Chapter: Modern Medical Toxicology: Neurotoxic Poisons: Drugs Used in Psychiatry
Lithium - Anti-Manic Drugs
ANTI-MANIC DRUGS
Lithium
┬Ę
Lithium, the lightest of all metals is the drug of choice
even today (more than 50 years after its introduction) for the treat-ment of
manic-depressive psychosis i.e. bipolar affective disorder. It is also useful
as adjunctive therapy for depression, mania in children and young adults,
alcoholism, and as a prophylaxis for cluster headaches.
┬Ę
Lithium is a naturally occurring alkali metal, present in
the earthŌĆÖs crust at concentrations of 0.005%. Lithium is used in industry as a
coolant in nuclear reactor, in alkaline storage batteries, and in the
manufacture of alloys. Occupational toxicity is however uncommon. Lithium
bromide, lithium chloride, lithium hydroxide, and lithium silicate are
synthesised from lithium carbonate which acts as a chemical intermediate.
Toxicokinetics
┬Ę
Lithium is rapidly absorbed on oral
administration and peak levels are achieved in 2 to 4 hours. Soluble lithium
compounds are rapidly and completely absorbed from the gastrointestinal tract,
besides subcutaneous, intramuscular, and intraperitoneal areas.
┬Ę
The volume of distribution is 0.6
L/kg, and plasma protein binding is to the extent of only 10%. Lithium is
evenly distributed among the tissue compartments. Sustained release
formulations require 25 to 30 hours for complete distribution.
┬Ę
The therapeutic elimination
half-life is about 20 to 24 hours, and 95% of the drug is excreted by the
kidney of which 80% is reabsorbed, while the remaining 20% appears in the urine
unchanged.
Mode of Action
┬Ę
The exact mechanism of action is so
unclear that there have been innumerable theories propounded to explain the
therapeutic efficacy of lithium in bipolar disorders none of which have been
conclusively demonstrated to be correct.
┬Ę
The main premise is as follows:
since lithium crosses cell membranes by various methods including the sodium
pump, the sodium leak canal, a lithium-bicarbonate exchange, and the
sodium-lithium counter exchange system, it is believed that the chemical exerts
its therapeutic effect by substituting for sodium in these transmembranal ion
exchanges.
┬Ę
A monovalent cation, chemically
similar to Na+ and K+, lithium is thought to act by
o imperfect
substitution for other cations in ionic processes and
o alteration
of the critical microenvironment required for humoral or metabolic processes.
┬Ę
By these mechanisms in the CNS,
lithium affects nerve excitation, synaptic transmission and neuronal
metabolism.
Adverse Effects
Ō¢ĀŌ¢Ā Thirst, polyuria,
tremor (even at rest), acne, hypothy-roidism, impaired concentration, ataxia,
and dysarthria.
Ō¢ĀŌ¢Ā Less commonly there
may be alopecia, psoriasis of finger-nails, and restless legs syndrome.
Ō¢ĀŌ¢Ā Sudden cessation of
lithium treatment after a prolonged course can sometimes precipitate asthma.
Drug Interactions
┬Ę
Diuretics and NSAIDs (except
aspirin) reduce lithium excretion. Combination of these drugs increases the
steady-state plasma lithium concentration by 39 to 50%. Observation for toxicity
and frequent monitoring is recom- mended.
┬Ę
Synergistic effect is noted with
pancuronium and suxam- ethonium.
┬Ę
Combination with neuroleptics may
result in encephalitis. The effect of antidepressants in general may be
augmented by lithium.
┬Ę
Lithium is frequently combined with
haloperidol for acute manic episodes during the first and second week of treat-
ment. Irreversible neurological toxicity and brain damage have occurred in some
of these patients.
┬Ę
In a review of lithium drug
interactions, treatment of breakthrough depression with tricyclic
antidepressants in patients taking lithium was associated with worsening of
lithium-induced tremor. There were also case reports of extrapyramidal symptoms
and seizures with the combi-nation.
┬Ę
ACE inhibitors have been reported to
enhance the toxic effects of lithium. They increase the tubular reabsorption of
lithium.
┬Ę Thiazide diuretics also, via their action on distal tubules, cause sodium depletion with a subsequent decrease in lithium clearance; lithium toxicity is thus likely to result.
Clinical (Toxic) Features
┬Ę
There are 3 types of lithium poisoning:
o
Acute poisoning in patients not under lithium treatment:mild or moderately severe
manifestations.
o
Acute poisoning in patients under lithium treatment: severe
manifestations.
o
Chronic poisoning in patients under lithium treatment.
┬Ę
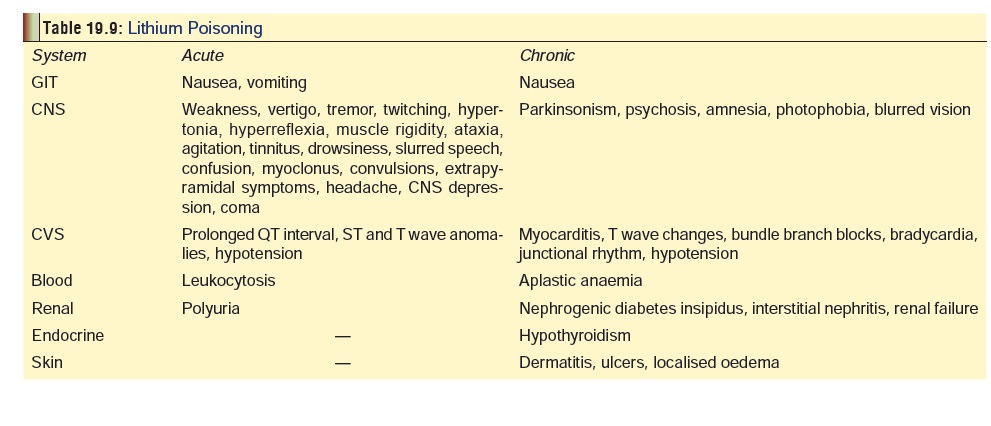
Table 19.9 lists the manifestations of lithium
toxicity.Nausea and vomiting are common effects. Headache can occur.
┬Ę
There are indications that lithium intake during preg-nancy
may be associated with cardiovascular and other congenital malformations.
Congenital malformations, including cardiac defects have been reported in
infants of mothers receiving lithium therapy in the first trimester.
┬Ę
Lithium toxicity may be one of the causes of Floppy babysyndrome.
┬Ę
In patients treated with lithium chronically, T wave
flat-tening is the most common EKG abnormality found in 20 to 100%, occurring
within 5 days of starting treatment and disappearing within 3 to 5 days after
discontinuing treatment. Sinus node dysfunction is the most frequently reported
conduction defect.
┬Ę
Hypercalcaemia and hyperkalaemia with cardiac rhythm
disturbances have been reported as a side effect of lithium treatment.
┬Ę
Neutrophilia is a reported side effect of treatment with
lithium, and significant leukocytosis may develop with lithium toxicity.
┬Ę
Tremor, hyperreflexia, ataxia, slurred speech, lethargy,
confusion, and cogwheel rigidity occur with mild to moderate intoxications.
Agitation is common. Seizures and coma may develop with severe poisoning. Fine
tremor of the hands is usually seen in 45 to 50% of patients starting lithium
therapy. Less than 10% of patients experience tremor after one year of therapy.
┬Ę Severe neurologic effects are much more common in patients with chronic poisoning than in those with acute overdose. Since lithium clears from the plasma much faster than from the brain, patients with chronic lithium toxicity may still have neurological toxicity when lithium levels have fallen into or below the therapeutic range.
┬Ę
Dehydration is a common finding in patients with chronic
lithium intoxication. Dehydration may precipi-tate chronic lithium toxicity
secondary to increased renal tubular resorption of lithium ion, and lithium
toxicity may cause dehydration secondary to nausea and vomiting, polyuria and
decreased water drinking from mental status changes.
┬Ę
Long-term lithium therapy has been shown to result in
decreased renal glomerular function. Nephrogenic diabetes insipidus and
resulting hypernatraemia may develop, particularly with chronic overdose. Acute
over-dose can lead to renal failure.
┬Ę
Only 1% of lithium therapy patients experience derma-tologic
effects. Acne, folliculitis, psoriasis, alopecia, cutaneous ulcers, xerosis
cutis, anaesthesia of the skin, and exfoliate dermatitis can all occur, which
usually resolve when therapy is discontinued.
┬Ę
Hypothyroidism has been associated with chronic lithium
intoxication. In systematic studies, the incidence has been consistently
elevated (10.4% of cases), espe-cially in females (14%) and in older
individuals. There is a substantially increased risk of hypothyroidism in
female patients age greater than 60, and in patients with a family history of
thyroid disease. The symptoms of GravesŌĆÖ disease may be masked by lithium
therapy.
Diagnosis
┬Ę
Blood lithium level (BLL): Toxicity
is associated with levels over 2 mEq/L. Death is likely if the BLL crosses 5
mEq/L. Therapeutic levels generally range from 0.6 to 1.2 mEq/L. However, serum
levels do not necessarily correlate with toxicity after acute ingestion.
┬Ę
Evidence of hypernatraemia,
hypocalcaemia, and hypopar-athyroidism.
┬Ę
Perform urinalysis and determine
serum creatinine to rule out impaired renal function.
Treatment
┬Ę Stabilisation: Maintenance of airway, breathing, andcirculation. Cardiac
monitoring is desirable. In the case of hypotension, infuse 10 to 20 ml/kg of
isotonic fluid and place in Trendelenburg position. If hypotension persists,
administer dopamine or noradrenaline. Consider central venous pressure monitoring
to guide further fluid therapy. For mild/moderate asymptomatic hypertension,
pharmacologic intervention is seldom necessary and 4 to 6 hours of observation
is usually adequate. For severe hypertension, use nitroprusside or esmolol.
┬Ę Decontamination : Activated charcoal is
ineffective.Stomach wash may help if the patient is seen early. Whole-bowel
irrigation with a balanced polyethylene-electrolyte solution (PEG-ELS) is said
to be quite beneficial. The recommended rates of administration are 2 L/hr
(adult), and 500 ml/hr (child). Bentonite has been shown to reduce lithium
absorption in vitro. In one study, bentonite reduced the lithium concentration
by 20.5% in deionised water (pH and by 48.1% in simulated gastric fluid (pH
1.2) at a bentonite lithium ratio of 30.1 (p value 0.0001).
┬Ę Elimination enhancement: Haemodialysis is indicated inthe
following situationsŌĆö
┬Ę
Severe intoxication with coma, convulsions, or respiratory
failure.
├ś Grade 3 coma.
┬Ę
Progressive deterioration.
┬Ę
Rising serum concentration.
├ś 4 mEq/L of serum concentration.
On
an average, 4 hours of haemodialysis will reduce plasma lithium concentration
by 1.0 mEq/L, and a total dialysis time of 10 to 12 hours may be required.
Lithium clearance during haemodialysis is approximately 100ŌĆō120 ml/min; thus
four hours of haemodialysis is equivalent to 24-hour clearance of 16ŌĆō20 ml/min.
Renal lithium clearance is 20 to 30% of creati-nine clearance; thus those with
renal impairment (calculated creatinine clearance less than 60 ml/min) are
generally good candidates for haemodialysis. Serum lithium levels should not be
considered a major criterion in acute intoxications. The deci-sion to institute
dialysis in acute intoxications should be based on a combination of clinical
toxicity, the duration of exposure, and a serial profile of serum lithium
levels.
However,
patients who have been dialysed sometimes develop a ŌĆ£reboundŌĆØ lithium level
after treatment because of subsequent leakage of intracellular lithium into the
plasma. Hence a repeat level should always be performed 6 hours post-dialysis,
and if this is high, a second round of dialysis may be needed.
┬Ę
If haemodialysis cannot be done, some investigators suggest
that sodium polystyrene sulfonate can be administered which is beneficial in
decreasing lithium absorption. It can however cause sodium overload and
hypokalaemia.
┬Ę
Recent studies indicate that continuous arteriovenous
haemodiafiltration (CAVH) can be very effective in lithium poisoning.
Successful use of veno- venous filtration has also been reported in some
isolated case reports.![]()
Related Topics