Chapter: Biology of Disease: Disorders of the Gastrointestinal Tract, Pancreas, Liver and Gall Bladder
Disorders of the Stomach
DISORDERS OF THE STOMACH
Gastritis is the most common disorder affecting the stomach and
is character-ized by inflammation and erosion of the gastric mucosa. Gastritis
is idiopathic in many cases but it can be caused by irritating foods,
beverages, ingested poisons, aspirin and staphylococcal exotoxin . Gastritis
may present acutely where the patient suffers from GIT bleeding, epigastric
pain, that is pain on or over the stomach area, anorexia and hematemesis or
vomit-ing of blood. Patients with chronic gastritis may have no symptoms except
for epigastric pain. The possibility of exposure to irritating substances must
be determined when assessing the patient’s clinical history. Gastroscopy, in
which a tube with a camera on its end is passed into the stomach allowing a
direct visualization of its wall, can be used to confirm the diagnosis by
reveal-ing inflamed portions of the lining of the stomach. Relief from the symptoms
of gastritis occurs following removal of the irritant substance or treatment of
the underlying cause(s).
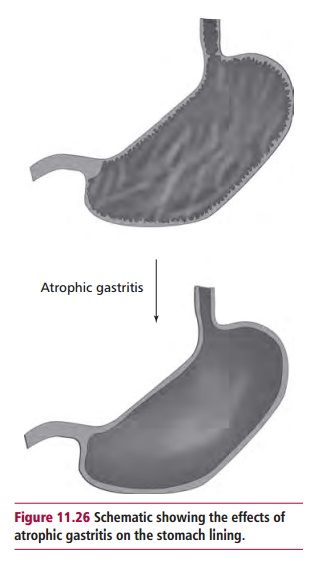
Atrophic gastritis is a degenerative stomach disorder
characterized by chronic inflammation of the stomach with atrophy of its mucous
membrane lining (Figure 11.26). This
results in loss of gastric glandular cells and their eventual replacement by
nonsecretory and fibrous tissues. Secretions of hydrochloric acid, pepsin and
intrinsic factor are impaired, leading to digestive problems, vitamin B12
deficiency and megaloblastic anemia. Atrophic gastritis is the result of
long-term damage to the gastric mucosa and is usually detected late in life. It
can be caused by persistent infection with the bacterium Helicobacterpylori but it can also have an autoimmune origin.
Helicobacter pylori is able to bind to the stomach
lining where the bacteriarelease urease, which hydrolyzes urea, releasing
ammonia that neutralizes the stomach acid. This allows the bacterium to
penetrate into the mucosal layer. The release of bacterial and inflammatory
toxic products by Helicobacter pylori
over time results in increasing gastric mucosal atrophy. Some glandular units
develop an intestinal-type epithelium; others are simply replaced by fibrous
tissue. The loss of gastric mucosa decreases the amount of acid secretion that
increases the gastric pH and leads to a reduced ability to kill bacteria.
Ingested bacteria can survive and reside in the stomach and the upper part of
the small intestine. Infection is usually acquired during childhood and, if
left untreated, progresses over the lifespan of the individual in one of two
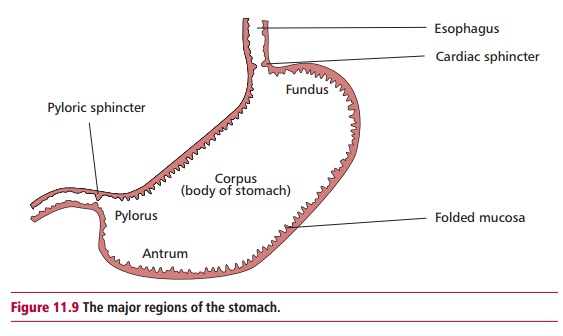
main ways that have different pathological consequences. The first is a
gastritis that mainly affects the antrum of the stomach (Figure 11.9). This is the most frequently observed pattern in
Western countries and individuals with peptic ulcers (seebelow) usually develop this pattern of gastritis. The second
pattern is a morewidespread atrophic gastritis affecting, for example, the
corpus, fundus and antrum with the loss of gastric glands and their partial
replacement by an intestinal-type epithelium. This pattern is observed more
often in developing countries and Asian individuals who develop gastric
carcinoma and gastric ulcers usually present with this pattern of gastritis.
Autoimmune gastritis is associated with serum anti-intrinsic
factor antibodies that reduce the amount of functioning intrinsic factor. This,
in turn, decreases the availability of vitamin B12 and eventually
leads to pernicious anemia in some patients. Cell-mediated immunity also
contributes to the disease because T cell lymphocytes infiltrate the gastric
mucosa and con-tribute to the epithelial cell destruction and resulting gastric
atrophy.
Specific data on the incidence of atrophic gastritis are scarse.
However, its prevalence mimics that of its two main causes. In both types,
atrophic gastri-tis develops over many years and is detected later in life. Helicobacter pylori (Figure 11.27) infects approximately 20%
of people younger than 40 years and 50% of those older than 60 years in the
developed world. Infection is highly prevalent in Asia and in developing
countries and it is estimated that 50% of the world’s population is infected.
Thus chronic gastritis is probably extremely common. In contrast, autoimmune
gastritis is a relatively rare condition, which is most frequently observed in
patients of northern European descent
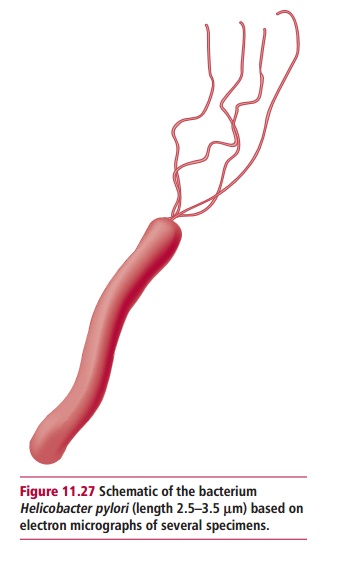
and in African Americans. The prevalence of pernicious anemia
resulting from autoimmune gastritis is estimated to be 127 in 100 000 in the
UK.
Chronic gastritis frequently is asymptomatic but can
present as nonspecific abdominal pain. Since gastritis often occurs in severely
ill, hospitalized peo-ple, its symptoms may be eclipsed by other, more severe
symptoms.
Atrophic gastritis cannot be reliably diagnosed by
gastroscopy but requires a microscopic examination of biopsy specimens. Helicobacter pylori infections are
normally diagnosed using serological tests, breath tests or antigen tests of
the feces. Pernicious anemia resulting from autoimmune atrophic gastritis
usually presents in patients approximately 60 years of age.
Treatment of atrophic gastritis is directed at
eliminating the causative agent, to correct complications of the disease and
attempt to revert the atrophic process. When Helicobacter pylori is the causative agent, it can be eradi-cated
using a combination of antimicrobial agents and antisecretory agents with a
success rate of about 90%. Lack of patient compliance and antimi-crobial
resistance are the most important factors influencing poor outcome. However,
treatment of Helicobacter pylori
infection may not lead to a reversal of existing damage unless started early
but may block further progression of the disease. Some evidence suggests that A-carotene and/or vitamins C and E
may reverse or reduce the risk of atrophic gastritis and/or gastric cancer. The
major complication in patients with autoimmune atrophic gastritis is the
development of pernicious anemia. This requires vitamin B12 replacement
therapy.

Ulcers are perforations of the GIT wall (Figure 11.28), particularly erosions of
the mucosal layer related to cancer, that is, malignant ulcers, or to stomach
acid, that is, peptic ulcers. Ulcers may also be named from their location, for
example esophageal, gastric or stomach and duodenal ulcers. Esophageal ulcers
are usually associated with hiatus hernias (see
below) caused by acid splashing from the stomach into the lower esophagus.
Gastric ulcers are rela-tively rare because the mucosal lining of the stomach
is protected from the acid by a layer of alkaline mucus. They generally occur
in patients older than 50 years of age. Duodenal ulcers are five times more
common than gastric ulcers and generally occur in a younger population. More than
90% of ulcers occur in the duodenal wall, usually after it has been weakened by
infection with Helicobacter pylori.
It used to be thought that ulcers were caused by stress and excessive
accumulation of HCl. However, it is now accepted that their commonest cause is
infection with Helicobacter pylori (Figure 11.27) which can colonize and
destroy the mucosal layer.
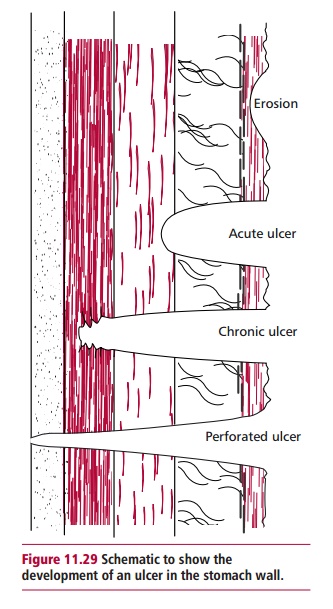
Peptic ulcers are linked to an increased production
of acid and pepsin in gastric juice or to a reduced protection of the mucosa
against gastric juice. Figure 11.29 illustrates
diagrammatically the development of a peptic ulcer.Lesions that do not extend through
the mucosal lining are referred to as ero-sions. Acute and chronic ulcers
penetrate this layer and, in serious cases, may penetrate the stomach wall. In
some patients, blood vessels in the GIT wall ulcerate and lead to heavy, and in
some cases fatal, bleeding. Chronic ulcers have an associated basal scarring.
Patients with peptic ulcers present with epigastric
pain but their diagnosis is made on clinical grounds, supported by endoscopy,
laboratory tests for assessing acid and pepsin secretion and identification of Helicobacter pylori infection. Treatment is aimed at eradication of
the Helicobacter pylori infec-tion
and reducing acid output. Antibiotics that effectively sup-press symptoms
include amoxycillin, clarithromycin, metronidazole and tetracycline, and they
often cure the patient. Bismuth chelate and sucralphate may also be
administered to decrease the synthesis of prostaglandins that stimulate
inflammation. The resulting decrease in acid production by parietal cells and
the increase in hydrogen carbonate production by mucus secreting epithelial
cells have cytoprotective effects.
Zollinger-Ellison syndrome is a rare disorder that
causes massive, multiple and recurrent peptic ulcers due to the excessive
secretion of gastric juice from tumors affecting the pancreas or duodenum.
Approximately 60% of the tumors are malignant. They are called gastrinomas
because they secrete large amounts of gastrin, hence patients have an increased
plasma gastrin concen-tration and rates of gastric acid secretion greater than
100 compared with nor-mal rates of less than 5 mmol h–1.
A diagnosis of Zollinger-Ellison syndrome usually
requires demonstrating an increase in the concentration of gastrin in the
patient’s serum, combined with an increased release of acid in the stomach.
However, in about 30% of cases the plasma gastrin concentration is normal or
only slightly above normal. The pentagastrin test is used to assess the acid
output of the stomach. Pentagastrin is an analog of gastrin that stimulates the
release of stomach acid. Acid output is assessed before and after intramuscular
injection of pentagastrin. Patients with Zollinger-Ellison syndrome have a high
basal acid output and pentagas-trin causes little further increase. Treatment
of Zollinger-Ellison syndrome is by surgical removal of the gastrinoma.
A hernia
is the protrusion of an organ or tissue out of the body cavity in which it is
normally found. A hiatus hernia occurs when the upper part of the stom-ach is
dislocated through the hole, called a hiatus, in the diaphragm, into the chest.
Sliding hiatus hernias occur when the esophagus and stomach both move upwards
so that the top end of the stomach protrudes through the gap in the diaphragm
normally occupied by the esophagus (Figure
11.30 (A)) and these constitute
90% of cases. The remaining 10% are rolling hiatus hernias where a portion of
the stomach curls upwards adjacent to the esophagus so that both it and an
upper part of the stomach protrude through the gap (Figure 11.30 (B)). The
causes of hiatus hernias are unknown but they may be due to intra-abdominal
pressure or weakening of the gastroesophageal junc-tion caused by trauma or
loss of muscle tone. Over 50% of individuals with hiatus hernia are
asymptomatic, but when symptoms do occur, they include heartburn, which is
aggravated by reclining, chest pain, dysphagia, belching, pain on swallowing
hot fluids and a feeling of food sticking in the esophagus. Although hiatus
hernia is not usually serious, it can cause inflammation of the lower end of
the esophagus leading to a back flow of gastric juices; this is called reflux esophagitis, and it may cause
bleeding (perhaps anemia) or a stricture. Cancer in a hiatus hernia is very
rare, but there is a slight increased risk of it developing in the inflamed
area.

Data on the incidence of hiatus hernia are few but
the condition increases with age and is particularly common in overweight
middle-aged women and can also occur during pregnancy. The contents of the GIT
are often not clearly visible by X-rays and diagnosis requires confirmation
with a barium meal. This consists of barium sulfate mixed with liquid and is
usually flavored. The barium in the meal lines the inside of the GIT wall and
is visible because barium is opaque to X-rays making this a useful method for
detecting structural abnormalities of the GIT. The presence of a hiatus hernia
can also be investigated by gastroscopy.
The aim of treatment is to alleviate the symptoms.
Losing weight, reduc-ing smoking and coffee and alcohol intakes all help to
relieve symptoms. The patient may be advised to avoid tight or restrictive
clothing. Avoiding food intake before sleep and elevating the head of the bed
help in reducing acid reflux. Medication such as antacids may be prescribed.
Surgery is only used when there is strangulation of the hernia or the symptoms
cannot be controlled.
Related Topics