Chapter: Medical Surgical Nursing: Assessment and Management of Female Physiologic Processes
Cytologic Test for Cancer (Pap Smear) - Diagnostic Evaluation of Female Physiologic Processes
Diagnostic Evaluation
CYTOLOGIC
TEST FOR CANCER (PAP SMEAR)
The Pap
smear is performed to detect cervical cancer. Before 1940, cervical cancer was
the most common cause of cancer death in women. Dr. George Papanicolaou
discovered the value of ex-amining exfoliated cells for malignancy in the
1930s. Due to the effectiveness of the Pap smear as a screening method,
cervical can-cer is now less common than breast or ovarian cancer.
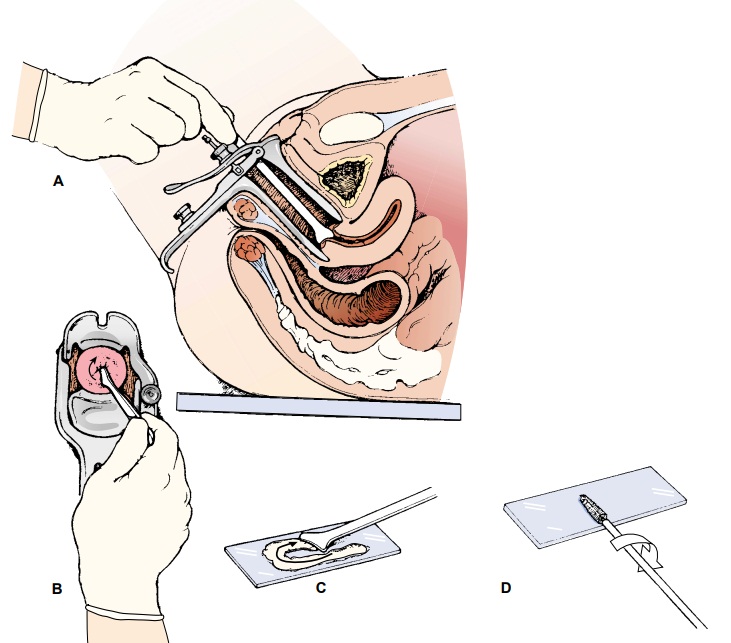
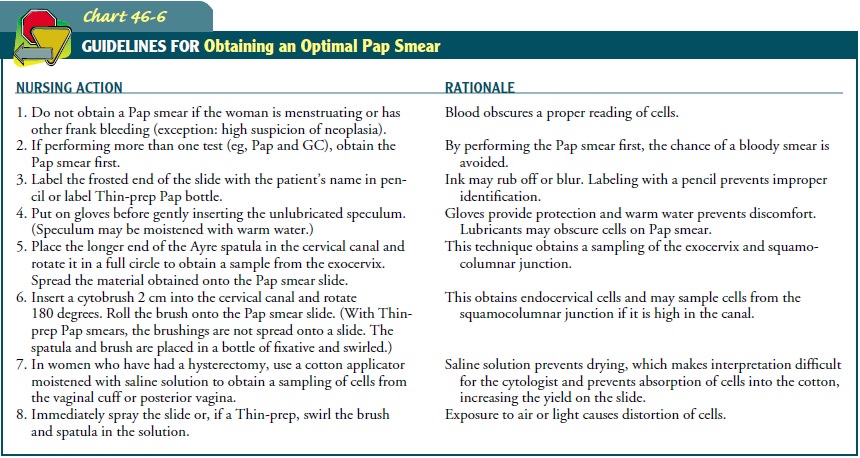
Cervical
secretions are gently removed from the cervical os (Fig. 46-6), transferred to
a glass slide, and fixed immediately by spraying with a fixative. A Thin-prep
Pap specimen is immersed in a solution rather than being placed on a slide.
This method al-lows for human papillomavirus (HPV) testing if the Pap smear
result is abnormal.
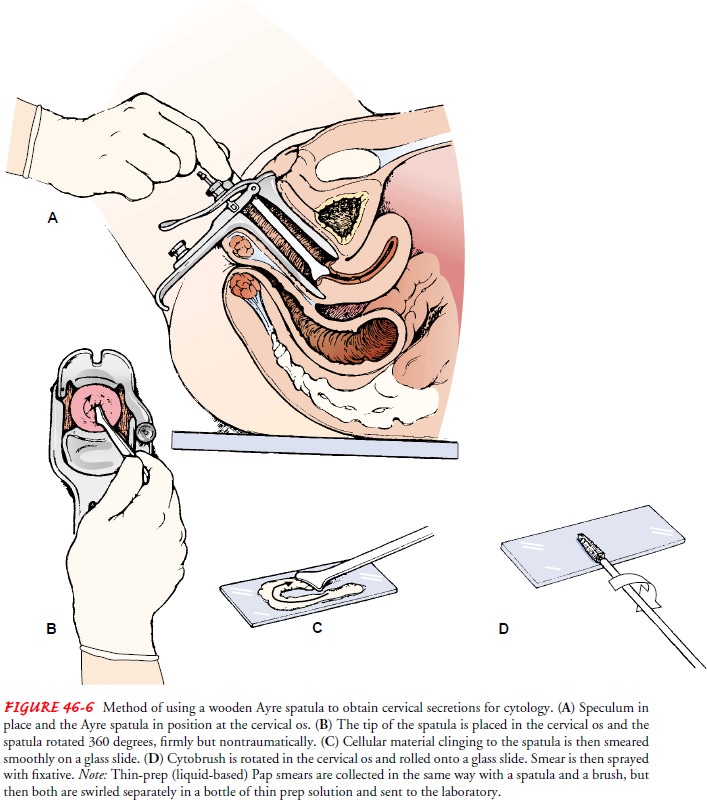
The
patient should be instructed not to douche before this ex-amination to avoid
washing away cellular material. The Pap smear should be performed when the
patient is not menstruating because blood usually interferes with
interpretation. The proper technique for obtaining a cervical specimen for
cytologic study is described in Chart 46-6. False-negative Pap smear results
may occur, as may false positives.
The
Bethesda Classification system (Chart 46-7) has been de-veloped to promote
consistency in reporting Pap smear results and to assist in standardizing
management guidelines (Solomon, Davey, Kurman et al., 2001). Terminology
includes the follow-ing categories:
·
Low-grade squamous intraepithelial lesion (LSIL),
which is equivalent to cervical intraepithelial neoplasia (CIN 1) and to mild
changes related to exposure to HPV
· High-grade squamous
intraepithelial lesions (HSIL), which equates to moderate and severe dysplasia,
carcinoma in situ (CIS), and CIN 2 and CIN 3
These
terms seen on Pap smear findings encompass the pre-cursors to invasive
carcinoma of the cervix.
Pap
smears that reveal mild inflammation or atypical squamous cells are usually
repeated in 3 to 6 months, with findings often re-turning to normal. Patients
are apprehensive because many women incorrectly assume that an abnormal Pap
smear means cancer. If a specific infection is causing inflammation, it is
treated appropri-ately, and the Pap smear is repeated. If the repeat Pap smear
reveals atypical squamous cells, then a colposcopy is appropriate.
Thin-prep
Pap specimens that show atypical cells can also be used to determine the
presence of HPV DNA. If HPV DNA is present, it is more likely that HSIL is
present.
If the
Pap smear results are abnormal, prompt notification, evaluation, and treatment
are crucial. Notification of patients is often done by nurses in women’s health
care. Pap smear follow-up is crucial as it can prevent cervical cancer. Many
women do not adhere to recommendations—particularly young women, those of low
socioeconomic status, minorities, women who have difficulty coping with the diagnosis,
and those without social sup-port. Fear, lack of understanding, and childcare
responsibilities have all been identified by women as reasons for poor
follow-up. Women with a history of abuse, obese women, and women who had a
negative gynecologic experience may also find returning for follow-up difficult
(Wee, McCarthy, Davis & Phillips, 2000). Interventions are tailored to meet
the needs of the particular group. Intensive telephone counseling, tracking
systems, brochures, videos, and financial incentives have all been used to
encourage follow-up. Nurses can provide clear explanations and emotional
support along with a carefully designed follow-up protocol designed to meet the
needs of their specific patient population (DeRemer Abercrombie, 2001).
Related Topics