Chapter: Microbiology and Immunology: Bacteriology: Campylobacter and Helicobacter
Laboratory Diagnosis of Helicobacter pylori Infections
Laboratory Diagnosis
◗ Specimens
These include stool samples and gastric biopsy specimen.
◗ Microscopy
H. pylori is demonstrated by microscopic examination of gastricbiopsy specimen stained with Gram, Giemsa, Warthin Starry silver, and hematoxylin–eosin stains. All these stains show organisms of H. pylori adhered to gastric mucosa. These meth-ods are highly specific.
◗ Culture
Diagnosis of H. pylori infection is made by culture of clinical specimens on freshly prepared chocolate agar and Skirrow’s campylobacter selective media followed by incubation at 35–37°C in a microaerophilic environment (5% O2, 10% CO2, and 85% N2) for 3–5 days. H. pylori produces convex, circular, and large colonies on these selective media.
◗ Identification of bacteria
Identification of bacterial isolates is made on the basis of typi-cal growth characteristics of H. pylori on selective medium; morphology; and oxidase, catalase, and urease test.
◗ Serology
ELISA is used for demonstration of serum antibodies to H. pylori in the patient serum. But since the antibody titers con-tinue to remain elevated a long time after H. pylori eradication, antibody-based test cannot distinguish between recent and old infection. ELISA shows a high sensitivity and specificity.
◗ Fecal antigen test
This is an immunochromatographic test, which uses monoclo-nal antibody for direct detection of H. pylori antigen in stool samples. This test is very sensitive (94%) and specific (98%).
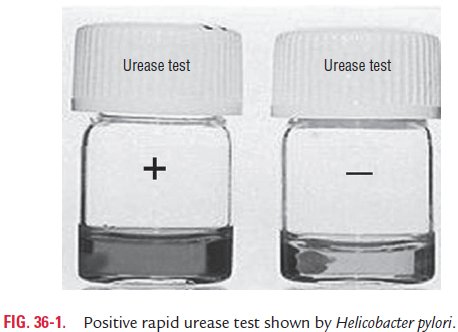
◗ Urease test
The urease test is the most rapid test, which can be dem-onstrated directly in the biopsy specimen. In this test, the biopsy tissues are put in a urease indicator medium (0.5 mL urea solution with an indicator) and incubated at 37°C. If H. pylori is present, the color of the medium changes due tochange of pH of the medium within a few minutes to 2 hours due to the production of ammonia. The test is highly spe-cific (100%), but sensitivity varies from 75% to 95% (Fig. 36-1, Color Photo 37).
◗ Rapid urea breath test
This test is based on detection of the products of urea degraded by H. pylori. In this method, patients drink a beverage that con-tains urea labeled with a carbon isotope, such as carbon 13 or carbon 14. After a short period of time, the concentration of labeled carbon is measured in the breath. The concentration is high only when urease present in H. pylori found in the stomach breaks down the urea. In normal human host, the concentra-tion of the labeled carbon in breath would not be high because the human stomach does not contain any urease. Positive urea breath test indicates H. pylori infection. The breath test is a very selective test. Disadvantages of the test are that it may show false positive results in:
infections with coccoid forms of H. pylori that do not pro-duce more urease enzymes and
patients receiving antibiotics, such as bismuth and hista-mine-2 blockers.
Related Topics