Chapter: Medicine Study Notes : Pharmacology
Inter-individual Differences - Pharmacokinetics
Inter-individual Differences
·
There are large inter-individual
differences in the capacity to metabolise drugs, due to:
Genetic factors
· Characteristics can be autosomal dominant, autosomal recessive, sex-linked, etc
· Either polygenic or monogenic (present either as polymorphisms – more than 1% - or as rare phenotypes - <1 %)
·
Cytochrome P450: a group of
enzymes located on the endoplasmic reticulum. Divided into families and
sub-families
· 3 polymorphisms have been well defined:
o Acetylation: enzyme: n-acetyl-transferase 2. Leads to slow and fast acetylators. 90% of Japanese are fast acetylators (autosomal dominant) compared with 55 – 60% of Europeans who are slow acetylators. Affects eg isoniazid and caffeine
o Oxidation: poor metabolisers are deficient in enzyme CYP2D6, affects 4 hydroxylation pathway. Covers lots of drugs – TCAs, antipsychotics (e.g. haloperidol), b blockers (e.g. metoprolol). ÂRisk of accumulation. Rest of population are extensive metabolisers
o Oxidation (CYP2C19): affects diazepam, omeprazole, others
Disease
·
Absorption in disease:
o Can affect gastric emptying rate: affects rate not extent
o ÂŻAbsorption rate in migraine, acute MI, labour, malabsorption syndromes (variable effect)
o Low cardiac output ® ¯IM absorption
· Distribution:
o For drugs with low Vd and high binding (only), changes in protein binding: e.g. ÂŻalbumin in hepatic disease, nephrotic syndrome, Âa1AGP in RA, Crohn‟s. Amount of free drug is the same.
o But normally total plasma concentration measured (and this will be reduced) ® danger of overdose
o Cardiac disease ® altered distribution (eg due to reduced gut flow ® poor absorption, ¯renal and hepatic perfusion ® ¯clearance)
o Obesity ® increased Vd for lipophilic drugs
· Metabolism:
o Most biotransformation occurs in liver. For some drugs, extraction depends on blood flow (where extraction ratio tends to 1)
o Liver disease ® ÂŻcapacity of metabolising enzymes (eg Âwarfarin, phenytoin) and possibly shunting of blood around liver (affects drugs with high first pass metabolism)
o Thyroid diseases ®  or ¯ metabolism
o Diabetes mellitus ® fatty liver ® change in metabolism
o Low clearance with high (>90%) degree of protein binding – generally ¯clearance
o Low clearance, low binding (e.g. paracetamol) – variable but can be ¯clearance
· Excretion:
o For many drugs, reduction in clearance ® Âhalf-life
o Adjust dose using creatinine clearance formula: Cockcroft Gault Formula
(a prediction which saves doing a 24 hr urine):
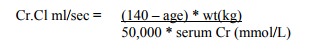
§ Cr.Cl ml/sec = (140 – age) * wt(kg)/ 50,000 * serum Cr (mmol/L)
·
Normal is 1.5 mls/sec. For mls/min, replace 50,000 by 815
·
For females, multiply by 0.85
o Important for eg digoxin and aminoglycosides which are excreted unchanged. If elderly ®¯excretion ® Âplasma concentration
·
Dose rate for a drug excreted
100% by the kidney (e.g. antibiotics) is:
·
DR = (Cr.Cl / 1.5) * normal DR
· This dose requires adjustment when not all the drug is excreted unchanged.
DR = (1 – fu) + fu * Cr.Cl / 1.5 * DR
Fu = fraction excreted unchanged
·
Liver disease: arbitrary rule:
o ÂŻDose by
50% for high clearance drugs (high 1st pass metabolism)
o ÂŻDose by
25% for low clearance drugs (enzyme capacity only)
·
Dosing in CV disease:
o ÂŻVd (vasoconstriction)
o ÂŻRenal
flow ® ¯excretion
o ÂŻMesenteric
blood flow ® ¯absorption of frusemide
Age
·
Epidemiology:
o Elderly > 75 years
o More likely to have multiple drugs (median per person over 65 is 3), 90% have one drug
o 2 * incidence of adverse reactions (20 – 25%).  in proportion to number of drugs
o 30% of elderly admissions due to drug problems
·
Absorption: little difference
compared with young, except if other drugs interfere (eg ÂŻ transit
time)
· Distribution:
o ÂŻLean body weight. ÂVd of fat soluble drugs (eg diazepam), possible problems with accumulation
o May be Âadipose compared with lean body tissue. Eg smaller loading dose of drugs with low Vd (eg digoxin and cimetidine)
o Protein binding: Albumin declines with age ® significant change only in tightly bound drugs (ie small Vd, eg phenytoin) or zero order elimination (eg warfarin)
· Metabolism: Hepatic clearance:
§ Liver has significant residual capacity so not much decline with age, especially given ¯ lean body weight
§ But significant (50%) reduction in liver blood flow, so significant reduction in metabolism of 1st pass metabolism (eg propranolol) or capacity limited metabolism (phenytoin or theophylline). Problem if narrow TI
§ ¯Hepatic
blood flow and hepatic mass
§ ¯First
pass clearance: eg major tranquillisers, TCAs, antiarrhythmics
· Excretion:
o Decline in renal function. ÂŻGRF by 50% (although wider spread of function ® Âinter-individual variability). Problems with digoxin, lithium and gentamycin
o ÂŻRenal clearance (see creatinine clearance above). However, Âvariability in serum creatinine (eg proportional to lean body mass) ® less reliable estimate of renal function
o Delayed action of renal acting drugs (eg diuretics)
o Tolerate renal side effects less well (eg NSAIDs)
o Need to adjust dose of: digoxin, cimitidine, ACE inhibitors, NSAID, Diazepam, aminoglycosides.
o Dose adjustment factor =
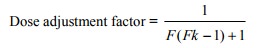
• F = fraction of drug normally excreted unchanged
• Kf = relative renal function of a patient = actual or derived Cr clearance [use Cockcroft & Gault formula ] / normal Cr clearance
• Principles of geriatric prescribing:
o Full drug history
o Reasonable therapeutic objective (ie forget management of long term risk
factors if they‟re 95)
·
Individual dose titration –
beware „usual‟ doses
·
Lowest possible dose
·
Simplest possible regime
·
Regular review of drug therapy
Children
· Clearance: functional maturity reached from 6 months to 1 year
·
Vd: have more body water and less
fat Ăž Âdose for H2O soluble and ÂŻ for lipid soluble
·
Guidelines:
o If < 6 months: consult a paediatrician
o 6 months to 1 year: use a nomogram for surface area. Estimates Dose =
[wt (kg) ^ 2/1.7 m ^2] * adult dose
Other Factors
· Sex: Women clear BZDs faster, NSAIDs slower
· Pregnancy: more rapid clearance of oxidised drugs due to Âliver flow.
·
Obesity: Use ideal body weight if
actual > 30% above ideal for drugs with low Vd
·
Environment
·
Diet: eg smoking, grapefruit
juice, malnutrition, alcohol
Related Topics