Chapter: Medical Surgical Nursing: Assessment and Management of Female Physiologic Processes
Menopause - Management of Normal and Altered Female Physiologic Processes
MENOPAUSE
Menopause
is the permanent physiologic cessation of menses as-sociated with declining
ovarian function; during this time, re-productive function diminishes and ends.
Postmenopause is the period beginning from about 1 year after menses cease.
Menopause is associated with some atrophy of breast tissue and genital organs,
loss in bone density, and vascular changes.
Menopause
starts gradually and is usually signaled by changes in menstruation. The
monthly flow may increase, decrease, be-come irregular, and finally cease.
Often, the interval between pe-riods is longer; a lapse of several months
between periods is not uncommon.
Changes
signaling menopause begin to occur as early as the late 30s, when ovulation
occurs less frequently, estrogen levels fluctuate, and FSH levels rise in an
attempt to stimulate estrogen production.
Clinical Manifestations
Because
of these hormonal changes, some women notice irregu-lar menses, breast
tenderness, and mood changes long before menopause occurs. The hot or warm
flashes and night sweats re-ported by some women are directly attributable to
hormonal changes. Hot flashes, which denote vasomotor instability, may vary in
intensity from a barely perceptible warm feeling to a sen-sation of extreme
warmth accompanied by profuse sweating, causing discomfort, sleep disturbances
and subsequent fatigue, and embarrassment.
Other
physical changes may include atrophic changes and osteoporosis (decreased bone density), resulting in
decreasedstature and bone fractures. About 1.5 million new fractures due to
osteoporosis occur yearly in the United States (NIH Consen-sus Statement,
2001). The entire genitourinary system is affected by the reduced estrogen
level. Changes in the vulvovaginal area may include a gradual thinning of pubic
hair and a slow shrinkage of the labia. Vaginal secretions decrease, and the woman
may report dyspareunia (discomfort during intercourse). The vaginal pH rises
during menopause, predisposing the woman to bacterial infections (atrophic
vaginitis). Discharge, itching, and vulvar burning may result.
Some
women report fatigue, dizziness, forgetfulness, weight gain, irritability,
trouble sleeping, feeling “blue,” and feelings of panic. Menopausal complaints
need to be evaluated carefully as they may indicate other disorders.
Psychological Considerations
Women’s
reactions and feelings related to loss of reproductive capacity may vary
(Jacob’s Institute of Women’s Health, 2000). For women with grown families,
menopause may result in role confusion or feelings of sexual and personal
freedom. Women may be relieved that the childbearing phase of their lives is
over. Each woman’s circumstances will affect her response and must be
considered on an individual basis. Nurses need to be aware of and sensitive to
all possibilities and take their cues from the patient.
Medical Management
As
stated earlier, menopause may be characterized by decreased vaginal secretions,
hot flashes, changes in the urinary tract, and mood swings. Decreased vaginal
lubrication may cause dyspareu-nia in the menopausal woman; this may be
prevented by the use of a water-soluble lubricant (eg, K-Y jelly, Replens,
Astro-Glide, or contraceptive foam or jelly). A vaginal cream containing
estro-gen or an estrogen-containing vaginal ring may be prescribed.
Women
approaching menopause often have many concerns about their health. Some have
concerns based on a family history of heart disease, osteoporosis, or breast
cancer. Each woman should discuss her concerns and feelings with her primary
health care provider so that she can make an informed decision about managing
menopausal symptoms and maintaining her health.
PHARMACOLOGIC THERAPY
Hormone Replacement Therapy.
HRT reduces
or eliminates per-sistent and severe hot flashes, reduces bone loss, decreases
the risk for colon cancer, and improves lipoproteins and lowers fibrino-gen levels
(Hulley, Grady, Bush, et al., 1998). Despite these find-ings, the more recent
Women’s Health Initiative controlled trial of HRT in over 16,600 women
demonstrated that the risks of HRT outweigh the benefits (Writing Group of the
Women’s Health Initiative Investigators, 2002). This study was halted after 5.2
years rather than continuing it for the planned duration of 8.5 years because women
receiving HRT had a higher risk for in-vasive breast cancer than the group
receiving placebo. Although the absolute risk of breast cancer is low for an
individual woman taking HRT, the risks were considered contrary to its intended
effect, which is to preserve health and prevent disease. Because of these
findings, many women have elected to discontinue HRT, and many of those who
previously would have taken HRT have refused or are reluctant to consider it.
Some women and their health care providers have elected to begin or continue
use of HRT to treat menopausal symptoms because of its benefits. Nurses need to
be knowledgeable about the issues associated with HRT use if they are to
provide appropriate health care to peri-menopausal and menopausal women.
Risks and Benefits of HRT.
The changes
that occur during meno-pause have adverse effects on women, placing them at
increased risk for atherosclerosis, angina, and coronary artery disease. The
effectiveness of HRT in reducing the risk for some of these con-ditions has not
been supported, and the American Heart Associ-ation has recommended against
initiating HRT for primary and secondary prevention of cardiovascular disease
or stroke (American Heart Association, 2002). HRT is contraindicated in women
with a history of breast cancer, vascular thrombosis, active liver disease or
chronically impaired liver function, some cases of uterine cancer, and
undiagnosed abnormal vaginal bleeding. The risk of thromboembolic phenomena is
slightly elevated. Women who elect to take HRT despite these risks should be
taught the signs and symptoms of deep vein thrombosis and pulmonary embolism and
should be instructed to report these signs and symptoms im-mediately. Nurses
should assess for leg redness, tenderness, chest pain, and shortness of breath
in patients who take HRT. Further, women taking HRT need to be informed about
the need for follow-up and monitoring. For women who decide to take HRT,
regular follow-up care, including a yearly physical examination and mammogram,
is important. An endometrial biopsy is indi-cated for women with any irregular
bleeding during treatment. Because the risk of complications increases the
longer HRT is used, HRT should be used for the shortest time necessary
(American Heart Association, 2002).
Making a Decision About HRT.
The decision
of whether to useHRT has been a difficult one for many women. Although the re-sults
of the Women’s Health Initiative trial may make the deci-sion easier for some
women, it is likely to remain a difficult decision for those who may benefit
from its use because of very disruptive symptoms of menopause and evidence of
bone loss. Women often want to learn about alternatives to HRT use; there-fore,
nurses should address other strategies that women can use to promote their
health in the perimenopausal period.
Method of HRT Administration.
There are
several different ap-proaches for use of hormone replacement. Some women take
both estrogen and progestin daily; others take estrogen for 25 consecu-tive
days each month, with progestin taken in cycles (eg, 10 to 14 days of the
month). Progestin is taken to prevent proliferation of the uterine lining and
hyperplasia in women who have not had their uterus removed. Women who take
hormones for 25 days often experience bleeding after completing the progestin.
Other women take estrogen and progesterone every day and usually ex-perience no
bleeding. They occasionally have irregular spotting, which should be evaluated
by their health care provider.
Estrogen
patches, which are replaced once or twice weekly, are another option but
require a progestin along with them if the woman still has a uterus. Vaginal
treatment with an estrogen cream, suppository, or an estradiol vaginal ring
(Estring) may be used for vaginal dryness or atrophic vaginitis. Estring is a
small, flexible vaginal ring that slowly releases estrogen in small doses over
3 months.
Alternatives to HRT.
Women may
benefit from learning aboutalternatives to HRT, including diet, vitamins, and
exercise. They need to know that these approaches to menopause have not been
examined thoroughly through research. Osteoporosis, a disease characterized by
low bone mass and microarchitectural deterioration of bone tissue, occurs with menopause
and leads to en-hanced bone fragility and increased risk for fracture. Other
fac-tors that increase a woman’s risk for osteoporosis include a thin body
frame, race (Caucasian or Asian), family history of osteo-porosis, nulliparity,
early menopause, moderate to heavy alcohol ingestion, smoking, caffeine use,
sedentary lifestyle, and a diet low in calcium. Women should be advised to
remain active or to begin an exercise program of weight-bearing activity, such
as walking; to take a calcium supplement; to decrease or stop smok-ing; and to
discuss the use of pharmacologic agents (bisphospho-nates, calcitonin,
parathyroid hormone, HRT) to reduce bone loss with their health care provider
(NIH Consensus Statement, 2001; National Osteoporosis Foundation, 1999).
Selective es-trogen receptor modulators (SERMs) such as raloxifene (Evista)
provide another alternative to HRT for the prevention and treat-ment of
osteoporosis. These medications do not appear to in-crease the risk for breast
cancer; indeed, the risk of breast and uterine cancer may be reduced. Their use
may increase hot flashes. No long-term studies exist on these medications
because of their recent development.
Problematic
hot flashes have been treated with venlafaxine (Effexor), paroxetine (Paxil),
gabapentin (Neurontin), and cloni-dine (Catapres). These medications have been
found to reduce hot flashes and are alternatives for women who do not wish to
use HRT. The web site of the North American Menopause Society
(http://www.menopause.org) provides additional suggestions.
Vitamin
B in doses of less than 200 mg has been found to relieve some distressing
menopausal symptoms. Vitamin E has been ef-fective in decreasing hot flashes
for many women. Some women are interested in alternative treatments (eg,
natural estrogens and progestins, black cohosh, ginseng, dong quai, soy
products, and several other herbal preparations); however, few scientific data
exist about the safety or effectiveness of these remedies. Assessment of
menopausal patients should include their use of complementary and alternative
therapies and supplements. Medications, including alendronate (Fosamax),
raloxifene (Evista), and calcitonin, for the treatment of osteoporosis have
given women another option in pre-venting or treating this major health
problem.
The
American Heart Association (2002) suggests the use of established methods of
treatment to lower heart disease risk in women. These include lifestyle changes
and behavioral strate-gies. Pharmacologic therapy (eg, aspirin, beta blockers,
statins, angiostatin-converting enzyme inhibitors) may be indicated in women
who have cardiovascular disease or are at high risk for it.
BEHAVIORAL STRATEGIES
Regular
physical exercise, including weight-bearing exercise, raises the heart rate,
increases high-density lipoprotein (HDL) levels, and helps to maintain bone
mass. It may also reduce stress, enhance well-being, and improve self-image.
Loss of muscle tis-sue is mediated by exercise; weight-bearing exercise (eg,
walking, jogging) at least four times a week is recommended.
NUTRITIONAL THERAPY
Women
should also be encouraged to decrease caloric intake, de-crease fat intake, and
increase intake of whole grains, fiber, fruit, and vegetables. Women of all
ages are urged to include high-calcium food in their diets daily. For example,
1 cup of milk contains about 300 mg of calcium, and 1 cup of nonfat yogurt
provides 415 mg of calcium.
Other sources of dietary calcium include most green leafy vegetables, seafood,
and calcium-fortified foods.
Calcium
supplementation may be helpful in reducing bone loss and preventing the
morbidity associated with fractures sec-ondary to osteoporosis. Bones serve as
a storehouse of the body’s calcium, and bone density decreases with age. When
calcium levels in the blood are low, the bones give up calcium to main-tain
homeostasis. Women of all age groups often ingest less than the recommended
amount of calcium. The average calcium in-take is 300 to 500 mg/day, whereas
the recommended amount is 1,300 mg/day for adolescents and young adults, 1,000
mg/day for adults 19 to 50 years of age, 1,200 mg/day for adults 51 years of
age and older (including menopausal women taking HRT), and 1,500 mg/day for
women who are menopausal and not taking HRT (National Osteoporosis Foundation,
1999; NIH Consen-sus Statement, 2001).
Nursing Management
Nurses
can encourage women to view menopause as a natural change resulting in freedom
from menses and symptoms related to hormonal changes. No relationship exists
between menopause and mental health problems; however, social circumstances
(eg, adolescent children, ill partners, and dependent or ill par-ents) that
usually coincide with menopause may produce stress.
Measures
should be taken to promote general health. The nurse can explain to the patient
that cessation of menses is a phys-iologic function that is rarely accompanied
by nervous symptoms or illness. The current expected life span after menopause
for the average woman is 30 to 35 years, which may encompass as many years as
the childbearing phase of her life. Menopause is not a complete change of life,
however. Normal sexual urges continue, and women retain their usual response to
sex long after meno-pause. Many women enjoy better health after menopause than
before, especially those who have experienced dysmenorrhea. The individual
woman’s evaluation of herself and her worth, now and in the future, is likely
to affect her emotional reaction to meno-pause. Patient teaching and counseling
regarding healthy lifestyles, health promotion, and health screening are of
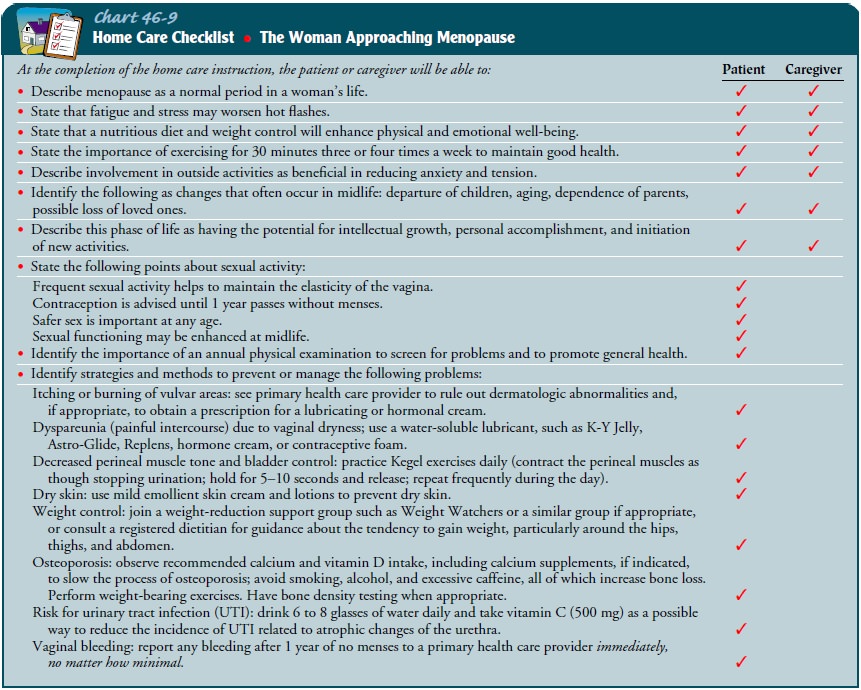
paramount im-portance (Chart 46-9).
Related Topics