Chapter: Medical Surgical Nursing: Assessment and Management of Female Physiologic Processes
Abortion - Management of Normal and Altered Female Reproductive Function
ABORTION
Interruption
of pregnancy or expulsion of the product of con-ception before the fetus is
viable is called abortion. The fetus is generally considered to be viable any
time after the fifth to sixth month of gestation. The term “premature labor” is
used when a woman experiences labor after this point in the pregnancy.
Spontaneous Abortion
It is
estimated that 1 of every 5 to 10 conceptions results in spon-taneous abortion.
Most of these occur because an abnormality in the fetus makes survival
impossible. Other causes may include systemic diseases, hormonal imbalance, or
anatomic abnormali-ties. If a pregnant woman experiences bleeding and cramping,
a threatened abortion is diagnosed because an actual abortion is usually
imminent. Spontaneous abortion occurs most commonly in the second or third
month of gestation.
There
are various kinds of spontaneous abortion, depending on the nature of the process
(threatened, inevitable, incomplete, or complete). In a threatened abortion,
the cervix does not dilate. With bed rest and conservative treatment, the
abortion may be prevented. If it cannot, an abortion is imminent. If only some
of the tissue is passed, the abortion is referred to as incomplete. If the
fetus and all related tissue are spontaneously evacuated, the abortion is
complete.
HABITUAL ABORTION
Habitual
or recurrent abortion is defined as successive, repeated, spontaneous abortions
of unknown cause. As many as 60% of abortions may result from chromosomal
anomalies. After two consecutive abortions, patients are referred for genetic
counseling and testing, and other possible causes are explored. If bleeding
oc-curs in these patients, conservative measures, such as bed rest and
administering progesterone to support the endometrium, are tried in an attempt
to save the pregnancy. Supportive counseling is crucial in this stressful
condition. Bed rest, sexual abstinence, a light diet, and no straining on
defecation are recommended in an effort to prevent spontaneous abortion. If
infection is suspected, antibiotics may be prescribed.
In the
condition known as incompetent or dysfunctional cervix, the cervix dilates
painlessly in the second trimester of pregnancy, often resulting in a
spontaneous abortion. In such cases, a surgi-cal procedure called cervical
cerclage may be used to prevent the cervix from dilating prematurely. The
procedure involves placing a purse-string suture around the cervix at the level
of the internal os. Bed rest is usually advised to keep the weight of the
uterus off the cervix.
The
patient and her health care providers must be informed that such a suture is in
place in this high-risk pregnancy. About 2 to 3 weeks before term or the onset
of labor, the suture is cut. Delivery is usually by cesarean section.
MEDICAL MANAGEMENT
After
a spontaneous abortion, all tissue passed vaginally is saved for examination.
The patient and all personnel caring for her are alerted to save any discharged
material. In the rare case of heavy bleeding, the patient may require blood
component transfusions and fluid replacement. An estimate of the bleeding
volume can be determined by recording the number of perineal pads and the
degree of saturation over 24 hours. When an incomplete abor-tion occurs,
oxytocin may be prescribed to cause uterine con-tractions before dilation and
evacuation (D & E) or uterine suctioning.
NURSING MANAGEMENT
Because
patients experience loss and anxiety, emotional support and understanding are
important aspects of nursing care. The response of the woman who desperately
wants a baby is very dif-ferent from that of the woman who does not want to be
preg-nant but may be frightened by the possible consequences of an abortion.
The
nurse must be aware that the woman having a sponta-neous abortion often
experiences a grieving period. The grieving may be delayed and may cause other
problems until resolved. The many reasons for a delayed grief reaction include
the following: friends may not have known the woman was pregnant; the woman may
not have seen the lost fetus and can only imagine the gender, size, and
characteristics of the child who never developed; there is usually no burial
service; and those who know about the loss (fam-ily, friends, caregivers) may
encourage denial by rarely talking about the loss or by discouraging the woman
from crying.
Providing
opportunities for the patient to talk and express her emotions helps and also
provides clues for the nurse in planning more specific care. Those closest to
the woman are encouraged to give emotional support and to allow her to talk and
freely express her grief. Unresolved grief may manifest itself in persistent
vivid memories of the events surrounding the loss, persistent sadness or anger,
and episodes of overwhelming emotion when recalling the loss. Dysfunctional
grief may require the assistance of a skilled therapist.
Elective Abortion
A
voluntary induced termination of pregnancy is called an elective abortion and
is usually performed by skilled health care providers. In 1973, the U.S.
Supreme Court in Roe v. Wade ruled that de-cisions about abortion reside with a
woman and her physician in the first trimester. During the second trimester,
the state may reg-ulate practice in the interest of a woman’s health and during
the final weeks of pregnancy may choose to protect the life of the fetus,
except when necessary to preserve the life or health of the woman.Legislation
has been passed to increase access to abortion clinics and to prevent violence
toward those who work in such facilities.
The
rate of abortion, steady from 1980 to 1990, decreased 15% from 1990 to 1995.
Rates since then have been the lowest since 1975 (Zapka, Lemon, Peerson et al.,
2001). However, the rate has increased among the following groups of females:
un-married Caucasian girls under age 15, unmarried non-Caucasian girls ages 15
to 19, and married non-Caucasian women ages 20 to 24. The U.S. rates of
abortion are among the highest in the industrialized Western world. These
numbers point out the need for nurses to provide contraceptive education and
counseling. Elective abortions may be carried out in many different ways (Chart
46-16).
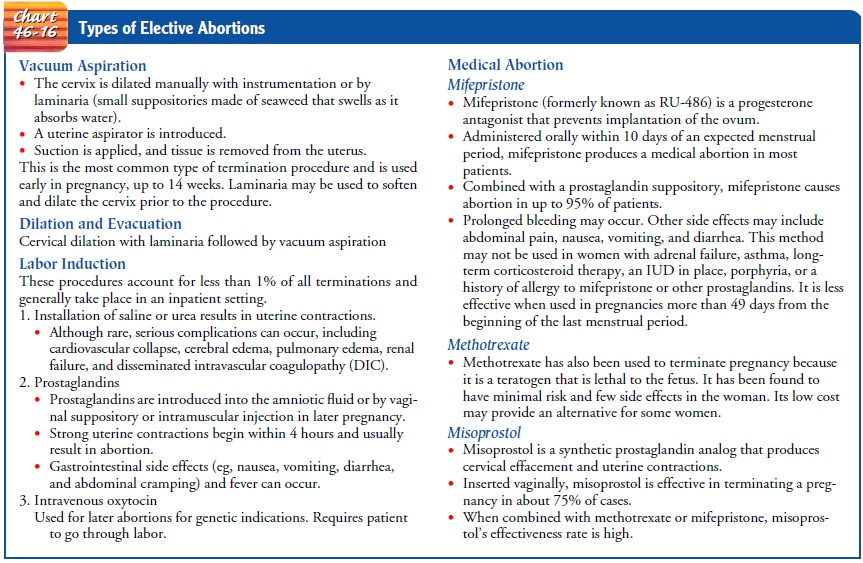
MEDICAL MANAGEMENT
Before the procedure is performed, a nurse or counselor trained in pregnancy counseling explores with the patient her fears, feelings, and options. After the patient’s choice is identified (ie, continuing pregnancy and parenthood; continuing pregnancy followed by adoption; or terminating pregnancy by abortion), a pelvic exami-nation is performed to determine uterine size. Laboratory studies before an abortion must include a pregnancy test to confirm the pregnancy, hematocrit to rule out anemia, Rh determination, and an STD screen. A patient with anemia may need an iron supple-ment, and an Rh-negative patient may require RhoGAM to pre-vent isoimmunization. Before the procedure, all patients should be screened for STDs to prevent introducing pathogens upward through the cervix during the procedure.
NURSING MANAGEMENT
Patient
teaching is an important aspect of care for women who elect to terminate a
pregnancy. A woman undergoing elective abortion is informed about what the
procedure entails and the ex-pected course after the procedure. The patient is
scheduled for a follow-up appointment 2 weeks after the procedure and is
in-structed in recognizing and reporting signs and symptoms of complications
(ie, fever, heavy bleeding, or pain).
Available
contraceptive methods are reviewed with the patient at this time. Effectiveness
depends on the method used and the extent to which the woman and her partner
follow the instruc-tions for use. The woman who has used any method of birth
con-trol should be assessed for her understanding of the method and its
potential side effects and her satisfaction with the method. If the patient was
not using contraception, the nurse explains all methods and their benefits and
risks and assists the patient in making a contraceptive choice for use after
abortion. An increas-ingly important related teaching issue is the need to use
barrier contraceptive devices (ie, condoms) for protection against
trans-mission of STDs and HIV infection.
Psychological
support is another important aspect of nursing care. Nurses need to be aware
that women terminate pregnancies for many reasons. Some women terminate
pregnancies because of severe genetic defects. Many women who have been raped
or impregnated in incestuous relationships or by an abusive partner elect to
terminate their pregnancies. Infertility patients may elect to undergo
selective termination if they become pregnant with multiple fetuses. In
pregnancies with multiple gestation, adverse outcomes are directly proportional
to the number of fetuses in the uterus. Such multifetal reductions are
specialized procedures that are stressful and difficult for the parents;
therefore, psychological support and understanding are required. The care of
women un-dergoing termination of pregnancy is stressful, and assistance needs to
be provided in a safe and nonjudgmental way. Nurses have the right to refuse to
participate in a procedure that is against their religious beliefs but are
professionally obligated not to im-pose their beliefs or judgments on their
patients.
Patients
may opt for a type of abortion that ends a pregnancy by using medication rather
than surgery. Mifepristone (RU-486, Mifeprex) is used only in early pregnancy
(up to 49 days from the last menstrual period). It works by blocking
progesterone. Cramping and bleeding similar to a heavy menstrual period will
occur. This method requires three visits to a health care provider. The first
visit consists of counseling and consent. A sonogram may be used to confirm the
pregnancy. Mifepristone will then be administered. The second visit consists of
a pelvic examination and possible sonogram to check if the pregnancy has been
termi-nated. A third visit 12 days later is to make sure that the pelvic
examination is normal and that the pregnancy has been terminated. If the pregnancy
persists, options will be discussed, in-cluding surgical abortion (ACOG
Practice Bulletin #26, 2001).
Infertility
Infertility
is defined as a couple’s inability to achieve pregnancy after 1 year of
unprotected intercourse. Primary infertility refers to a couple who has never
had a child. Secondary infertility means that at least one conception has
occurred, but currently the cou-ple cannot achieve a pregnancy. In the United
States, infertility is a major medical and social problem, affecting 10% to 15%
of the reproductive-age population. In 20%, the infertility is unex-plained.
The remaining 80% involve medical causes equally dis-tributed between men and
women (ACOG Technical Bulletin #125, 2001; Compendium,
2000). Women’s infertility may be related to anovulation, uterine or cervical
factors, blocked fallo-pian tubes, or endometriosis, while men’s infertility is
related to sperm quality or sperm production. For infertile women who wish to
bear children, infertility may have a profound emotional toll (Gonzalez, 2000;
Hart, 2002).
Pathophysiology
Possible
causes of infertility include uterine displacement by tumors, congenital
anomalies, and inflammation. For an ovum to become fertilized, the vagina,
fallopian tubes, cervix, and uterus must be patent and the mucosal secretions
of the cervix must be receptive to sperm. Semen and cervical secretions are
alkaline, whereas normal vaginal secretions are acidic. Often more than one
factor is responsible for the problem. Identify-ing the causes may require the
services of a gynecologist, urolo-gist, and endocrinologist.
Assessment and Diagnostic Findings
Careful
evaluation includes physical examination, endocrinologic investigation, and
consideration of psychosocial factors. Three complete histories (one of each
partner and one of the couple), physical examination, and laboratory studies
are performed on both partners to rule out such causative factors as previous
STDs, anomalies, injuries, tuberculosis, mumps orchitis, impaired sperm
production, endometriosis, DES exposure, or antisperm anti-bodies. Five factors
are considered basic to infertility: ovarian, tubal, cervical, uterine, and
semen conditions.
OVARIAN FACTORS
Studies
performed to determine if there is regular ovulation and if progestational
endometrium is adequate for implantation may in-clude a basal body temperature
chart for at least four cycles, an en-dometrial biopsy, serum progesterone
level, and ovulation index. The ovulation index involves a urine-stick test
that determines if the surge in LH that precedes follicular rupture has
occurred.
TUBAL FACTORS
Hysterosalpingography
is used to rule out uterine or tubal ab-normalities. Laparoscopy permits direct
visualization of the tubes and other pelvic structures and can assist in
identifying condi-tions that may interfere with fertility (eg, endometriosis).
CERVICAL FACTORS
The
cervical mucus can be examined at ovulation and after in-tercourse to determine
whether proper changes occur that pro-mote sperm penetration and survival. A
postcoital cervical mucus test (Sims-Huhner test) is performed 2 to 8 hours
after inter-course. Cervical mucus is aspirated with a medicine dropper–like
instrument. Aspirated material is placed on a slide and examined under the
microscope for the presence and viability of sperm cells. The woman is
instructed not to bathe or douche between coitus and the examination.
UTERINE FACTORS
Fibroids,
polyps, and congenital malformations are possible con-ditions in this category.
Their presence may be determined by pelvic examination, hysteroscopy, saline
sonogram (a variation of a sonogram), and hysterosalpingography.
SEMEN FACTORS
After
2 to 3 days of sexual abstinence, a specimen of ejaculate is collected in a
clean container, kept warm, and examined within 1 hour for the number of sperm
(density), percentage of moving forms, quality of forward movement (forward
progression), and morphology (shape and form). From 2 to 6 mL of watery
alkaline semen is normal; a normal count is 60 million to 100 million sperm/mL,
although the incidence of impregnation is lessened only when the count drops
below 20 million sperm/mL. A nor-mal semen analysis should show the following
(Angard, 1999):
· Volume: more than 1 mL
· Concentration: more than
20 million/mL
· Motility: more than 50%
of the forms should be moving
· Morphology: more than
60% of sperm should have normal forms
· No sperm clumping,
significant red or white blood cells, or thickening of seminal fluid
(hyperviscosity)
MISCELLANEOUS FACTORS
Men
may also be affected by varicoceles, varicose veins around the testicle, which
decrease semen quality by increasing testicular temperature. Retrograde
ejaculation or ejaculation into the blad-der is assessed by urinalysis after ejaculation.
Blood
tests for male partners may include measuring testos-terone; FSH and LH (both
of which are involved in maintaining testicular function); and prolactin levels
and antisperm antibod-ies (treated with corticosteroids).
Immunologic
factors also are being investigated. Some cases of recurrent early pregnancy
loss or recurrent natural abortion are the result of an abnormal response by
the woman to antigens on fetal or placental tissues. Some women have been
treated with infusions of their partner’s lymphocytes with some success, but
this treatment remains experimental and the long-term effects are unknown.
Medical Management
Infertility
is often difficult to treat because it frequently results from a combination of
factors. Couples undergoing an infertility evaluation may conceive without the
cause of infertility ever iden-tified. Likewise, although some couples undergo
all tests, the cause of the problem may remain undiscovered and infertility
persists. Between these extremes, many problems, both simple and complex, can
be discovered and corrected. Patients may need assisted reproductive technology
to conceive; the methods are de-scribed below. Therapy may require surgery to
correct a mal-function or anomaly, hormonal supplements, attention to proper
timing, and recognition and correction of psychological or emo-tional factors.
PHARMACOLOGIC THERAPY
Pharmacologically
induced ovulation is undertaken when women do not ovulate on their own or
ovulate irregularly. Various med-ications are used, depending on the primary
cause of infertility (Chart 46-17). Clomiphene citrate (Clomid) is the most
com-mon medication used. Although Clomid’s precise action is un-known, it
enhances the release of pituitary gonadotropins, resulting in follicular
rupture or ovulation.
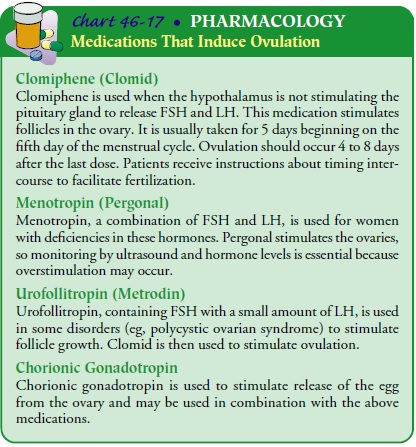
Another
mode of pharmacotherapy for anovulatory women includes the use of pulsatile
gonadotropin-releasing hormone (GnRH). The woman wears an infusion pump
attached to an in-travenous or subcutaneous catheter for up to 21 days.
Adminis-tration of GnRH can result in ovulation in some women with low hormone
levels. This option can reduce cycle monitoring and the incidence of multiple
gestation (ACOG Technical Bulletin #197,
ACOG Compendium, 2001).
Human
menopausal gonadotropin may also be used as it stim-ulates the ovaries to
produce eggs. Blood tests and ultrasounds are used to monitor ovulation.
Multiple pregnancies may occur with these medications. Ovarian hyperstimulation
syndrome (OHSS) may also occur. This condition is characterized by enlarged
mul-ticystic ovaries and is complicated by a shift of fluid from the
intra-vascular space into the abdominal cavity. It is iatrogenic and
preventable and develops after ovarian stimulation. The fluid shift can result
in ascites, pleural effusion, and edema; hypo-volemia may also result. Risk
factors include younger age, history of polycystic ovarian syndrome, high serum
estradiol levels, a larger number of follicles, and pregnancy. If the woman is
preg-nant, she is producing human chorionic gonadotropin, which can worsen
OHSS. Symptoms include abdominal discomfort, distention, weight gain, and
ovarian enlargement. This condition may be moderate, severe, or critical.
Severe OHSS may result in acute respiratory distress syndrome (ARDS). It is
prevented by careful monitoring and adjustment of medication dosage.
Management
in mild and moderate cases of OHSS consists of decreased activity, monitoring
of urine output, and frequent office visits as designated by the reproductive
endocrinologist. The patient with severe OHSS is hospitalized for monitoring
and treatment. Severe OHSS is characterized by clinical ascites, hypovolemia,
oliguria, hemoconcentration, electrolyte imbal-ance, and ovarian size greater
than 10 cm. Treatment of severe OHSS includes use of an indwelling catheter for
strict monitor-ing of fluid intake and output and daily measurements of weight
and abdominal circumference. Intravenous fluids and heparin are administered as
prescribed. The patient is permitted to ambulate as tolerated. Critical OHSS is
life-threatening and is characterized by tense ascites that may be accompanied
by hydrothorax, renal failure, and ARDS. Volume expanders, di-uretic agents,
hemodialysis, and intubation may be required (Copeland, 2000).
ARTIFICIAL INSEMINATION
Depositing
semen into the female genital tract by artificial means is called artificial
insemination. If the sperm cannot penetrate the cervical canal normally,
artificial insemination using the partner’s semen (AIH, or artificial
insemination with sperm from the husband or partner) may be considered. In
azoosper-mia (lack of sperm in the semen), semen from carefully selected donors
may be used (AID, or artificial insemination with sperm from donor).
Indications
for using artificial insemination include: (1) the man’s inability to deposit
semen in the vagina, which may be due to premature ejaculation, pronounced
hypospadias (a displaced male urethra), or dyspareunia (painful intercourse
experienced by the woman), (2) inability of semen to be transported from the
vagina to the uterine cavity (this is usually due to faulty chemical conditions
and may occur with an abnormal cervical discharge), and (3) a single woman’s
desire to have a child.
The
woman may have received clomiphene (Clomid) and menotropins (Pergonal) to
stimulate ovulation before insemina-tion. Ultrasounds and blood studies of
varying hormone levels are used to pinpoint the best time for insemination and
to monitor for OHSS. The recipient is placed in the lithotomy position on the
ex-amination table, a speculum is inserted, and the vagina and cervix are
swabbed with a cotton-tipped applicator to remove any excess secretions. Semen
is drawn into a sterile syringe, and a cannula is attached. The semen is then
directed to the external os. Semen may also be placed into the uterine cavity
(intrauterine insemination). In this procedure, the sperm are washed before
insertion to remove biochemicals and to select the most active sperm. This is
indicated when mucus is inadequate, when antibodies are present, or when the
sperm count is low. After careful withdrawal of the cannula, the patient
remains in a supine position for 30 minutes.
The
success rate for artificial insemination varies. Three to six inseminations may
be required over 2 to 4 months. Because arti-ficial insemination is likely to
be a stressful and difficult situation for couples, nursing support and
strategies to promote coping are crucial.
Cannula With Partner’s Semen.
Certain
conditions need to beestablished before semen is transferred to the vagina. The
woman must have no abnormalities of the genital system, the fallopian tubes
must be patent, and ova must be available. In the male, sperm need to be normal
in shape, amount, motility, and en-durance. The time of ovulation should be
determined as accu-rately as possible so that the 2 or 3 days during which
fertilization is possible each month can be targeted for treatment.
Fertilization seldom
occurs from a single insemination. Usually, insemination is attempted between
days 10 and 17 of the cycle; three different attempts may be made during one
cycle. Semen is collected by masturbation; alternatively, a perforated sheath
is worn over the penis during intercourse by couples who object to
masturbation. Withdrawal and using condoms for sperm collection are consid-ered
unsatisfactory by many infertility specialists because some sperm may be lost
or adversely affected.
Insemination With Donor Semen.
When the
sperm of thewoman’s partner is defective or absent or when there is a risk of
transmitting a genetic disease, donor sperm may be used. Safe-guards are put in
place to address legal, ethical, emotional, and religious issues. Written
consent is obtained to protect all parties involved, including the woman, the
donor, and the resulting child. The donor’s semen is frozen and the donor is
evaluated to ensure that he is free of genetic disorders and STDs, including
HIV infection.
IN VITRO FERTILIZATION
In
vitro fertilization (IVF) involves ovarian stimulation, egg re-trieval,
fertilization, and embryo transfer. This procedure is ac-complished by first
stimulating the ovary to produce multiple eggs or ova, usually with
medications, because success rates are greater with more than one early embryo.
Many different proto-cols exist for inducing ovulation with one or more agents.
Pa-tients are carefully selected and evaluated, and cycles are carefully
monitored using ultrasound and estradiol levels. At the appro-priate time, the
ova are recovered by transvaginal ultrasound re-trieval. Sperm and eggs are
coincubated for up to 36 hours, and the embryos are transferred about 48 hours
after retrieval. Im-plantation should occur in 3 to 5 days.
Gamete
intrafallopian transfer (GIFT), a variation of IVF, is the treatment of choice
for patients with ovarian failure. Success rates vary from 20% to 30%. The
ovaries are stimulated with go-nadotropin derivatives, and follicles are
observed with vaginal ultrasound. Once the oocyte is mature, it is retrieved by
laparoscopy or transvaginally with ultrasound guidance. The oocyte
(unfertilized egg) is removed and drawn into a catheter, where it is mixed with
sperm that was obtained shortly before the oocyte retrieval. The most motile
fraction of sperm is selected by a washing process. The oocyte and sperm are
then inserted into the fallopian tube, where fertilization occurs. The latter
method avoids anesthesia. GIFT is the technique of choice for nontubal causes
of infertility and for older infertile women.
Zygote
intrafallopian transfer (ZIFT) consists of oocyte re-trieval and fertilization
in vitro; the zygotes are placed into the fal-lopian tubes via laparoscopy.
The
most common indications for IVF and GIFT are ir-reparable tubal damage,
endometriosis, immunologic problems, unexplained infertility, inadequate sperm,
and exposure to DES.
OTHER ASSISTED REPRODUCTIVE TECHNOLOGIES
In
intracytoplasmic sperm injection (ICSI), an ovum is retrieved as described
previously, and a single sperm is injected through the zona pellucida, through
the egg membrane, and into the cyto-plasm of the oocyte. The fertilized egg is
then transferred back to the donor. ICSI is the treatment of choice in severe
male factor infertility.
Women
who cannot produce their own eggs (ie, premature ovarian failure) have the
option of using the eggs of a donor after stimulation of the donor’s ovaries.
The recipient also receives hor-mones in preparation for these procedures.
Couples may also choose this modality if the female partner has a genetic
disorder that may be passed on to children.
Nursing Management
Nursing
interventions appropriate when working with couples during infertility
evaluations include the following: assist in re-ducing stress in the
relationship, encourage cooperation, protect privacy, foster understanding, and
refer the couple to appropri-ate resources when necessary. Because infertility
workups are expensive, time-consuming, invasive, stressful, and not always
successful, couples need support in working together to deal with this
endeavor.
Resolve,
Inc., a nonprofit self-help group that provides infor-mation and support for
infertile patients, was founded by a nurse who experienced difficulty
conceiving. The literature on infertil-ity that is produced by this group is an
important resource for pa-tients and professionals. Most areas across the
country have local support groups. More information can be obtained by writing
to Resolve, Inc..
Smoking
is strongly discouraged because it has an adverse ef-fect on the success of
assisted reproduction. Diet, exercise, stress reduction techniques, health
maintenance, and disease preven-tion are being emphasized in many infertility
programs.
Related Topics