Chapter: Essential Anesthesia From Science to Practice : Clinical management : Airway management
Can’t intubate situations
Can’t intubate situations
Here the
hearts (of the caregivers) begin to pound . . . when the vocal cords cannot be
visualized. If this problem arises after adequate pre-oxygenation, you will
have won valuable time before serious hypoxemia ensues. The first thing we try
is to change the patient’s position, the laryngoscope blade, and/or the
laryngoscopist. If this does not help (and the patient is still apneic), then
another technique must be attempted (Table 2.3).
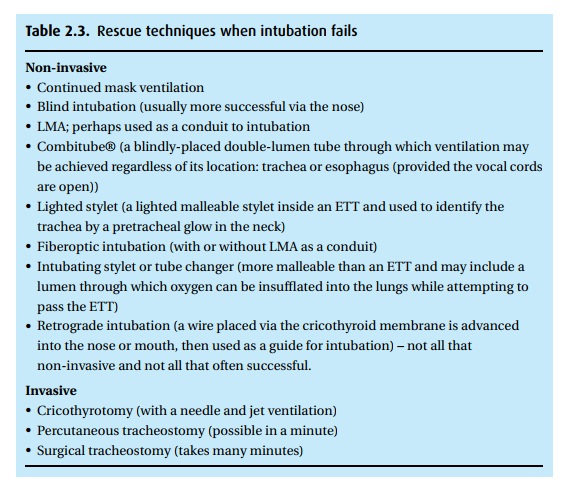
The
selection of rescue technique depends on the situation, experience of the
physician, availability of equipment, and whether mask–ventilation is possible.
For example, “can’t intubate, can’t ventilate” scenarios necessitate rapid
inter-vention, and thus, fiberoptic intubation would not be a likely choice for
an inex-perienced physician; placement of an LMA is much more likely to be
successful. Whereas in a “can’t intubate, can
ventilate” scenario, we may be able to mask– ventilate the patient’s lungs
while the surgeon does a tracheostomy or wait until the patient awakens and
then perform an awake fiberoptic intubation. Remem-ber that non-depolarizing
muscle relaxants cannot be reversed until the patient regains at least one
twitch on the train-of-four (ulnar stimulation), which may require 30 minutes
to more than an hour depending on the muscle relaxant and dose administered.
For this reason, we choose short-acting drugs, e.g., succinyl-choline, when we
anticipate difficulties: if intubation fails, the drug effect will wear off
within a few minutes, and the patient can once again breathe spontaneously.
Related Topics