Chapter: Modern Medical Toxicology: Neurotoxic Poisons: Drugs Used in Psychiatry
Classical Neuroleptics
Classical Neuroleptics
Uses
· Neuroleptics are used in the
treatment of schizophrenia, manic phase of manic-depressive illness, severe
depression associated with psychosis, and organic psychotic states.
· Phenothiazines are particularly
useful in the treatment of amphetamine intoxication, anxiety, dysreflexia,
behaviour problems, depression, chemotherapy-induced emesis, mania, porphyria
and schizophrenia.
· Phenothiazine itself is used as an
insecticide, in the manu-facture of dyes, as a polymerisation inhibitor,
antioxidant, chain transfer agent in rubber production, as a parent compound
for chlorpromazine as well as related antipsy-chotic drugs, as a urinary
antiseptic, and as an anthelmintic drug.
· Thioxanthenes are also used for the
treatment of psychosis and schizophrenia. Flupenthixol is primarily used for
the treatment of acute and chronic psychoses. Although it has been studied in
depressive illnesses and cocaine withdrawal, further research is needed.
· Haloperidol and benperidol are used
to treat schizophrenia and acute psychosis; schizoaffective disorders; paranoid
syndrome; and Tourette’s syndrome. Haloperidol is frequently used for agitation
or aggressive behaviour, espe-cially in elderly patients. Droperidol is used as
an antiemetic and sedative.
· Molindone is a dihydroindolone
antipsychotic agent. It is not structurally related to the phenothiazines, the
buty-rophenones or the thioxanthenes. It is indicated for the management of the
manifestations of psychotic conditions (e.g. chronic schizophrenia, brief
reactive psychosis, or schizophreniform disorders).
· Pimozide is a drug that belongs to
the diphenylbutylpiperi-dine group of neuroleptics, and is an orally active antip-sychotic
drug, which shares with other antipsychotics the ability to block dopaminergic
receptors on neurons in the central nervous system. It is indicated for the
suppression of motor and phonic tics in patients with Tourette’s disorder who
have failed to respond satisfactorily to standard treat-ment. The ability of
pimozide to suppress motor and phonic tics in Tourette’s Disorder is thought to
be a function of its dopaminergic blocking activity. Pimozide has also been
used in the treatment of schizophrenia.
Mode of Action
· Neuroleptics inhibit the activity of
a variety of receptors— dopaminergic, cholinergic, alpha1 and alpha2
adrenergic, histaminic, and serotonergic (5HT2). Neuroleptic
activity is thought to be related to the dopamine-receptor blocking activity in
the limbic system. There are 6 sub-types of dopamine receptor – D1,
D2A, D2b , D3 , D4 , and D5.
Most neuroleptics have a high affinity for D2 and D3
receptors. Some neuroleptics (thioxanthenes and phenothiazines) bind with great
affinity to D1 , D2 , D3 , and D4
sub-types, while haloperidol and pimozide have high selectivity at D2
and D3 receptors and less D4 affinity.
· Phenothiazines are neuroleptic
agents which affect four anatomical sites of action, specifically the reticular
acti- vating system of the midbrain, the limbic system, the hypothalamus, and
the globus pallidus and corpus striatum. Antipsychotic effects of
phenothiazines are still not understood completely but suggested mechanisms
include post-synaptic block of adrenergic or dopaminergic receptor sites,
metabolic inhibition of oxidative phosphorylation,or decrease in the
excitability of the neuronal membranes. They possess significant
anticholinergic, alpha-adrenergic blocking, quinidine-like and extrapyramidal
effects. Since the phenothiazines also lower the seizure threshold, large doses
may produce seizures.
· Like other neuroleptics,
flupenthixol is an antagonist at postsynaptic D1 and D2
dopamine receptors. Low doses of flupenthixol may exert selective effects on
inhibitory presynaptic dopamine autoreceptors. This may partially explain its
activating and antidepressant properties.
· Thiothixene has some pharmacological
properties in common with the piperazine phenothiazines; mode of action has not
been clearly established.
· Similar to other neuroleptics,
haloperidol centrally blocks the action of dopamine by binding previously to D2A
recep- tors, and to a lesser extent, D1A receptors. The potency of
all antipsychotic drugs correlates well with their affinity for D2A
receptors.
· Pimozide is a neuroleptic which is
thought to act by decreasing the permeability of membranes covering dopa-
minergic receptors. This prevents released neurotransmit- ters from reaching
these sites. Pimozide binds preferentially to dopamine-2 receptors (as do the
butyrophenones), whereas phenothiazines bind more selectively to dopa-mine-1
receptors. This may explain pimozides's efficacy in the treatment of Gilles de
la Tourette and other tic disorders, as well as its unique side effect profile
(vide infra).
Toxicokinetics
â– â– All dopamine receptor antagonists
are generally well absorbed on oral or parenteral administration. Haloperidol
is readily absorbed (60 to 70%) from the gastrointestinal tract. Plasma
concentrations usually peak 1 to 4 hours after ingestion and ½ to 1 hour after
intramuscular injection. Following oral administration, haloperidol is
detectable in the plasma within 1 hour with peak values occurring at 3 to 6
hours. A number of factors interfere with GI absorp-tion—antacids, caffeine,
smoking, and food.
â– â– Most
antipsychotics are highly lipophilic and accumulate in fat, lungs, and brain.
They are generally highly protein-bound. Protein binding is over 90% for
haloperidol.
â– â– Metabolism
is largely hepatic and occurs through conju-gation with glucuronic acid,
hydroxylation, oxidation, demethylation, and sulfoxide formation, by cytochrome
P450 (CYP)2D6 and CYP3A isoenzymes. Systemic clear-ance is high because of a
high hepatic extraction ratio, and only negligible amounts of the unchanged
drug are excreted in the urine.
â– â– The
toxicokinetics of long-acting (injectable) antipsy-chotics differ greatly from
those of short-acting (oral and injectable) drugs. Long-acting compounds take
much longer to reach steady state and are eliminated very slowly.
â– â– Pimozide
is slowly absorbed, and peak plasma levels are noted around 8 hours. Protein
binding is reported to be 99%. Pimozide is metabolised in the liver by
oxidative N-dealkylation to at least two metabolites thought to be inactive.
The kidney is the major route of elimination.
â– â– Elderly
patients should be prescribed lower than usual dosages of antipsychotics owing
to decreased renal clear-ance, diminished cardiac output, decreased liver size,
and weaker P450 activity.
Adverse and Toxic Effects
Neurological:
·
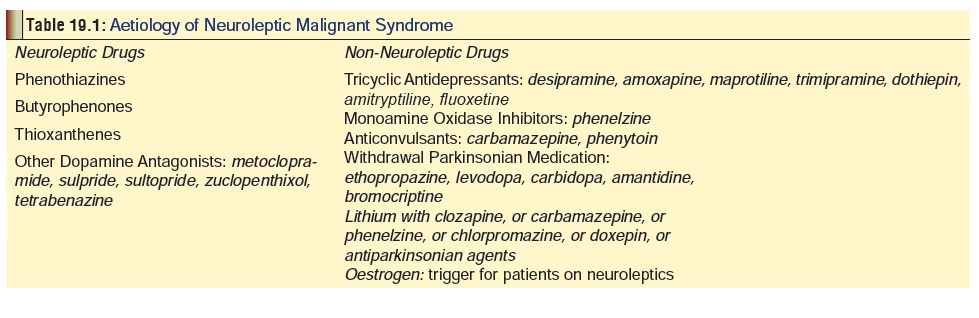
Neuroleptic malignant syndrome (NMS): This was firstdescribed in 1968
and is a rare complication occurring in about 0.02 to 2.4% of patients taking
antipsychotic medication. However, NMS can be caused by other drugs also (Table 19.1). Among the neuroleptics,
NMS is most frequently associated with phenothiazines, buty-rophenones, and
thioxanthines. Several cases have been reported with therapeutic doses of
haloperidol. Among the phenothiazines, NMS appears most commonly following
fluphenazine decanoate administration or withdrawal.
o
NMS is believed to be an idiosyncratic reaction and carries
with it a high mortality (20 to 40%).
o
The syndrome is twice as common in males as in females, and
is more likely to occur in younger patients.
o
The pathophysiology is thought to be central dopa-mine
blockade, and symptoms usually begin 3 to 9 days after neuroleptic treatment,
lasting for about 5 to 10 days even after discontinuing the drug.
o In essence, NMS is a severe form of extrapyramidal reaction and is manifested by hyperthermia (39° C to 42° C), muscular hypertonicity (generalised “lead pipe” rigidity, akinesia, tremor, choreoathetosis), fluctuating mental status (confusion, agitation, stupor), and autonomic irregularities (tachycardia, labile blood pressure, tachypnoea, urinary inconti-nence, respiratory stridor, sweating, cardiac arrest).
o
Complications include rhabdomyolysis, aspira-tion pneumonia,
pulmonary embolism, pulmonary oedema, ARDS, DIC, seizures, myocardial infarc-tion,
peripheral neuropathy and death.
o
Laboratory investigations indicate the presence of metabolic
acidosis, liver enzyme abnormalities, leukocytosis, and elevation of creatinine
as well as creatine phosphokinase.
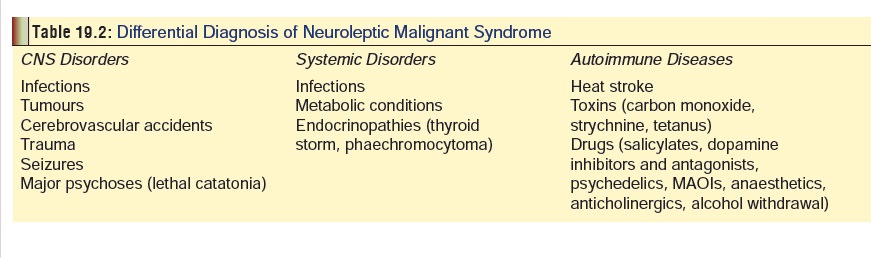
o
Differential diagnosis includes all causes of fever,
leukocytosis, and rigidity (Table 19.2).
Acute extrapyramidal syndromes: These syndromesresult from
decreased dopamine activity in the basal ganglia and have their onset soon
after initiation of antipsychotic drug therapy, but disappear once the drug use
is discontinued.
·
Akathisia—It is the most common and most distressing of the
acute extrapyramidal syndromes resulting from antipsychotic therapy and is
charac-terised by a sensation of restlessness manifesting as agitation,
fidgeting, restless legs, hostility, and belligerence. This may mislead the
clinician into believing that the patient requires an increased dosage of the
drug which will only worsen the condition. Akathisia is more frequently
encountered in elderly patients.
· Acute dystonia—This is more common in children and male adults administered butyrophenones and piperazines and is characterised by oculogyric crisis (upward gaze paralysis), spasms of jaw and throat, tongue protrusion, torticollis (neck twisting), retro-collis (spasm of back of neck), opisthotonus, facial grimacing, tortipelvis (abdominal wall spasm), and laryngeal dystonia which can be life threatening.
·
Parkinsonism—This is more common in elderly patients and
manifests classically as akinesia, rigidity, shuffling gait, mask-like facies,
and tremor.
·
Examination often reveals a positive glabella tap.
Chronic extrapyramidal syndromes:
·
Tardive dyskinesia—This is the most serious side effect of
long term phenothiazine and haloperidol treatment. Elderly women are most
susceptible. Manifestations are quite disabling and comprise facial gimacing,
eye blinking, furrowing of eyebrows, lip smacking, tongue protrusion, jaw
deviation, and choreoathetoid-like movements of the limbs. These features are
completely absent in sleep. Once estab-lished, tardive dyskinesia may take a
long time to disappear, and sometimes becomes permanent.
·
Rabbit syndrome—This is characterised by rhythmic
involuntary movements of the oral and masticatory musculature mimicking the
chewing movements of a rabbit. It may be irreversible.
Cardiovascular:
·
Common cardiovascular adverse effects include orthos-tatic
(or postural) hypotension, cardiac arrhythmias, and ECG anomalies (prolongation
of PR, QRS, and QTc intervals, blunt T waves, and depressed ST segments).
·
Cardiac arrest and sudden death have been reported in
overdose patients.
·
Ventricular tachycardia may progress to torsades de pointes
or ventricular fibrillation and can be difficult to treat.
· Among the phenothiazines,
thioridazine and mesori-dazine are associated with maximum cardiotoxicity.
Gastrointestinal:
Gastrointestinal toxic effects manifest as dry mouth and constipation; less
commonly there may be vomiting or diarrhoea.
Other
Systems:
·
Urinary retention may result from the anticholinergic effect
of many of these drugs.
·
Leukopenia, thrombocytopenia, agranulocytosis, and
pancytopenia are rare complications.
·
Skin rash occasionally occurs. Photosensitivity reac-tions
are not uncommon, and therefore patients should be instructed to avoid direct
sunlight.
·
High-dose thioridazine therapy can cause retinal
pigmentation and blindness. Presumably, other pheno-thiazines can also cause
this effect.
·
Female patients may experience galactorrhoea, breast enlargement,
and irregular menses while on antipsy-chotic medication owing to increased
circulating prol-actin concentrations. In males there may be decreased libido,
erectile disurbances, and ejaculatory problems. Priapism associated with the
therapeutic use of chlor-promazine, thioridazine, mesoridazine, and
fluphena-zine has been reported.
·
An absent gag reflex and swallowing difficulties have been
associated with phenothiazine therapy. Sudden death due to asphyxiation and/or
aspiration of gastric content has occurred secondary to the absent gag reflex.
·
Hepatic disease has been associated with almost all of the
phenothiazines. Cholestatic jaundice or mixed cholestatic and hepatocellular
jaundice, not necessarily related to either dose or duration of therapy, are
the most common hepatic problems associated with therapeutic use and overdose.
·
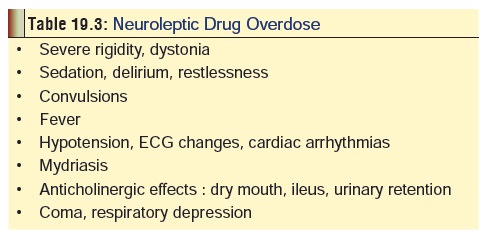
Acute overdoses of antipsychotic drugs result in the
exaggeration of the usual adverse effects already described, and summarised in Table 19.3.
o
Phenothiazines may interfere with the body’s ability to
thermoregulate, and cause hyperthermia or hypo-thermia. Hypothermia may occur
with therapeutic use and overdose of phenothiazines and related agents; the
elderly are especially vulnerable.
o Hypotension and hypertension have both been reported; hypotension is the more common serious effect. Patients who overdose on thioridazine may experience late onset atrioventricular block.
o
Cardiac disorders may be most pronounced 10 to 15 hours
after ingestion.
o
Chlorpromazine has been reported to cause coma with
pulmonary oedema with ingestion of overdose.
o
Patients who have overdosed on phenothiazines and related
agents may develop rhabdomyolysis secondary to episodes of neuroleptic
malignant syndrome, seizures or prolonged immobility. Rhabdomyolysis is often
followed by acute renal insufficiency.
o
Mydriasis is common with ingestion of chlorproma-zine and
thioridazine.
o
Most common manifestations of acute intoxication with
chlorprothixene include somnolence, coma, miosis, seizures, hypotension,
cardiac arrhythmias, and respiratory depression. Possible sequelae include
acute reversible renal failure.
o
Flupenthixol overdose results in extrapyramidal movements,
somnolence, and tardive dyskinesia, while thiothixene causes hypotension,
somnolence, extrapyramidal signs, and tardive dyskinesia.
o
Most common major signs of acute intoxication with
haloperidol include somnolence, coma, respiratory depression, extrapyramidal
signs, cardiac arrhyth-mias, and hypotension. Premature ventricular
contractions, ventricular arrhythmias, torsades de pointes, and bradycardia
have been reported with overdose. Cases of QT prolongation and/or torsades de
pointes have been reported in patients receiving droperidol at doses at or
below recommended doses. Some cases have occurred in patients with no known
risk factors for QT prolongation and some cases have been fatal. Possible
sequelae with haloperidol include neuroleptic malignant syndrome and acute
renal failure. Extrapyramidal effects are common with both droperidol and
haloperidol therapy. Potentially irreversible, involuntary dyskinetic movements
may develop in some patients treated therapeutically with haloperidol. Elderly
women appear at greatest risk. These signs may also occur with overdose. Sudden
death has been reported in young, otherwise healthy adults given large
thera-peutic doses of haloperidol or droperidol.
o
Molindone is somewhat less likely than other neuroleptics to
cause hypotension, but may cause sedation. It can however facilitate the onset
of neuroleptic malignant syndrome. Extrapyramidal effects (rigidity, tremor,
akathisia, major tonic spasms and tardive dyskinesia) are likely with large
doses. Especially in patients who have previous exposure to neuroleptics,
therapeutic administration and overdose may facilitate rhabdomyolysis with high
CPK levels, myoglobinuria, hyperkalaemia, acid-base derangements and subsequent
acute renal failure. Although most neuroleptic drugs are asso-ciated with weight
gain, molindone appears to be more often associated with weight loss. Menstrual
abnormalities can occur with molindone therapy (heavy menstrual flow,
amenorrhoea.).
o
Intoxication with dibenzoxapines can result in respiratory
depression, hypotension, prolonged seizures, coma, hyperthermia, rhabdomyolysis
and renal failure. Cardiac arrhythmias and conduction delays are not a
prominent feature of overdose, but have been reported, usually in patients with
severe neurologic toxicity: supraventricular tachycardia, atrial flutter,
premature ventricular contractions, nonspecific ST segment and T wave changes,
QRS prolongation, bradycardia, and myocardial failure. Anticholinergic effects
are not prominent. Pupils may be dilated but usually respond to light; blurred
vision may occur secondary to loss of accom-modation reflexes. Miosis has also
been reported, usually in patients with seizures or CNS depression. Mortality
is most often due to complications of intractable seizures or brain death.
o
Loxapine overdose complicated by multiple seizures,
rhabdomyolysis, and acute renal failure has been reported. Mild overdoses only
result in drowsiness, lethargy and confusion. Parkinsonism, akathisia, dystonic
reactions, tardive dyski-nesia, choreoathetosis, cogwheel rigidity, tardive
myoclonus, and lingual dyskinesia have been described at therapeutic doses in
patients treated with loxapine and amoxapine.
o
With pimozide therapy, adverse effects occur in about 10 to
15% of patients and are dose related, occurring most frequently when the daily
dose exceeds 10 mg/ day. Hypotension, cardiac arrhythmias including QT
prolongation and torsade de pointes, extrapyramidal effects, anorexia, nausea,
diarrhoea or constipation, sedation, mydriasis, facial swelling, amenorrhoea
with galactorrhoea, xerostomia, anxiety, agitation, dysphoria, lethargy, and
depression may occur. Prolongation of the QT interval occurs commonly after an
overdose. Hypotension, cardiac arrhythmias including QT prolongation and
torsade de pointes, and seizures may occur following an overdose with pimozide.
Extrapyramidal and anticholinergic effects also occur following overdoses.
Diagnosis
·
Monitor acid-base status, fluid and
electrolyte balance, hepatic enzyme levels (serum ALP, SGOT, and SGPT), renal
function and urine output.
·
Patients with clinical signs of
neuroleptic malignant syndrome should be monitored for rising serum CPK levels
and leukocyte count.
·
Institute continuous cardiac
monitoring and follow serial ECGs.
·
Unabsorbed phenothiazines are
radiopaque in the gastroin-testinal tract, and the diagnosis of phenothiazine
ingestion can be made radiographically. Absence of radiopacity does not rule
out phenothiazine overdose.
·
Phenothiazines have been reported to
impart a pink to red, purple, orange, or rust colour to the urine. This change
in urine colour is variable among patients.![]()
Treatment
Neuroleptic malignant syndrome:
·
Discontinue neuroleptic therapy.
·
Management of hyperthermia by rapid external cooling with
ice. Do not use antipyretics; they are useless in this setting.
·
Dantrolene sodium, 1 to 3 mg/kg/day IV in 4 divided doses
(maximum 10 mg/kg/day). Maintenance dose (oral): 50 to 200 mg/day.
·
Bromocriptine, 2.5 to 10 mg orally, 3 times a day (maximum
20 mg, 4 times a day). Continue with dant-rolene or bromocriptine (rarely both
together), until patient’s condition improves, or until creatine kinase levels
return to normal. It is important to note that dantrolene or bromocriptine (or
even amantidine) may not produce immediate improvement, which usually takes 24
to 72 hours to be evident. Bromocriptine and amantidine act by inducing central
dopamine agonist effects, while dantrolene inhibits the release of calcium from
sarcoplasmic reticulum.
·
Pancuronium and sodium nitroprusside have been used with
success in some cases of neuroleptic malignant syndrome.
·
Supportive measures—correction of fluid and electro-lyte
imbalance, management of hypo/hypertension, maintaining pulmonary,
cardiovascular, and renal func-tions, and sedation.
·
Electroconvulsive therapy may be required in some cases.
Acute extrapyramidal syndromes:
Akathisia—
·
Reduce dose of neuroleptic drug.
·
Administer antiparkinsonian drugs or
benzodiaz-epines, or both.
·
Propranolol (20 to 50 mg daily) may
help to reduce hyperactivity associated with haloperidol.
Acute
dystonia—
·
Diphenhydramine, 1 to 2 mg/kg, IV, (maximum 100 mg), or benztropine mesylate, 1 to 2 mg, IV.
·
Maintenance: benztropine mesylate orally, 1 to 2 mg twice a
day, or trihexyphenidyl 2 mg three
times a day, or diphenhydramine 1
mg/kg (upto 50 mg), four times a day.
·
Parkinsonism—Administration of antiparkinsonian drugs,.
Chronic extrapyramidal syndromes:
·
Tardive dyskinesia—It is the most recalcitrant of the
adverse effects of neuroleptic medication, and once established is extremely
resistant to treatment. Therefore preventing this complication is more
impor-tant, which can be achieved by avoidance of high-dose, long-term daily
therapy as well as observing “drug holidays” i.e. periods of abstinence from
drugs.
·
![]() Treatment of tardive dyskinesia has
been attempted with a wide variety of drugs with little or no success. They
include the following: serotonergic drugs (tryptophan, cyproheptadine),
noradrenergic drugs (lithium), b-adrenergic receptor antagonists
(propranolol), and a-adrenergic agonists (cloni-dine).
Treatment of tardive dyskinesia has
been attempted with a wide variety of drugs with little or no success. They
include the following: serotonergic drugs (tryptophan, cyproheptadine),
noradrenergic drugs (lithium), b-adrenergic receptor antagonists
(propranolol), and a-adrenergic agonists (cloni-dine).
·
Newer approaches with morphine, naloxone, oestrogen,
pyridoxine, manganese, phenytoin, and papaverine have also not been
encouraging.
·
Anticholinergic agents usually aggravate existing tardive
dyskinesia, while cholinergic drugs are only marginally beneficial.
·
Benzodiazepines may give temporary relief, but sometimes
there is exacerbation.
Rabbit
syndrome—
·
Discontinue neuroleptic therapy.
·
Administer antiparkinsonian drugs.
Cardiovascular toxicity:
·
Arrhythmias can be managed effectively by temporary cardiac
pacing which should preferably last for 10 days, especially in patients who
have presented with ventricular tachycardia associated with AV block I or II.
Drugs such as quinidine, procainamide, disopyramide, and isoproterenol are
contraindicated. Lignocaine-like drugs are only sometimes effective. Lignocaine
is indicated in patients with frequent PVCs (greater than 5 per minute),
coupled, multifocal, or R on T phenom-enon associated with ingestion.
Cardioversion is often required for ventricular tachycardia, and is the initial
treatment for ventricular fibrillation, but the arrhyth-mias are often
resistant. A pacing wire may be the only effective treatment, especially if
atrioventricular block is present.
·
For torsade de pointes: Withdraw the causative agent.
Haemodynamically unstable patients require electrical cardioversion. Emergent
treatment with magnesium, isoproterenol, or atrial overdrive pacing is
indicated. Detect and correct underlying electrolyte abnormalities
(hypomagnesaemia, hypokalaemia, hypocalcaemia).
·
All patients with neuroleptic-induced cardiac toxicity
should be subjected to careful cardiac monitoring.
·
Hypotension usually responds to Trendelenberg posi-tion and
Ringer’s lactate. If vasopressors are considered necessary, a-adrenergic agonists such as noradrenaline are the drugs of
choice. Use of adrenaline in hypoten-sive patients who have overdosed on
neuroleptics is generally NOT recommended, since these drugs may reverse
adrenaline’s usual pressor action and aggra-vate hypotension. Because dopamine
is more easily administered and can often be instituted more readily, it is
recommended by some investigators as the agent of choice. According to them, if
hypotension does not respond to dopamine, an agent with more selec-tive alpha
agonist activity is a logical second choice (noradrenaline, metaraminol).
Gastrointestinal symptoms:
·
Patients who experience a severely
dry mouth should be advised to rinse their mouth frequently, and to chew gum
(preferably sugar-less) or candy. Over-indulgence of the latter can however
predispose to oral fungal infec-tions and dental caries.
·
Constipation can be managed with
stool softeners or laxatives.
Acute neuroleptic overdose:
·
Activated charcoal and stomach wash can help if the patient
is seen in a short time after the ingestion. Sustained-release formulations of
thioridazine, chlor-promazine, and possibly other phenothiazines may require
extended treatment. Whole bowel irrigation or extended administration of
activated charcoal may reduce absorption.
·
Stabilisation—intubation, assisted ventilation, IV line,
cardiac monitoring.
·
Decontamination—gastric lavage, activated charcoal.
·
Elimination enhancement – haemodialysis, haemoperfu-sion,
etc. do not appear to be beneficial. Plasmapheresis may be beneficial in haloperidol-induced
NMS.
·
Management of convulsions with diazepam or pheny-toin.
Seizures are a particular problem with dibenzo-xapines such as amoxapine and
loxapine. If seizures cannot be controlled with diazepam or lorazepam, or
recur, administer phenobarbitone. If phenobarbitone is ineffective, consider
propofol, barbiturate coma and/or neuromuscular paralysis with continuous EEG
moni-toring.
·
Management of hypotension: Fluid challenge is suffi-cient
for correction of hypotension in most patients. If it is not effective,
dopamine is recommended as the drug of choice. If hypotension does not respond
to dopamine, an agent with more selective alpha agonist activity is a logical
second choice (noradrenaline, metaraminol).
·
Cardiac monitoring: Since the phenothiazines produce
“quinidine-like” effects on the myocardium, quinidine, procainamide, and
disopyramide should be avoided. Lignocaine is usually effective for ventricular
arrhyth-mias. Sodium bicarbonate may also be effective in treating arrhythmias
and QRS widening. Cardioversion is often required for ventricular tachycardia,
and is the initial treatment for ventricular fibrillation, but the dysrhythmias
are often resistant. A pacing wire may be the only effective treatment,
especially if atrioventricular block is present. With reference to torsades des
pointes, haemodynamically unstable patients require electrical cardioversion.
Emergent treatment with magnesium, isoproterenol, or atrial overdrive pacing is
indicated.
·
Detect and correct underlying electrolyte abnormalities.
Management
of rhabdomyolysis:
·
Early aggressive fluid replacement is the mainstay of
therapy and may help prevent renal insufficiency.
·
Diuretics such as mannitol or furosemide may be needed to
maintain urine output. Urinary alkalinisa-tion is NOT routinely recommended.
·
Initial treatment should be directed towards controlling
acute metabolic disturbances such as hyperkalaemia, hyperthermia, and
hypovolaemia. Control seizures, agitation, and muscle contrac- tions.
·
Vigorous fluid replacement with 0.9% saline is necessary
even if there is no evidence of dehydra- tion. Hypovolaemia, increased
insensible losses, and third spacing of fluid commonly increase fluid
requirements. Strive to maintain a urine output of at least 2 to 3 ml/kg/hr. In
severe cases 500 ml of fluid per hour may be required for the first several
days. Monitor fluid input and urine output, plus insensible losses. Monitor for
evidence of fluid overload and compartment syndrome; monitor serum
electrolytes, CK, and renal function tests.
Related Topics