Chapter: Clinical Anesthesiology: Anesthetic Management: Obstetric Anesthesia
Anesthetic Risk in Obstetric Patients
ANESTHETIC RISK IN OBSTETRIC PATIENTS
Although the majority of women of
childbearing age are healthy and would be considered to be at mini-mal
operative risk, pregnancy, certain maternal– fetal factors, and preexisting
medical conditions significantly increase surgical and obstetric risks.
Maternal Mortality
Maternal mortality is usually presented as the number of women who die
while pregnant (or within 42 days of pregnancy termination) after excluding
accidents and unrelated causes. This number is often indexed to the total
number of live births. The maternal mortality index has decreased nearly
100-fold since 1900. Likely due to better reporting, it rose slightly in the
United States to 21 deaths per 100,000 live births in 2010. The world average
is 400 deaths per 100,000 live births. Of all maternal deaths worldwide, 99%
occur in Africa, Asia, Latin America, and the Caribbean.
In the United States, overall mortality risk is greater for women older
than 35 years of age, black women, and women who do not receive prenatal care.
The leading causes of death associated with a live birth in 2010 were
cardiovascular diseases (13.5%), cardiomyopathy (12.6%), hemorrhage (11.9%), noncardiovascular diseases (11.8%), hyper-tensive disorders of
pregnancy (11.1%), infection/ sepsis (11.1%), thrombotic pulmonary embolism
(5.6%), amniotic fluid embolism (5.6%), cerebro-vascular accidents (5.3%) and
anesthesia compli-cations (0.6%) Of all maternal deaths, only 34% of patients
died within 24 h of delivery, whereas 55% died between 1 and 42 days, and
another 11% died between 43 days and 1 year. Direct causes of mater-nal deaths
are more clearly detailed from Canadian data, which show that, in addition to
pulmonary embolism and preeclampsia/pregnancy-induced hypertension (PIH),
amniotic fluid embolism and intracranial hemorrhage emerge as important
addi-tional causes of death.
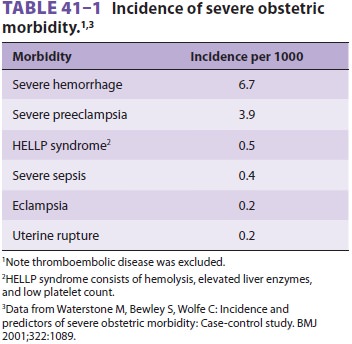
Severe obstetric morbidity may be a more
sensi-tive measure of outcome than maternal mortality. Data from the United
Kingdom suggest that inci-dence of severe obstetric morbidity is 12 per 1000
deliveries, 100 times more common than mortality. Risk factors include age
greater than 34 years, non-white ethnic group, multiple pregnancy, history of
hypertension, previous postpartum hemorrhage, and emergency cesarean delivery. Table
41–1 lists the estimated incidence of the most
common causes of severe morbidity; thromboembolic disease was deliberately
excluded because of the difficulty
In making the diagnosis in nonfatal cases. By
far the most common morbidities encountered in obstetrics are severe hemorrhage
and severe preeclampsia.
Anesthetic Mortality
Anesthesia accidents and mishaps account for approximately 2–3% of
maternal deaths. Data col-lected between 1985 and 1990 suggested a maternal
mortality of 32 deaths per 1,000,000 live births due to general anesthesia and
1.9 deaths per 1,000,000 live births due to regional anesthesia. More recent
data between 1998 and 2005 suggest a lower over-all maternal mortality from
anesthesia (about 1.2 % of live births), possibly due to greater use of
regional anesthesia for labor and cesarean delivery. Most deaths occur during
or after cesarean section. Moreover, the risk of an adverse outcome appears to
be much greater with emergent than with elective cesarean sections.
Obstetric Anesthesia Closed Claims
Obstetric anesthesia care accounts for approx-imately 12% of the
American Society of Anesthesiologists (ASA) Closed Claims database claims. A
comparison of obstetric anesthesia claims from 1990 to 2003 or with pre-1990
claims shows a decrease in maternal deaths, as well as a decrease in
respiratory-damaging events (aspi-ration, difficult intubation, esophageal
intuba-tion, and inadequate oxygenation/ventilation). Although newborn deaths
and brain damage also decreased over this period, they remained a leading cause
of obstetric anesthesia malpractice claims. Maternal nerve injury was more
common in claims reported after 1990 compared with ear-lier years.
Related Topics