Chapter: Essentials of Anatomy and Physiology: Reproductive System
Male Reproductive System
MALE REPRODUCTIVE SYSTEM
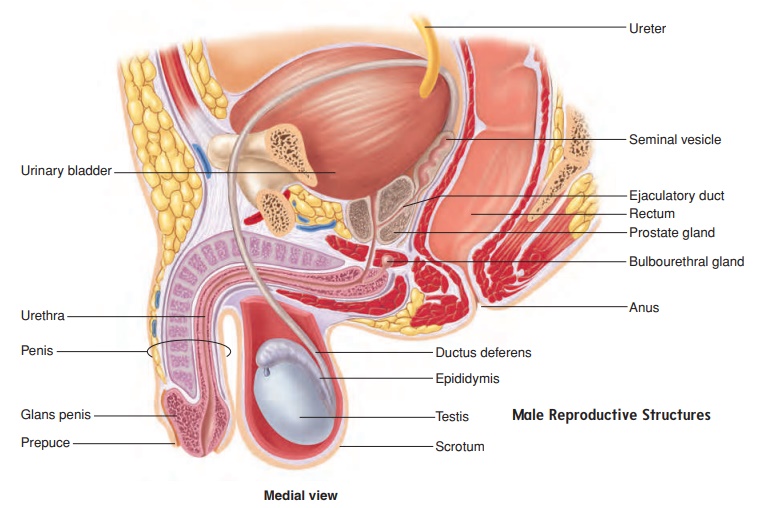
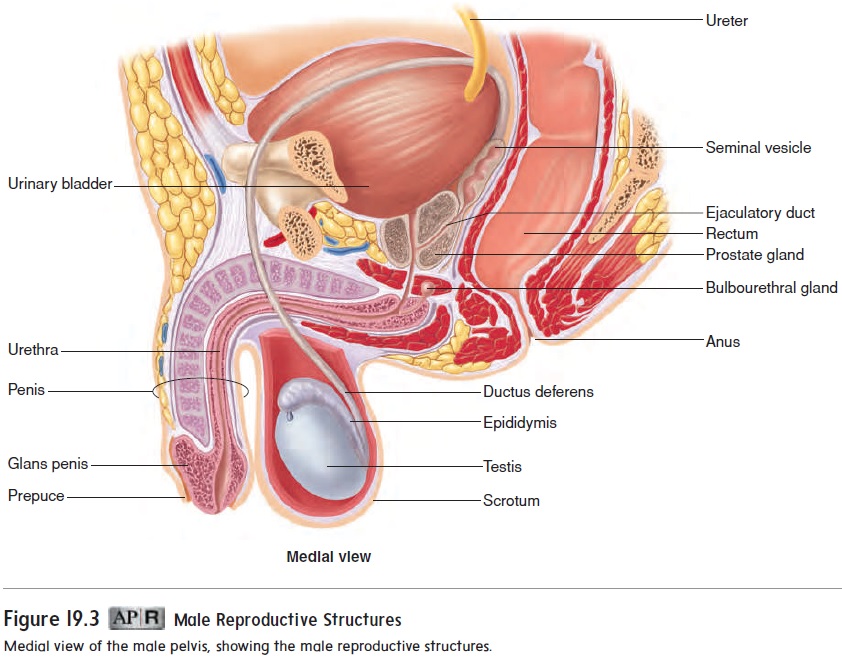
The male reproductive system consists of the testes (sing. testis), a series of ducts, accessory glands, and supporting structures. The ducts include the epididymides (sing. epididymis), the ducta deferentia (sing. ductus deferens; also, vas deferens), and the ure-thra. Accessory glands include the seminal vesicles, the prostate gland, and the bulbourethral glands. Supporting structures include the scrotum and the penis (figure 19.3). The sperm cells are very heat-sensitive and must develop at a temperature slightly less than normal body temperature. The testes, in which the sperm cells develop, are located outside the body cavity in the scrotum, where the temperature is lower. Sperm cells travel from each testis to the prostate gland and then empty into the urethra within the prostate gland. The urethra exits the pelvis, passes through the penis, and opens to the outside of the body.
Scrotum
The scrotum (skrō′ tum) is a saclike structure containing the testes. It is divided into right and left internal compartments by an incom-plete connective tissue septum. Externally, the scrotum consists of skin. Beneath the skin are a layer of loose connective tissue and a layer of smooth muscle called the dartos (dar′ tōs) muscle.
In cold temperatures, the dartos muscle contracts, causing the skin of the scrotum to become firm and wrinkled and reducing the overall size of the scrotum. At the same time, extensions of abdominal muscles into the scrotum, called cremaster (krē-mas′ ter) muscles, contract (see figure 19.6). Consequently, the testes arepulled nearer the body, and their temperature is elevated. During warm weather or exercise, the dartos and cremaster muscles relax, the skin of the scrotum becomes loose and thin, and the tes-tes descend away from the body, which lowers their temperature. The response of the dartos and cremaster muscles is important in regulating the temperature in the testes. If the testes become too warm or too cold, normal sperm cell development does not occur.
Testes
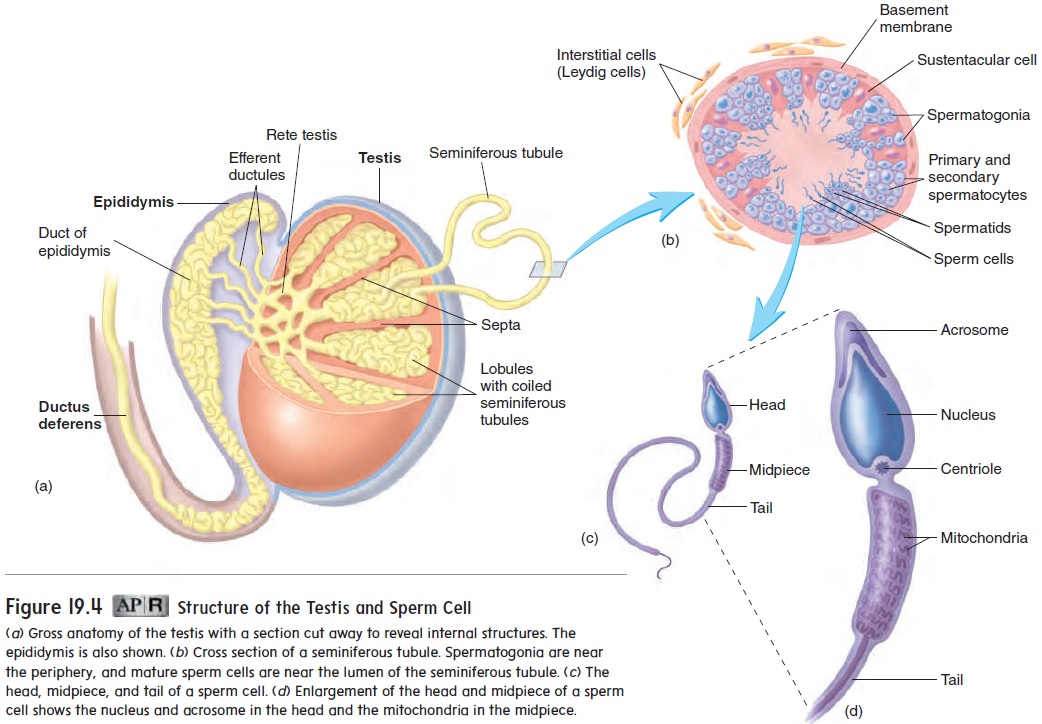
(sem′ -nif′ er-ŭ s) tubules, in which sperm cells develop. Delicate connective tissue surrounding the seminiferous tubules contains clusters of endocrine cells called interstitial (in-ter-stish′ ă l) cells, or Leydig(lı̄ ′ dig) cells, which secrete testosterone. The seminifer-ous tubules contain germ cells and sustentacular cells, or Sertoli(ser-tō ′ lē ) cells (figure 19.4b). Sustentacular cells are large and extend from the periphery to the lumen of the seminiferous tubule. They nourish the germ cells and produce a number of hormones.
Spermatogenesis
Spermatogenesis (sper′m̆a-t̄o-jen′̆e-sis) is the formation of spermcells. Before puberty, the testes remain relatively simple and unchanged from the time of their initial development.
The interstitial cells are not prominent, and the seminiferous tubules are small and not yet functional. At the time of puberty, the interstitial cells increase in number and size, the seminiferous tubules enlarge, and spermatogenesis begins.
Germ cells are partially embedded in the sustentacular cells. The most peripheral germ cells are spermatogonia (sper′ mă-tō-gō′ nē-ă; undeveloped sperm cells), which divide through mitosis (figure 19.5). Some daughter cells produced from these mitotic divi-sions remain as spermatogonia and continue to divide by mitosis. Other daughter cells form primary spermatocytes (sper′ mă-tō-sı̄tz; sperm cells), which divide by meiosis and become sperm cells.
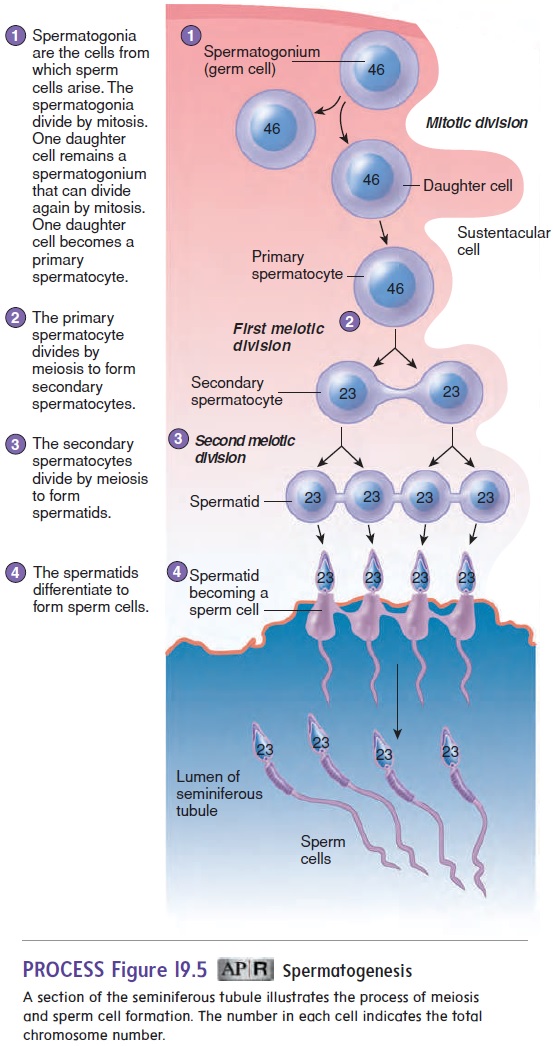
Spermatogenesis
A primary spermatocyte contains 46 chromosomes, each con-sisting of 2 chromatids. Each primary spermatocyte passes through the first meiotic division to produce 2 secondary spermatocytes. Each secondary spermatocyte undergoes the second meiotic division to produce 2 smaller cells called spermatids (sper′ mă-tidz), each having 23 chromosomes. After the second meiotic division, the spermatids undergo major structural changes to form sperm cells (figure 19.5; see figure 19.4b,c). Much of the cytoplasm of the sper-matids is eliminated, and each spermatid develops a head, midpiece, and flagellum (tail) to become a sperm cell, or spermatozoon (figure 19.5; see figure 19.4b–d). The nucleus of the sperm cell is located in the head of the sperm cell. Just anterior to the nucleus is a vesicle called theacrosome (ak′ rō-sōm), which contains enzymes that are released during the process of fertilization and are necessary for the sperm cell to penetrate the oocyte, or egg cell.
At the end of spermatogenesis, the developing sperm cells are located around the lumen of the seminiferous tubules, with their heads directed toward the surrounding sustentacular cells and their tails directed toward the center of the lumen (figure 19.5; see fig-ure 19.4b). Finally, sperm cells are released into the lumen of the seminiferous tubules.
Ducts
After their production, sperm cells are transported through the semi-niferous tubules and a series of ducts to the exterior of the body.
Epididymis
The seminiferous tubules of each testis empty into a tubular net-work called the rete (rē′ tē; net) testis (see figure 19.4a). The rete testis empties into 15–20 tubules called the efferent ductules (ef′ er-ent dŭk′ toolz). The efferent ductules carry sperm cells from the testis to a tightly coiled series of threadlike tubules that form a comma-shaped structure on the posterior side of the testis called the epididymis (ep-i-did′ i-mis) (figure 19.6; see figures 19.3 and 19.4). The sperm cells continue to mature within the epididymis, developing the capacity to swim and the ability to bind to the oocyte. Sperm cells taken directly from the testes are not capable of fertilizing oocytes, but after maturing for several days in the epididymis, the sperm cells develop the capacity to function as gametes. Final changes in sperm cells, calledcapacitation (kă-pas′ i-tă′ shun), occur after ejaculation of semen into the vagina and prior to fertilization.
Ductus Deferens
The ductus deferens (dŭk′ tŭs def′ er-enz), or vas deferens, emerges from the epididymis and ascends along the posterior side of the testis to become associated with the blood vessels and nerves that supply the testis. These structures form the spermatic cord (figure 19.6a). Each spermatic cord consists of the ductus defer-ens, testicular artery and veins, lymphatic vessels, and testicular nerve. It is surrounded by the cremaster muscle and two connective tissue sheaths.
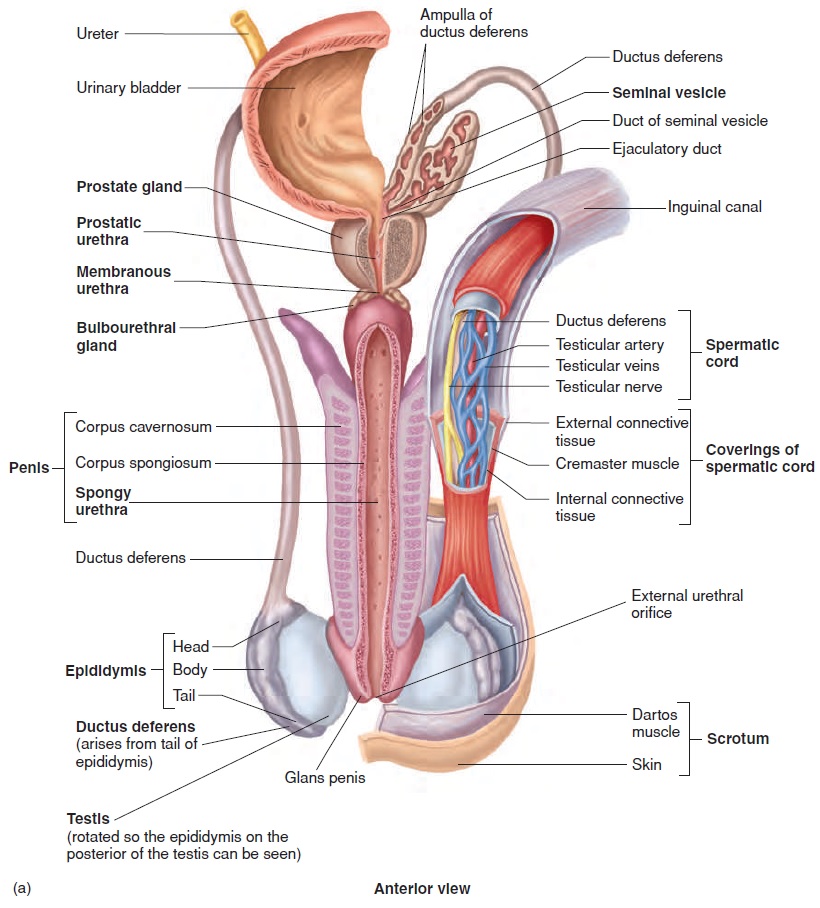
Each ductus deferens extends, in the spermatic cord, through the abdominal wall by way of the inguinal canal. Each ductus def-erens then crosses the lateral wall of the pelvic cavity and loops behind the posterior surface of the urinary bladder to approach the prostate gland (figure 19.6a; see figure 19.3). The total length of the ductus deferens is about 45 cm.
Just before reaching the pros-tate gland, the ductus deferens increases in diameter to become the ampulla of the ductus deferens (figure 19.6a). The wall of the ductus deferens contains smooth muscle, which contracts in peristaltic waves to propel the sperm cells from the epididymis through the ductus deferens.
Seminal Vesicle and Ejaculatory Duct
Urethra
The male urethra (ū-rē′ thră) extends from the urinary bladder to the distal end of the penis (figure 19.6a; see figure 19.3). The ure-thra can be divided into three parts: the prostatic urethra, which passes through the prostate gland; the membranous urethra, which passes through the floor of the pelvis and is surrounded by the external urinary sphincter; and the spongy urethra, which extends the length of the penis and opens at its end. The urethra is a passageway for both urine and male reproductive fluids. However, urine and the reproductive fluids do not exit the ure-thra at the same time. While male reproductive fluids are passing through the urethra, a sympathetic reflex causes the internal uri-nary sphincter to contract, which keeps semen from passing into the urinary bladder and prevents urine from entering the urethra.
Penis
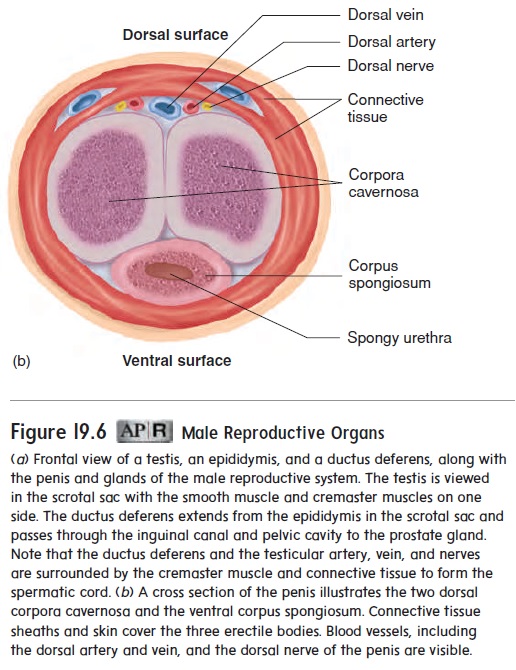
The penis (pe′ nis) is the male organ of copulation and func-tions in the transfer of sperm cells from the male to the female. The penis contains three columns of erectile tissue (figure 19.6). Engorgement of this erectile tissue with blood causes the penis to enlarge and become firm, a process called erection (ē-rek′ shŭn). Two columns of erectile tissue form the dorsal portion and the sides of the penis and are called the corpora cavernosa (kōr′ pōr-ă kav-er-nōs′ ă). The third, smaller erectile column occupies theventral portion of the penis and is called the corpus spongiosum (kōr′ pŭs spŭn-gē-ō′ sŭm). It expands over the distal end of the penis to form a cap, the glans (glanz) penis. The spongy urethra passes through the corpus spongiosum, including the glans penis, and opens to the exterior as the external urethral orifice.
The shaft of the penis is covered by skin that is loosely attached to the connective tissue surrounding the penis. The skin is firmly attached at the base of the glans penis, and a thinner layer of skin tightly covers the glans penis. The skin of the penis, espe-cially the glans penis, is well supplied with sensory receptors. A loose fold of skin, called the prepuce (prē′ pūs), or foreskin, covers the glans penis (see figure 19.3).
Glands
The seminal vesicles are glands consisting of many saclike structures located next to the ampulla of the ductus deferens (figure 19.6a; see figure 19.3). There are two seminal vesicles.
Each is about 5 cm long and tapers into a short duct that joins the ampulla of the ductus deferens to form the ejaculatory duct, as previously mentioned.
The prostate (pros′ tāt) gland consists of both glandular and muscular tissue and is about the size and shape of a walnut (figure 19.6a; see figure 19.3). The prostate gland surrounds the urethra and the two ejaculatory ducts. It consists of a capsule and numerous partitions. The cells lining the partitions secrete prostatic fluid. There are 10–20 short ducts (not seen in figure 19.6a) that carry secretions of the prostate gland to the prostatic urethra.
The bulbourethral (bul′ b̄o -̄u -r̄e ′ thr̆a l) glands, or Cowperglands, are a pair of small, mucus-secreting glands located near thebase of the penis (figure 19.6a; see figure 19.3). In young adults, each is about the size of a pea, but they decrease in size with age. A single duct from each gland enters the urethra.
Secretions
Semen (sē′men) is a mixture of sperm cells and secretions from themale reproductive glands. The seminal vesicles produce about 60% of the fluid, the prostate gland contributes approximately 30%, the testes contribute 5%, and the bulbourethral glands contribute 5%.
The bulbourethral glands and the mucous glands in the urethra produce a mucous secretion, which lubricates the urethra, helps neutralize the contents of the normally acidic urethra, provides a small amount of lubrication during intercourse, and helps reduce acidity in the vagina.
Testicular secretions include sperm cells and a small amount of fluid. The thick, mucuslike secretion of the seminal vesicles contains the sugar fructose and other nutrients that nourish sperm cells. The seminal vesicle secretions also contain proteins that weakly coagulate after ejaculation and enzymes that are thought to help destroy abnor-mal sperm cells. Prostaglandins, which stimulate smooth muscle contractions, are present in high concentrations in the secretions of the seminal vesicles and can cause contractions of the female repro-ductive tract, which help transport sperm cells through the tract.
The thin, milky secretions of the prostate have an alkaline pH and help neutralize the acidic urethra, as well as the acidic secretions of the testes, the seminal vesicles, and the vagina. The increased pH is important for normal sperm cell function. The movement of sperm cells is not optimal until the pH is increased to between 6.0 and 6.5. In contrast, the pH of vaginal secretions is between 3.5 and 4.0. Prostatic secretions also contain proteolytic enzymes that break down the coagulated proteins of the seminal vesicles and make the semen more liquid. The normal volume of semen is 2–5 milliliters (mL), with each milliliter of semen typi-cally containing about 100 million sperm cells.
Related Topics