Chapter: Medical Physiology: The Body Fluid Compartments: Extracellular and Intracellular Fluids; Interstitial Fluid and Edema
Edema: Excess Fluid in the Tissues
Edema: Excess Fluid in the Tissues
Edema refers to the presence of excess fluid in the body tissues. In most instances, edema occurs mainly in the extracellular fluid compartment, but it can involve intracellular fluid as well.
Intracellular Edema
Two conditions are especially prone to cause intracel-lular swelling: (1) depression of the metabolic systems of the tissues, and (2) lack of adequate nutrition to the cells. For example, when blood flow to a tissue is decreased, the delivery of oxygen and nutrients is reduced. If the blood flow becomes too low to main-tain normal tissue metabolism, the cell membrane ionic pumps become depressed. When this occurs, sodium ions that normally leak into the interior of the cell can no longer be pumped out of the cells, and the excess sodium ions inside the cells cause osmosis of water into the cells. Sometimes this can increase intra-cellular volume of a tissue area—even of an entire ischemic leg, for example—to two to three times normal. When this occurs, it is usually a prelude to death of the tissue.
Intracellular edema can also occur in inflamed tissues. Inflammation usually has a direct effect on the cell membranes to increase their permeability, allow-ing sodium and other ions to diffuse into the interior of the cell, with subsequent osmosis of water into the cells.
Extracellular Edema
Extracellular fluid edema occurs when there is excess fluid accumulation in the extracellular spaces. There are two general causes of extracellular edema: (1) abnormal leakage of fluid from the plasma to the inter-stitial spaces across the capillaries, and (2) failure of the lymphatics to return fluid from the interstitium back into the blood. The most common clinical cause of interstitial fluid accumulation is excessive capillary fluid filtration.
Factors That Can Increase Capillary Filtration
To understand the causes of excessive capillary filtra-tion, it is useful to review the determinants of capillary filtration. Mathematically, cap-illary filtration rate can be expressed as
Filtration = Kf x (Pc – Pif – πc + pif),
where Kf is the capillary filtration coefficient (the product of the permeability and surface area of the capillaries), Pc is the capillary hydrostatic pressure, πif is the interstitial fluid hydrostatic pressure, pc is the capillary plasma colloid osmotic pressure, and pif is the interstitial fluid colloid osmotic pressure. From this equation, one can see that any one of the followingchanges can increase the capillary filtration rate:
a.Increased capillary filtration coefficient.
b. Increased capillary hydrostatic pressure.
c. Decreased plasma colloid osmotic pressure.
Lymphatic Blockage Causes Edema
When lymphatic blockage occurs, edema can become especially severe because plasma proteins that leak into the interstitium have no other way to be removed. The rise in protein concentration raises the colloid osmotic pressure of the interstitial fluid, which draws even more fluid out of the capillaries.
Blockage of lymph flow can be especially severe with infections of the lymph nodes, such as occurs with infection by filaria nematodes. Blockage of the lymph vessels can occur in certain types of cancer or after surgery in which lymph vessels are removed or obstructed. For example, large numbers of lymph vessels are removed during radical mastectomy, impairing removal of fluid from the breast and arm areas and causing edema and swelling of the tissue spaces. A few lymph vessels eventually regrow after this type of surgery, so that the interstitial edema is usually temporary.
Summary of Causes of Extracellular Edema
A large number of conditions can cause fluid accumu-lation in the interstitial spaces by the abnormal leaking of fluid from the capillaries or by preventing the lym-phatics from returning fluid from the interstitium back to the circulation. The following is a partial list of con-ditions that can cause extracellular edema by these two types of abnormalities:
I. Increased capillary pressure
A.Excessive kidney retention of salt and water
Acute or chronic kidney failure
Mineralocorticoid excess
B.High venous pressure and venous constriction
Heart failure
Venous obstruction
Failure of venous pumps
Paralysis of muscles
Immobilization of parts of the body
Failure of venous valves
C.Decreased arteriolar resistance
Excessive body heat
Insufficiency of sympathetic nervous system
Vasodilator drugs
II.Decreased plasma proteins
A.Loss of proteins in urine (nephrotic syndrome)
B.Loss of protein from denuded skin areas
Burns
Wounds
C.Failure to produce proteins
Liver disease (e.g., cirrhosis)
Serious protein or caloric malnutrition
III. Increased capillary permeability
A.Immune reactions that cause release of histamine and other immune products
B.Toxins
C.Bacterial infections
D.Vitamin deficiency, especially vitamin C
E.Prolonged ischemia
F.Burns
IV. Blockage of lymph return
A.Cancer
B.Infections (e.g., filaria nematodes)
C.Surgery
D.Congenital absence or abnormality of lymphatic vessels
Edema Caused by Heart Failure. One of the most serious andmost common causes of edema is heart failure. In heart failure, the heart fails to pump blood normally from the veins into the arteries; this raises venous pressure and capillary pressure, causing increased capillary filtration. In addition, the arterial pressure tends to fall, causing decreased excretion of salt and water by the kidneys, which increases blood volume and further raises capil-lary hydrostatic pressure to cause still more edema. Also, diminished blood flow to the kidneys stimulates secretion of renin, causing increased formation of angiotensin II and increased secretion of aldosterone, both of which cause additional salt and water retention by the kidneys. Thus, in untreated heart failure, all these factors acting together cause serious generalized extra-cellular edema.
In patients with left-sided heart failure but without significant failure of the right side of the heart, blood is pumped into the lungs normally by the right side of the heart but cannot escape easily from the pulmonary veins to the left side of the heart because this part of the heart has been greatly weakened. Consequently, all the pulmonary vascular pressures, including pulmon-ary capillary pressure, rise far above normal, causing serious and life-threatening pulmonary edema. When untreated, fluid accumulation in the lungs can rapidly progress, causing death within a few hours.
Edema Caused by Decreased Kidney Excretion of Salt and Water.
As discussed earlier, most sodium chloride added to the blood remains in the extracellular compartment, and only small amounts enter the cells. Therefore, in kidney diseases that compromise urinary excretion of salt and water, large amounts of sodium chloride and water are added to the extracellular fluid. Most of this salt and water leaks from the blood into the interstitial spaces, but some remains in the blood. The main effects of this are to cause (1) widespread increases in interstitial fluid volume (extracellular edema) and (2) hypertension because of the increase in blood volume. As an example, children who develop acute glomerulonephritis, in which the renal glomeruli are injured by inflammation and therefore fail to filter adequate amounts of fluid, also develop serious extracellular fluid edema in the entire body; along with the edema, these children usually develop severe hypertension.
Edema Caused by Decreased Plasma Proteins. A reduction inplasma concentration of proteins because of either failure to produce normal amounts of proteins or leakage of proteins from the plasma causes the plasma colloid osmotic pressure to fall. This leads to increased capillary filtration throughout the body as well as extra-cellular edema.
One of the most important causes of decreased plasma protein concentration is loss of proteins in the urine in certain kidney diseases, a condition referred to as nephrotic syndrome. Multiple types of renal diseases can damage the membranes of the renal glomeruli, causing the membranes to become leaky to the plasma proteins and often allowing large quantities of these proteins to pass into the urine. When this loss exceeds the ability of the body to synthesize proteins, a reduc-tion in plasma protein concentration occurs. Serious generalized edema occurs when the plasma protein con-centration falls below 2.5 g/100 ml.
Cirrhosis of the liver is another condition that causesa reduction in plasma protein concentration. Cirrhosis means development of large amounts of fibrous tissue among the liver parenchymal cells. One result is failure of these cells to produce sufficient plasma proteins, leading to decreased plasma colloid osmotic pressure and the generalized edema that goes with this condition.
Another way that liver cirrhosis causes edema is that the liver fibrosis sometimes compresses the abdominal portal venous drainage vessels as they pass through the liver before emptying back into the general circulation. Blockage of this portal venous outflow raises capillary hydrostatic pressure throughout the gastrointestinal area and further increases filtration of fluid out of the plasma into the intra-abdominal areas. When this occurs, the combined effects of decreased plasma protein concentration and high portal capillary pres-sures cause transudation of large amounts of fluid and protein into the abdominal cavity, a condition referred to as ascites.
Safety Factors That Normally Prevent Edema
Even though many disturbances can cause edema, usually the abnormality must be severe before serious edema develops. The reason for this is that three major safety factors prevent excessive fluid accumulation in the interstitial spaces: (1) low compliance of the inter-stitium when interstitial fluid pressure is in the nega-tive pressure range, (2) the ability of lymph flow to increase 10- to 50-fold, and (3) washdown of inter-stitial fluid protein concentration, which reduces interstitial fluid colloid osmotic pressure as capillary filtration increases.
Safety Factor Caused by Low Compliance of the Interstitium in the Negative Pressure Range
We noted that interstitial fluid hydro-static pressure in most loose subcutaneous tissues of the body is slightly less than atmospheric pressure, averaging about –3 mm Hg. This slight suction in the tissues helps hold the tissues together. Figure 25–7 shows the approximate relations between different levels of interstitial fluid pressure and interstitial fluid volume, as extrapolated to the human being from animal studies. Note in Figure 25–7 that as long as the interstitial fluid pressure is in the negative range, small changes in interstitial fluid volume are associated with relatively large changes in interstitial fluid hydrostatic pressure. Therefore, in the negative pressure range, the compliance of the tissues, defined as the change involume per millimeter of mercury pressure change, is low.
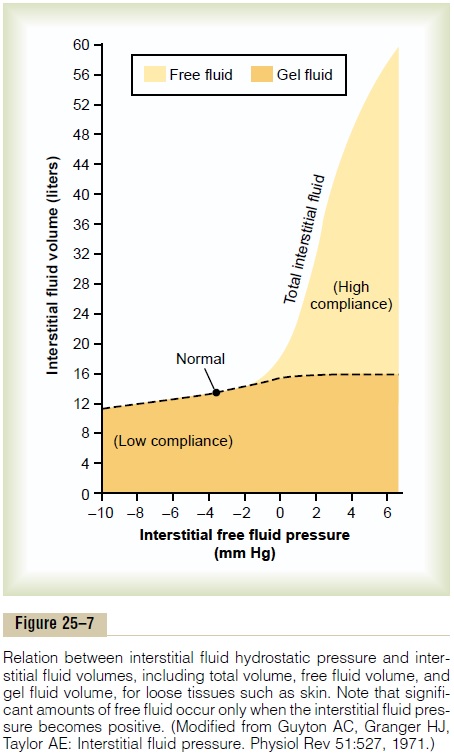
How does the low compliance of the tissues in the negative pressure range act as a safety factor against edema? To answer this question, recall the determi-nants of capillary filtration discussed previously. When interstitial fluid hydrostatic pressure increases, this increased pressure tends to oppose further capillary filtration. Therefore, as long as the interstitial fluid hydrostatic pressure is in the negative pressure range, small increases in interstitial fluid volume cause rela-tively large increases in interstitial fluid hydrostatic pressure, opposing further filtration of fluid into the tissues.
Because the normal interstitial fluid hydrostatic pressure is –3 mm Hg, the interstitial fluid hydrostatic pressure must increase by about 3 mm Hg before large amounts of fluid will begin to accumulate in the tissues. Therefore, the safety factor against edema is a change of interstitial fluid pressure of about 3 mm Hg.
Once interstitial fluid pressure rises above 0 mm Hg, the compliance of the tissues increases markedly, allowing large amounts of fluid to accumulate in the tissues with relatively small additional increases in interstitial fluid hydrostatic pressure. Thus, in the pos-itive tissue pressure range, this safety factor against edema is lost because of the large increase in compli-ance of the tissues.
Importance of Interstitial Gel in Preventing Fluid Accumulation in the Interstitium. Note in Figure 25–7 that in normaltissues with negative interstitial fluid pressure, virtually all the fluid in the interstitium is in gel form. That is, the fluid is bound in a proteoglycan meshwork so that there are virtually no “free” fluid spaces larger than a few hundredths of a micrometer in diameter. The impor-tance of the gel is that it prevents fluid from flowing easily through the tissues because of impediment from the “brush pile” of trillions of proteoglycan filaments. Also, when the interstitial fluid pressure falls to very negative values, the gel does not contract greatly because the meshwork of proteoglycan filaments offers an elastic resistance to compression. In the negative fluid pressure range, the interstitial fluid volume does not change greatly, regardless of whether the degree of suction is only a few millimeters of mercury negative pressure or 10 to 20 mm Hg negative pressure. In other words, the compliance of the tissues is very low in the negative pressure range.
By contrast, when interstitial fluid pressure rises to the positive pressure range, there is a tremendous accu-mulation of free fluid in the tissues. In this pressure range, the tissues are compliant, allowing large amounts of fluid to accumulate with relatively small additional increases in interstitial fluid hydrostatic pressure. Most of the extra fluid that accumulates is “free fluid” because it pushes the brush pile of proteoglycan filaments apart. Therefore, the fluid can flow freely through the tissue spaces because it is not in gel form. When this occurs, the edema is said to be pitting edema because one can press the thumb against the tissue area and push the fluid out of the area. When the thumb is removed, a pit is left in the skin for a few seconds until the fluid flows back from the surrounding tissues. This type of edema is distinguished from nonpitting edema, which occurs when the tissue cells swell instead of the interstitium or when the fluid in the interstitium becomes clotted with fibrinogen so that it cannot move freely within the tissue spaces.
Importance of the Proteoglycan Filaments as a “Spacer” for the Cells and in Preventing Rapid Flow of Fluid in the Tissues. Theproteoglycan filaments, along with much larger collagen fibrils in the interstitial spaces, act as a “spacer” between the cells. Nutrients and ions do not diffuse readily through cell membranes; therefore, without adequate spacing between the cells, these nutrients, electrolytes, and cell waste products could not be rapidly exchanged between the blood capillaries and cells located at a dis-tance from one another.
The proteoglycan filaments also prevent fluid from flowing too easily through the tissue spaces. If it were not for the proteoglycan filaments, the simple act of a person standing up would cause large amounts of inter-stitial fluid to flow from the upper body to the lower body. When too much fluid accumulates in the intersti-tium, as occurs in edema, this extra fluid creates large channels that allow the fluid to flow readily through the interstitium. Therefore, when severe edema occurs in the legs, the edema fluid often can be decreased by simply elevating the legs.
Even though fluid does not flow easily through the tissues in the presence of the compacted proteoglycan filaments, different substances within the fluid can diffuse through the tissues at least 95 per cent as easilyas they normally diffuse. Therefore, the usual diffusion of nutrients to the cells and the removal of waste prod-ucts from the cells are not compromised by the proteo-glycan filaments of the interstitium.
Increased Lymph Flow as a Safety Factor Against Edema
A major function of the lymphatic system is to return to the circulation the fluid and proteins filtered from the capillaries into the interstitium. Without this con-tinuous return of the filtered proteins and fluid to the blood, the plasma volume would be rapidly depleted, and interstitial edema would occur.
The lymphatics act as a safety factor against edema because lymph flow can increase 10- to 50-fold when fluid begins to accumulate in the tissues. This allows the lymphatics to carry away large amounts of fluid and proteins in response to increased capillary filtra-tion, preventing the interstitial pressure from rising into the positive pressure range. The safety factor caused by increased lymph flow has been calculated to be about 7 mm Hg.
“Washdown” of the Interstitial Fluid Protein as a Safety Factor Against Edema
As increased amounts of fluid are filtered into the interstitium, the interstitial fluid pressure increases, causing increased lymph flow. In most tissues, the protein concentration of the interstitium decreases as lymph flow is increased, because larger amounts of protein are carried away than can be filtered out of the capillaries; the reason for this is that the capillaries are relatively impermeable to proteins, compared with the lymph vessels. Therefore, the proteins are “washed out” of the interstitial fluid as lymph flow increases.
Because the interstitial fluid colloid osmotic pres-sure caused by the proteins tends to draw fluid out of the capillaries, decreasing the interstitial fluid proteins lowers the net filtration force across the capillaries and tends to prevent further accumulation of fluid. The safety factor from this effect has been calculated to be about 7 mm Hg.
Summary of Safety Factors That Prevent Edema
Putting together all the safety factors against edema, we find the following:
1. The safety factor caused by low tissue compliance in the negative pressure range is about 3 mm Hg.
2. The safety factor caused by increased lymph flow is about 7 mm Hg.
3. The safety factor caused by washdown of proteins from the interstitial spaces is about 7 mm Hg.
Therefore, the total safety factor against edema is about 17 mm Hg. This means that the capillary pres-sure in a peripheral tissue could theoretically rise by 17 mm Hg, or approximately double the normal value, before marked edema would occur.
Related Topics