Chapter: Basic & Clinical Pharmacology : Thyroid &Antithyroid Drugs
Hypothyroidism
CLINICAL PHARMACOLOGY OF THYROID & ANTITHYROID DRUGS
HYPOTHYROIDISM
Hypothyroidism
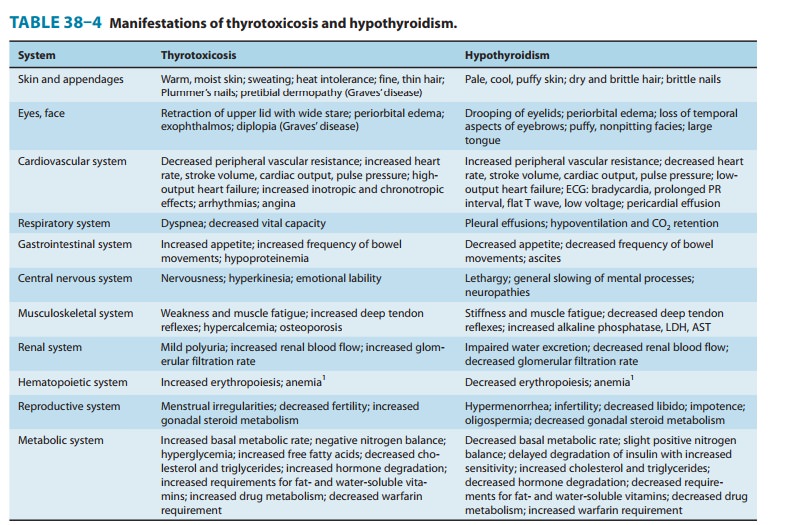
is a syndrome resulting from deficiency of thyroid hormones and is manifested
largely by a reversible slowing down of all body functions (Table 38–4). In
infants and children, there is striking retardation of growth and development
that results in dwarfism and irreversible mental retardation.
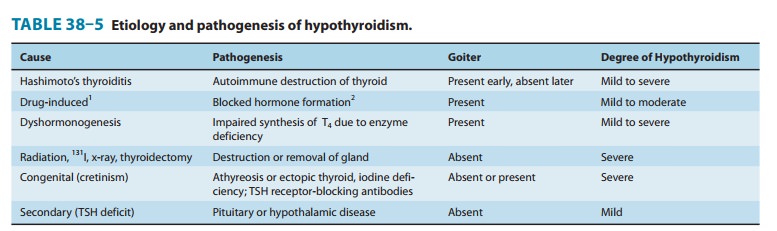
The
etiology and pathogenesis of hypothyroidism are outlined in Table 38–5.
Hypothyroidism can occur with or without thyroid enlargement (goiter). The
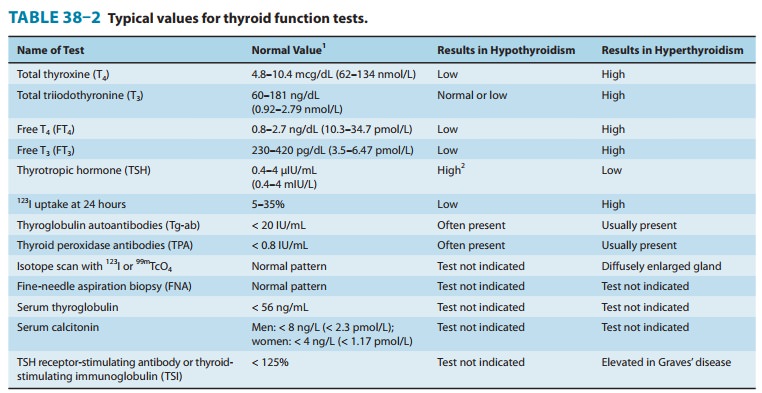
laboratory diagnosis of hypothyroidism in the adult is easily made by the
combination of a low free thyroxine and elevated serum TSH (Table 38–2).
The
most common cause of hypothyroidism in the USA at this time is probably
Hashimoto’s thyroiditis, an immunologic disorder in genetically predisposed
individuals. In this condition, there is evidence of humoral immunity in the
presence of antithyroid anti-bodies and lymphocyte sensitization to thyroid
antigens. Certain medications can also cause hypothyroidism (Table 38–5).
MANAGEMENT OF HYPOTHYROIDISM
Except
for hypothyroidism caused by drugs, which can be treated in some cases by
simply removing the depressant agent, the gen-eral strategy of replacement
therapy is appropriate. The most sat-isfactory preparation is levothyroxine,
administered as either a branded or generic preparation. Treatment with
combination levothyroxine plus liothyronine has not been found to be superior
to levothyroxine alone. Infants and children require more T4
per kilogram of body weight than adults. The average dosage for an infant 1–6
months of age is 10–15 mcg/kg/d, whereas the average dosage for an adult is
about 1.7 mcg/kg/d. Older adults (> 65 years of age) may require less
thyroxine for replacement. There is some variability in the absorption of
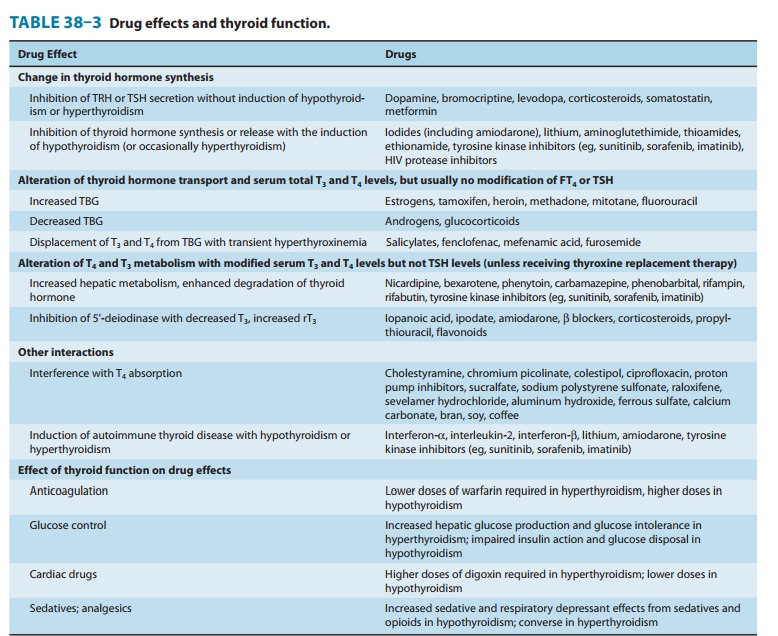
thyroxine, so this dosage will vary from patient to patient. Since interactions
with certain foods (eg, bran, soy, coffee) and drugs (Table 38–3) can impair
its absorption, thyroxine should be administered on an empty stom-ach (eg, 30
minutes before meals or 1 hour after meals or at bedtime). Its long half-life
of 7 days permits once-daily dosing. Children should be monitored for normal
growth and develop-ment. Serum TSH and free thyroxine should be measured at
regu-lar intervals and TSH maintained within an optimal range of 0.5–2.5 mU/L.
It takes 6–8 weeks after starting a given dose of thyroxine to reach
steady-state levels in the bloodstream. Thus, dosage changes should be made
slowly.
In
long-standing hypothyroidism, in older patients, and in patients with
underlying cardiac disease, it is imperative to start treatment with reduced
dosages. In such adult patients, levothy-roxine is given in a dosage of 12.5–25
mcg/d for 2 weeks, increas-ing the daily dose by 12.5–25 mcg every 2 weeks
until euthyroidism or drug toxicity is observed. In older patients, the heart
is very sensitive to the level of circulating thyroxine, and if angina pectoris
or cardiac arrhythmia develops, it is essential to stop or reduce the dose of
thyroxine immediately. In younger patients or those with very mild disease,
full replacement therapy may be started immediately.
The toxicity of
thyroxine is directly related to the hormone level. In children, restlessness,
insomnia, and accelerated bone maturation and growth may be signs of thyroxine
toxicity. In adults, increased nervousness, heat intolerance, episodes of
palpitation and tachycar-dia, or unexplained weight loss may be the presenting
symptoms. If these symptoms are present, it is important to monitor serum TSH
(Table 38–2), which will determine whether the symptoms are due to excess
thyroxine blood levels. Chronic overtreatment with T4, particularly in
elderly patients, can increase the risk of atrial fibrilla-tion and accelerated
osteoporosis.
Special Problems in Management of Hypothyroidism
A. Myxedema and Coronary Artery Disease
Since myxedema
frequently occurs in older persons, it is often asso-ciated with underlying
coronary artery disease. In this situation, the low levels of circulating
thyroid hormone actually protect the heart against increasing demands that
could result in angina pec-toris or myocardial infarction. Correction of
myxedema must be done cautiously to avoid provoking arrhythmia, angina, or
acute myocardial infarction. If coronary artery surgery is indicated, it should
be done first, prior to correction of the myxedema by thyroxine administration.
B. Myxedema Coma
Myxedema
coma is an end state of untreated hypothyroidism. It is associated with
progressive weakness, stupor, hypothermia, hypoventilation, hypoglycemia,
hyponatremia, water intoxication, shock, and death.
Myxedema
coma is a medical emergency. The patient should be treated in the intensive
care unit, since tracheal intubation and mechanical ventilation may be
required. Associated illnesses such as infection or heart failure must be
treated by appropriate ther-apy. It is important to give all preparations
intravenously, because patients with myxedema coma absorb drugs poorly from
other routes. Intravenous fluids should be administered with caution to avoid
excessive water intake. These patients have large pools of empty T3
and T4 binding sites that must be filled
before there is adequate free thyroxine to affect tissue metabolism.
Accordingly, the treatment of choice in myxedema coma is to give a loading dose
of levothyroxine intravenously—usually 300–400 mcg ini-tially, followed by
50–100 mcg daily. Intravenous T3
can also be used but may be more cardiotoxic and more difficult to monitor.
Intravenous hydrocortisone is indicated if the patient has associ-ated adrenal
or pituitary insufficiency but is probably not neces-sary in most patients with
primary myxedema. Opioids and sedatives must be used with extreme caution.
C. Hypothyroidism and Pregnancy
Hypothyroid
women frequently have anovulatory cycles and are therefore relatively infertile
until restoration of the euthyroid state. This has led to the widespread use of
thyroid hormone for infertil-ity, although there is no evidence for its
usefulness in infertile euthyroid patients. In a pregnant hypothyroid patient
receiving thyroxine, it is extremely important that the daily dose of
thyrox-ine be adequate because early development of the fetal brain depends on
maternal thyroxine. In many hypothyroid patients, an increase in the thyroxine
dose (about 30–50%) is required to nor-malize the serum TSH level during
pregnancy. It is reasonable to counsel women to take an extra 25 mcg thyroxine
tablet as soon as they are pregnant and to separate thyroxine from prenatal
vita-mins by at least 4 hours. Because of the elevated maternal TBG levels and,
therefore, elevated total T4 levels,
adequate maternal thyroxine dosages warrant maintenance of TSH between 0.5 and
3.0 mU/L and the total T 4 at or
above the upper range of normal.
D. Subclinical Hypothyroidism
Subclinical
hypothyroidism, defined as an elevated TSH level and normal thyroid hormone
levels, is found in 4–10% of the general population but increases to 20% in
women older than age 50
The
consensus of expert thyroid organizations concluded that thyroid hormone
therapy should be considered for patients with TSH levels greater than 10 mIU/L
while close TSH monitoring is appropriate for those with lower TSH elevations.
E. Drug-Induced Hypothyroidism
Drug-induced
hypothyroidism (Table 38–3) can be satisfactorily managed with levothyroxine
therapy if the offending agent cannot be stopped. In the case of amiodarone-induced
hypothyroidism, levothyroxine therapy may be necessary even after
discontinuance because of amiodarone’s very long half-life.
Related Topics