Chapter: Essential Anesthesia From Science to Practice : Clinical management : Airway management
Endotracheal intubation: Oral intubation by direct laryngoscopy - Airway management techniques
Endotracheal intubation
Oral intubation by direct
laryngoscopy
We
prefer to intubate the trachea when we need to have more control of the
patient’s airway, ventilate his lungs, and protect against aspiration of
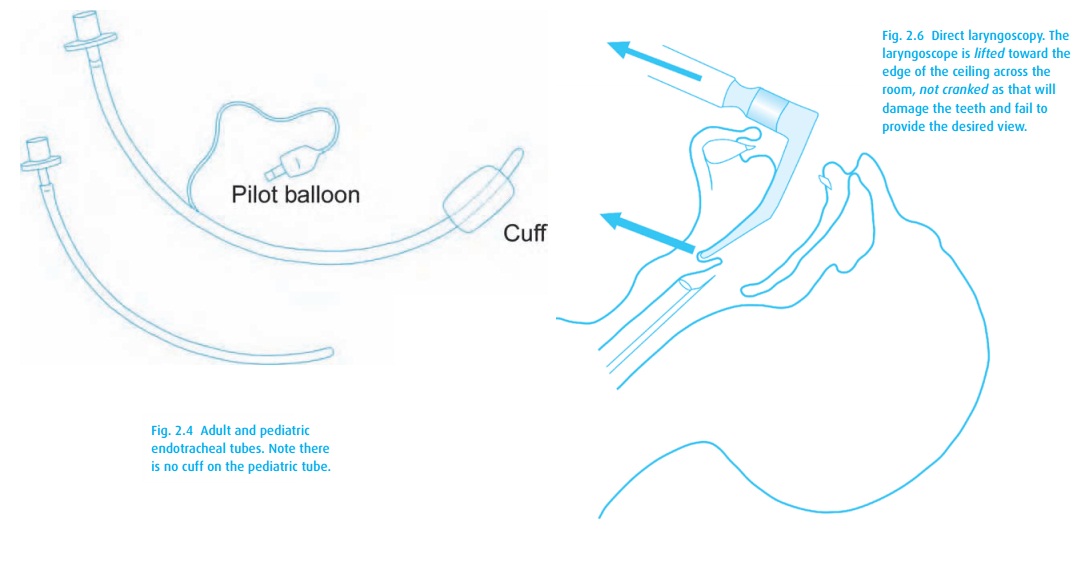
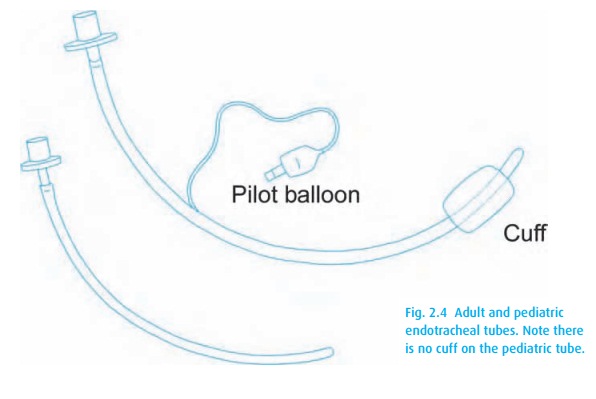
gastric con-tents. The use of a cuffed tracheal tube (Fig. 2.4) reduces the risk of aspiration in the adult.1 Our first step is to confirm all necessary
equipment is at hand:
·
a properly checked anesthesia machine, or a self-inflating bag or
Mapleson system with source of compressed oxygen, and a tight fitting mask;
·
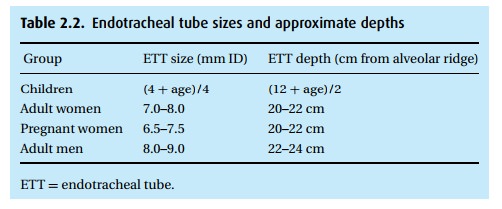
endotracheal tubes (ETT) of appropriate sizes (see Table 2.2). Generally we like to have an extra tube 1/2
size smaller than that anticipated . . . just in case;
·
a stylet that fits in the ETT – sometimes required to stiffen and
shape the tube;
·
a syringe to inflate the ETT cuff;
·
an oral airway, in case intubation and mask ventilation prove to be
difficult;
·
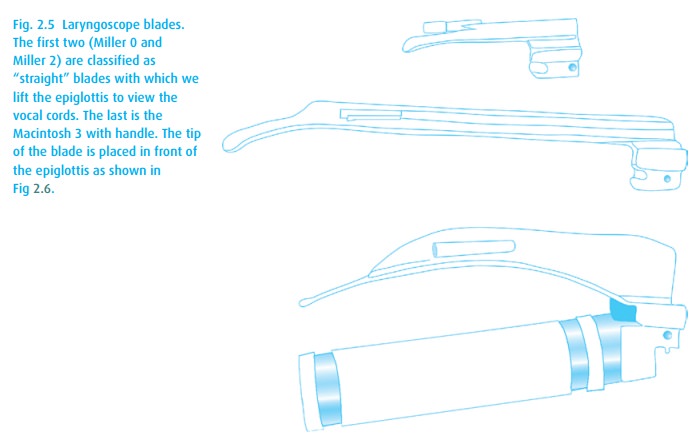
laryngoscope handle and appropriate blades (Fig. 2.5), usually at least a curved (Macintosh) and
straight (Miller), with confirmation that the light works!
·
suction – for the inevitable oral secretions and potential
regurgitation; induction drugs;?>
·
an assistant schooled in application of cricoid pressure: manual
pressure applied to the cricoid ring, compressing the esophagus against the
vertebral body beneath, in hope of preventing passive regurgitation.
The smooth placement of an endotracheal tube requires skill and practice. Usually we start with denitrogenating (pre-oxygenating) the patient’s lungs before ren-dering the patient unconscious and immobile (including paralysis of the muscles of respiration) for the intubation. If the patient cannot breathe and we are unable to ventilate his lungs, his life is in danger. Fortunately, we can usually identify those patients in whom conventional endotracheal intubation will be difficult. It is vitally important to recognize them before administering medications that induce apnea.
Intubation
is typically performed with direct visualization of the larynx, that is, we
like to watch the tube pass through
the vocal cords. Unfortunately, without an instrument such as the laryngoscope,
no direct line of sight exists through the open mouth to the larynx. Instead,
we must find a way to bring the larynx into view – enter “direct laryngoscopy.”
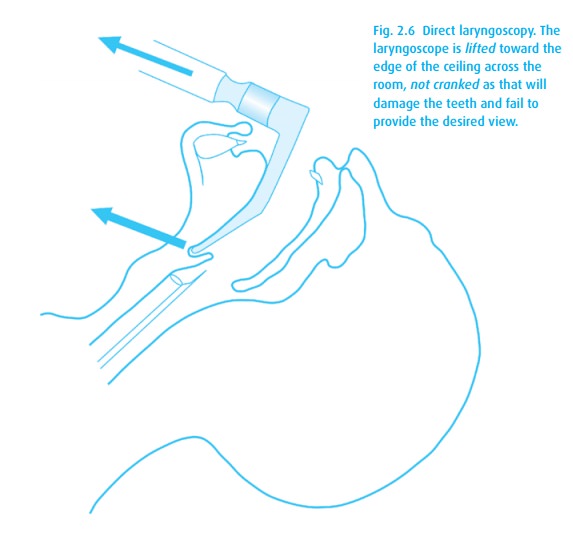
Here we position the patient’s head in the “sniffing position:” flexed at the
lower cervical spine and extended at the atlanto-occipital joint (see Fig. 2.6). Then we advance a laryngoscope to the level
of the epiglottis and use it to pull the lower jaw and tongue up and out of the
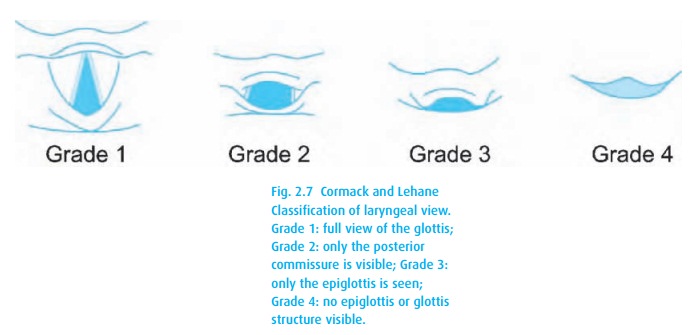
way, opening up a line of sight to the larynx (usually). The exposure of the
larynx varies and has been classified by Cormack and Lehane (Fig. 2.7).
Thus, to
intubate a patient with a “normal airway,” first position, denitrogenate
(pre-oxygenate), and induce the patient as described above, then proceed as
follows:
·
Take the laryngoscope in your left hand; the right hand is
responsible for everything else.
·
Place the right hand on top of the patient’s head and accentuate
neck exten-sion. Note that some prefer to perform a scissor-like maneuver with
the right thumb and index finger to open the patient’s jaw.
·
Advance the laryngoscope down the right side of the mouth to the
level of the tonsillar pillars. Sweep the tongue to the left as you bring the
laryngoscope to the midline.
·
With a straight blade, lift the epiglottis; with a curved blade,
place it at the base of the epiglottis. As above, lift forward and upward (in
the direction of the laryngoscope handle). Do not pry or crank with the
laryngoscope! Teeth might be broken.
·
When you can see the glottic opening clearly, grasp the
endotracheal tube (hold it like a pencil – not a dagger) with the right hand
(preferably without losing sight of the glottis), and advance the tip into the
trachea just until the cuff disappears completely beyond the vocal cords.
·
Inflate the cuff only to the point of no air leakage, and confirm trachealposition.
This
last point is very important.
Patients do not die from esophageal intubation; they die when esophageal
intubation is not recognized! You must be absolutely
sure the tube is in the right place! A fiberoptic bronchoscope that finds the
tip of the tube below the cords and above the carina would be ideal but is
impractical as a clinical routine. A chest radiograph, both PA and lateral,
confirming location in the trachea would also work, but is similarly
impractical for OR applications. Instead, we must use clinical clues and
technology.
i.
Confirmation of exhaled CO2 is the
gold standard, either
by quantitative capno-graphy as in the operating room, or the more mobile
colorimetric sensors. Note, however, that this only guarantees ventilation of
the lungs. It does notspecifically identify the ETT as placed in the trachea. Pharyngeal position of the tube
with ventilation (as with an LMA) may yield CO2. Conversely,
duringcardiovascular collapse, with minimal or no pulmonary blood flow, little
or no CO2 will be returned to the lungs from the periphery, and
end-tidal CO2 mightnot be measurable. Place a sensor anyway because
the return of detectable CO2 will indicate effective resuscitative
efforts and perfusion of the lungs.
ii.
Breath sounds While not definitive for tracheal placement,
breath soundsshould be present across the chest and absent over the stomach. We
can rule out endobronchial intubation when we hear good breath sounds
bilaterally. Emphasis on the bilaterally;
listening close to one side of the sternum, we often mistake breath sounds
transmitted from the other side.
iii.
Condensation While reassuring, condensation in the clear
plastic ETT duringexhalation is no ironclad guarantee either.
iv.
Palpation of the ETT cuff Still not flawless, but when combined with the
pres-ence of exhaled CO2, palpation of the cuff in the suprasternal
notch (notable by the bounce felt while squeezing the pilot balloon) does
confirm tracheal position.
v.
Chest excursion should be symmetric.
Related Topics