Chapter: Medical Surgical Nursing: Assessment and Management of Female Physiologic Processes
Function of the Female Reproductive System
FUNCTION
OF THE FEMALE REPRODUCTIVE SYSTEM
Ovulation
At puberty (usually between ages 12 and 14, but earlier for some; 10 or 11 years of age is not uncommon), the ova begin to mature. During a period known as the follicular phase, an ovum enlarges as a type of cyst called a graafian follicle until it reaches the surface of the ovary, where transport occurs.
The ovum (or oocyte) is discharged into
the peritoneal cavity. This periodic discharge of matured ovum is referred to
as ovulation. The ovum usually finds
its way into the fallopian tube, where it is carried to the uterus. If it meets
a spermatozoon, the male reproductive cell, a union occurs and conception takes
place. After the discharge of the ovum, the cells of the graafian follicle
undergo a rapid change. Gradually, they become yellow (corpus luteum) and produce progesterone,
a hormone that prepares the uterus for receivingthe fertilized ovum. Ovulation
usually occurs 2 weeks prior to the next menstrual period.
The Menstrual Cycle
The
menstrual cycle is a complex process involving the reproduc-tive and endocrine
systems. The ovaries produce steroid hormones, predominantly estrogens and
progesterone. Several different es-trogens
are produced by the ovarian follicle, which consists of thedeveloping ovum
and its surrounding cells. The most potent of the ovarian estrogens is
estradiol. Estrogens are responsible for developing and maintaining the female
reproductive organs and the secondary sex characteristics associated with the
adult female. Estrogens play an important role in breast development and in
monthly cyclic changes in the uterus.
Progesterone
is also important in regulating the changes that occur in the uterus during the
menstrual cycle. It is secreted by the corpus luteum, which is the ovarian
follicle after the ovum has been released. Progesterone is the most important
hormone for conditioning the endometrium
(the mucous membrane lining the uterus) in preparation for implantation of a
fertilized ovum. If pregnancy occurs, the progesterone secretion becomes
largely a function of the placenta and is essential for maintaining a normal
pregnancy. In addition, progesterone, working with estrogen, pre-pares the
breast for producing and secreting milk. Androgens
are also produced by the ovaries, but only in small amounts. These hormones are
involved in the early development of the follicle and also affect the female
libido.
Two
gonadotropic hormones are released by the pituitary gland: FSH and LH. Follicle-stimulating hormone (FSH) is
primarily responsible for stimulating the ovaries to secrete estro-gen. Luteinizing hormone (LH) is primarily
responsible for stimulating progesterone production. Feedback mechanisms, in
part, regulate FSH and LH secretion. For example, elevated es-trogen levels in
the blood inhibit FSH secretion but promote LH secretion, whereas elevated
progesterone levels inhibit LH secre-tion. In addition, gonadotropin-releasing
hormone (GnRH) from the hypothalamus affects the rate of FSH and LH release.
The
secretion of ovarian hormones follows a cyclic pattern that results in changes
in the uterine endometrium and in menstrua-tion
(Fig. 46-3; Table 46-1). This cycle is typically 28 days inlength, but
there are many normal variations (21 to 42 days). In the proliferative phase at the beginning of the cycle (just after
men-struation), FSH output increases, stimulating estrogen secretion. This
causes the endometrium to thicken and become more vascu-lar. In the secretory phase near the middle portion
of the cycle (day 14 in a 28-day cycle), LH output increases, stimulating
ovulation. Under the combined stimulus of estrogen and progesterone, the
endometrium reaches the peak of its thickening and vasculariza-tion. The luteal phase begins after ovulation and
is characterized by the secretion of progesterone from the corpus luteum.
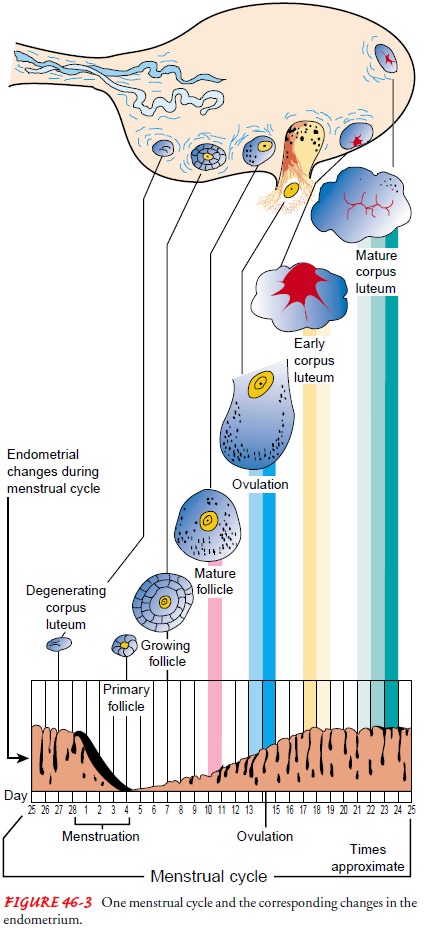
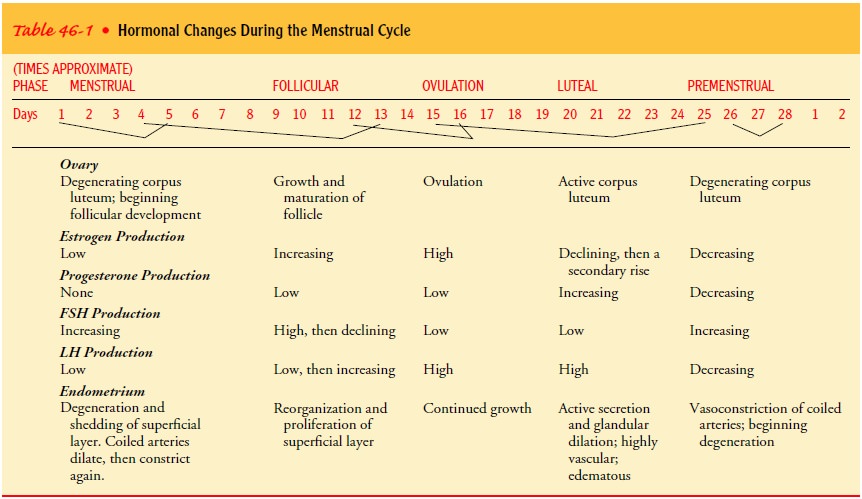
If the ovum is fertilized, estrogen and progesterone levels re-main high and the complex hormonal changes of pregnancy fol-low. If the ovum has not been fertilized, FSH and LH output diminishes, estrogen and progesterone secretion falls, the ovum disintegrates, and the endometrium, which has become thick and congested, becomes hemorrhagic. The product consisting of old blood, mucus, and endometrial tissue is discharged through the cervix and into the vagina. After the menstrual flow stops, the cycle begins again; the endometrium proliferates and thickens from estrogenic stimulation, and ovulation recurs.
Menopausal Period
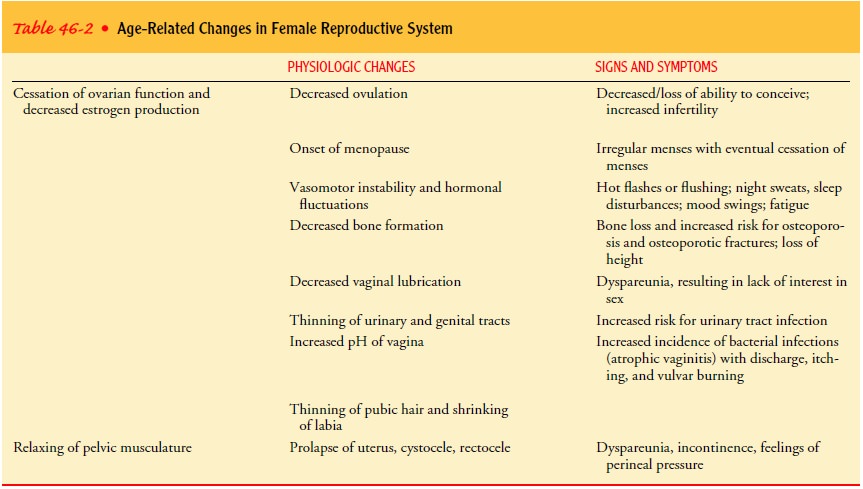
The
menopausal period marks the end of a woman’s reproductive capacity. It usually
occurs between the ages of 45 and 52 years but may occur as early as age 42 or
as late as age 55; the median age is 51. Menopause
is not a pathologic phenomenon but a normal part of aging and maturation.
Menstruation ceases, and because the ovaries are no longer active, the
reproductive organs become smaller. No more ova mature; therefore, no ovarian
hormones are produced. (An artificial menopause may occur earlier if the
ovaries are surgically removed or are destroyed by radiation or chemotherapy.)
Besides changes in the reproductive system that reduce estrogen levels,
multifaceted changes occur throughout the woman’s body. These changes include
neuroendocrinologic, bio-chemical, and metabolic alterations related to normal
maturation or aging (Table 46-2).
Related Topics