals. The already expanded pool of
noradrenaline arising out of MAO inhibition is greatly aggravated by this
release, resulting in hypertension, tachycardia, (sometimes bradycardia),
severe occipital headache, hyperthermia, altered mental status, convulsions,
and even intracranial haemorrhage and death.
·
While most sympathomimetic agents are capable of producing
this reaction, there are exceptions, e.g. adrenaline, noradrenaline and
isoproterenol, which do not release a stored pool of noradrenaline, but instead
bind directly with postsynaptic alpha- and beta-adrenergic receptors. Apart
from sympathomimetic drugs, there are a number of other drugs with which the
MAOIs interact adversely (Table 19.7).
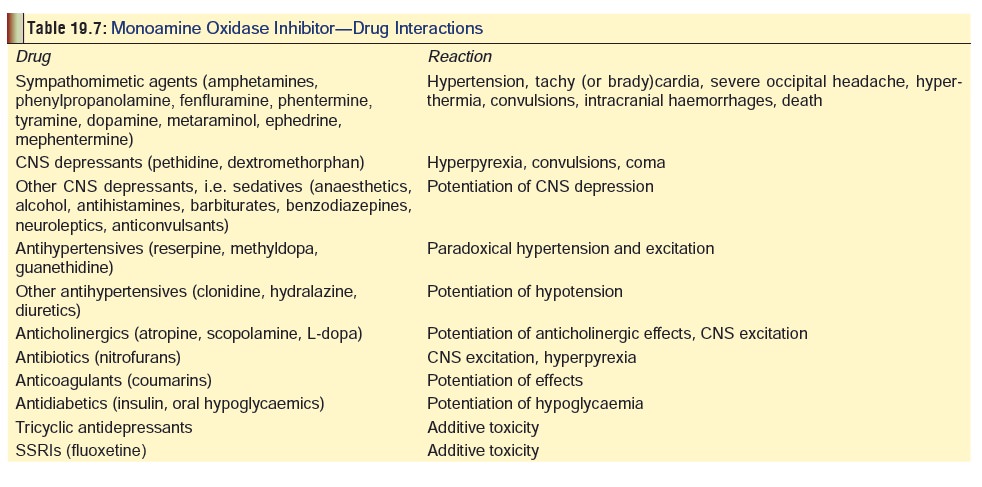
·
Combination of MAOIs with indirect acting sympatho- mimetic
drugs can cause severe hypertension. Drugs with the potential to cause this
reaction include amphetamines, dopamine, cocaine, phentermine, ephedrine,
metaraminol, and phenylpropanolamine.
·
With reference to the reaction with tyramine, a similar
mechanism is postulated. Pharmacologically active dietary monoamines are found
in substantial quantities in protein foods which contain decarboxylating
bacteria. Amino acids are converted to monoamines (tyramines, histamine,
phenylethylamine) which are normally degraded in the GI tract and liver by MAO,
but in the setting of MAO inhibition large amounts of these mono-amines enter
the systemic circulation, release stored noradrenaline, and cause a severe
hypertensive crisis. Foods capable of producing this tyramine reaction are
listed in Table 19.8.
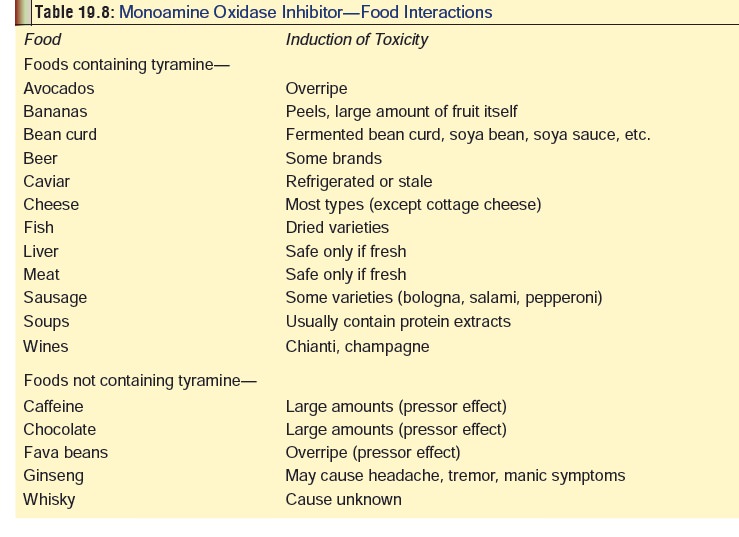
·
It must be mentioned that the tyramine reaction is mainly
associated with irreversible MAOIs, while reversible MAOIs do not normally
induce such a reaction, e.g. brofaromine, cimoxatone and moclobemide.
· The MAOIs are also capable of causing the serotonin syndrome, especially when combined with selective serotonin reuptake inhibitors (SSRIs). At least 14 days should elapse between the discontinu-ation of an MAOI and the initiation of SSRI therapy. In some cases, e.g. fluoxetine, this interval may have to be prolonged upto 4 to 5 weeks. Combination of MAOIs with tricyclics can also produce serious (even fatal) reactions, though the practice of combined therapy is actually quite common.
·
Addicts who abuse cocaine are at special risk of suffering a
severe reaction when they are on MAOI medication. Features include severe
headache, hyperthermia, tremor, convulsions, and death.
Clinical (Toxic) Features
· Overdose is characterised by an
initial delay in presentation of upto 12 hours or more.
· Symptoms include anxiety, flushing,
headache, nausea, tachycardia/bradycardia, hypertension/hypotension,
agita-tion, delirium, hallucinations, nystagmus, tremors, muscle rigidity,
trismus, opisthotonus, convulsions, hyperthermia, profuse sweating, tachypnoea,
respiratory depression, and cardiovascular collapse.
· Pupils may be dilated and minimally
reactive to light after MAOI overdose or MAOI-induced serotonin syndrome. Ping
pong gaze (rhythmic and pendular, conjugate horizontal eye movements) has been described
in some cases of MAOI overdose.
· Death occurs in some cases from
complications such as ARDS, DIC, and myoglobinuric renal failure.
· Overdose complicated by
rhabdomyolysis or hypotension often leads to myoglobinuria, acute tubular
necrosis and renal failure.
· Coagulopathy, haemolysis and
thrombocytopenia may develop with MAOI overdose.
·
The newer reversible, selective inhibitors of MAO-A (e.g.
moclobemide) appear to have a less severe toxicity profile when used in
overdose. They have also been suggested to interact less with tyramine than
traditional MAOIs and thus may have less potential to cause hypertensive crisis
when tyramine-containing foods are ingested.
·
Chronic use of these drugs (especially phenelzine and
tranylcypromine) can lead to withdrawal reaction on abrupt cessation,
characterised by anxiety, depression, confusion, hallucinations, nausea,
vomiting, diarrhoea and chills.
Usual Fatal Dose
Ingestion
of greater than 2 to 3 mg/kg of an MAOI should be considered potentially
life-threatening, and 4 to 6 mg/kg or greater is consistent with reported
fatalities.
Treatment
·
Due to the potential for delayed and severe toxicity, any
patient with a history of acute MAOI overdose, even in the absence of symptoms
in the first 4 to 6 hours, should be admitted for ICU monitoring and remain
until stable for 24 hours. The following measures are suggested for the
treatment of adverse as well as toxic effects of MAOIs:
·
Maintenance of airway, oxygen, assisted ventilation, etc.
(as needed).
·
Cardiac monitoring.
·
Electrolytes should be monitored closely, particularly for
hyperkalaemia.
·
Monitor liver and renal function, and CPK level.
·
Severe hypertension should be treated with IV sodium
nitroprusside or phentolamine. Methyldopa and guanethi-dine are contraindicated
as they may potentiate hyper-tensive crises.
·
Hypotension (or shock) can be managed by IV fluids, and
vasopressors such as noradrenaline or dopamine, i.e. direct-acting
alpha-adrenergic agonists.
·
Ventricular tachyarrhythmias usually respond to ligno-caine,
phenytoin, or procainamide.
·
If the patient is seen within a short time of overdosing,
gut decontamination must be carried out—lavage, activated charcoal, cathartics.
·
Acidic diuresis and haemodialysis have been tried with
varying degree of success but are probably best avoided. Although MAO inhibitor
excretion is enhanced by forced acid diuresis, there is no evidence that it is
effective in reducing the severity of an overdose. In fact, such a procedure
may be dangerous in this situation because of the instability of the
cardiovascular system.
·
Muscle rigidity and agitation may respond to phenothi-azines
such as chlorpromazine. Diazepam is however safer, and phenytoin is a good
alternative. In the presence of intractable muscle rigidity, neuromuscular
paralysis with pancuronium may be necessary.*
·
Seizures are best treated with benzodiazepines or
barbi-turates.
·
Hyperthermia can be managed with paracetamol and external
cooling. In severe cases (malignant hyperthermia-type), IV dantrolene is given
at a dose of 2.5 mg/kg, every 6 hours, for 24 hours. As an alternative,
bromocriptine can be administered.
·
For rhabdomyolysis: Early aggressive fluid replacement is
the mainstay of therapy and may help prevent renal insufficiency. Diuretics
such as mannitol or furosemide may be needed to maintain urine output. Urinary
alka-linisation is not routinely recommended. Initial treatment should be
directed towards controlling acute metabolic disturbances such as
hyperkalaemia, hyperthermia, and hypovolaemia. Control seizures, agitation, and
muscle contractions.
·
Serotonin syndrome must be treated on the recommended lines
outlined under SSRIs.
·
Patients should be placed on special diets low in
tyra-mine-containing foods for at least 2 weeks post-exposure.
Related Topics