Chapter: Clinical Anesthesiology: Anesthetic Management: Obstetric Anesthesia
Anesthesia for Fetal Resuscitation
FETAL RESUSCITATION
Resuscitation of the neonate starts during
labor. Any compromise of the uteroplacental circulation readilyproduces fetal
asphyxia. Intrauterine asphyxia during labor is the most common cause of
neonatal depression. Fetal monitoring throughout labor is helpful in
identifying which babies may be at risk, detecting fetal distress, and
evaluating the effect of acute interventions. These include correcting
mater-nal hypotension with fluids or vasopressors, supple-mental oxygen, and
decreasing uterine contraction (stopping oxytocin or administering tocolytics).
Some studies suggest that the normal fetus can compensate for up to 45 min of
relative hypoxia, a period termed fetal stress; the latter is associated with a
marked redis-tribution of blood flow primarily to the heart, brain, and adrenal
glands. With time, however, progressive lactic acidosis and asphyxia produce
increasing fetal distress that necessitates immediate delivery.
1. Fetal Heart Rate Monitoring
Monitoring of fetal heart rate (FHR) is presently
the most useful technique in assessing fetal well-being, although alone it has
a 35–50% false-positive rate of predicting fetal compromise. Because of this,
the term fetal distress in the
context of FHR monitoring has been largely replaced with nonreassuring FHR. Correct interpretation of heart rate patterns is
cru-cial. Three parameters are evaluated: baseline heart rate, baseline
variability, and the relationship to uter-ine contractions (deceleration
patterns). Monitoring of heart rate is most accurate when fetal scalp
elec-trodes are used, but this may require rupture of the membranes and is not
without complications (eg, amnionitis or fetal injury).
Baseline Heart Rate
The mature fetus normally has a baseline
heart rate of 110–160 beats/min. An increased baseline heart rate may be due to
prematurity, mild fetal hypoxia, chorio-amnionitis, maternal fever, maternally
administered drugs (anticholinergics or β agonists), or, rarely, hyperthyroidism. A decreased baseline heart rate
may be due to a postterm pregnancy, fetal heart block, or fetal asphyxia.
Baseline Variability
The healthy mature fetus normally displays a base-line beat-to-beat (R
wave to R wave) variability that can be classified as minimal (<5 beats/min), mod-erate (6–25
beats/min), or marked (>25
beats/min). Baseline variability, which is best assessed with scalp electrodes,
has become an important sign of fetal well-being and represents a normally
functioning autonomic system. Sustained
decreased baseline variability is a prominent sign of fetal asphyxia. Central
nervous system depressants (opioids, bar-biturates, volatile anesthetics,
benzodiazepines, or magnesium sulfate) and parasympatholytics (atro-pine) also
decrease baseline variability, as do pre-maturity, fetal arrhythmias, and
anencephaly. A sinusoidal pattern that resembles a smooth sine wave is
associated with fetal depression (hypoxia, drugs, and anemia secondary to Rh
isoimmunization).
Accelerations
Accelerations of FHR are defined as increases
of 15 beats/min or more lasting for more than 15 s. Periodic accelerations in
FHR reflect normal oxy-genation and are usually related to fetal movements and
to responses to uterine pressure. Such accel-erations are generally considered
reassuring. By 32 weeks, fetuses display periodic increases in base-line heart
rate that are associated with fetal move-ments. Normal fetuses have 15–40
accelerations/h. The mechanism is thought to involve increases in catecholamine
secretion with decreases in vagal tone. Accelerations diminish with fetal
sleep, some drugs (opioids, magnesium, and atropine), as well as fetal hypoxia.
Accelerations to fetal scalp or vibro-acoustic stimulation are considered a reassuring
sign of fetal well-being. The absence of both baseline variability and
accelerations is nonreassuring and may be an important sign of fetal
compromise.
Deceleration Patterns
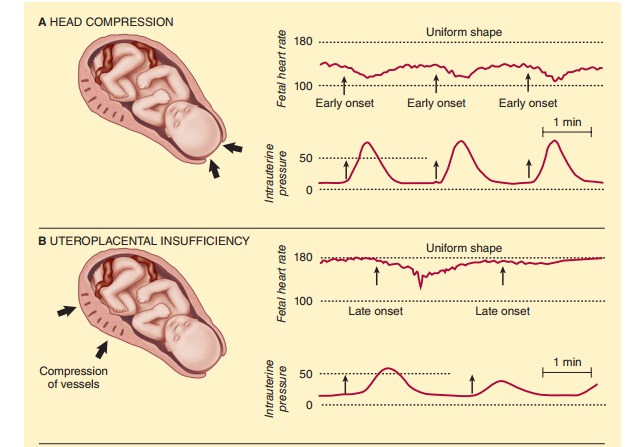
A. Early (Type I) Decelerations
Early deceleration (usually 10–40 beats/min) (Figure
41–4A) is thought to be a vagal response
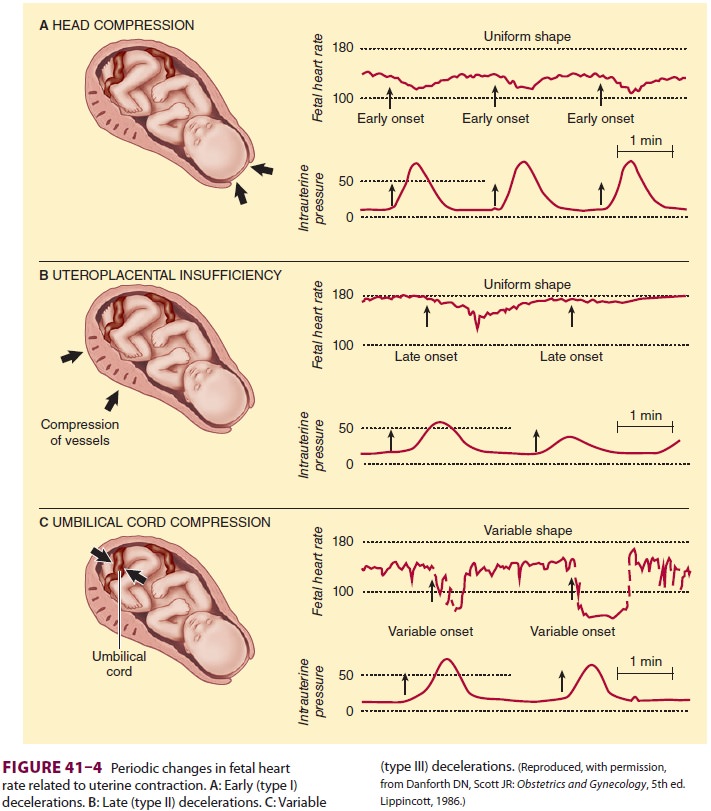
to compression of the fetal head or
stretching of the neck during uterine contractions. The heart rate forms a
smooth mirror image of the contraction. Early decelerations are generally not
associated with fetal distress and occur during descent of the head.
B. Late (Type II) Decelerations
Late decelerations (Figure
41–4B) are associated with fetal compromise and
are characterized by a decrease in heart rate at or following the peak of
uterine contractions. Late decelerations may be subtle (as few as 5 beats/min).
They are thought to represent decreased arterial oxygen tension on atrial
chemoreceptors. Late decelerations with nor-mal variability may be observed
following acute insults (maternal hypotension or hypoxemia) and are usually
reversible with treatment. Late decelera-tions with decreased variability are
associated with prolonged asphyxia and may be an indication for fetal scalp
sampling (see Other Monitoring section). Complete abolition of variability in
this set-ting is an ominous sign signifying severe decompen-sation and the need
for immediate delivery.
C. Variable (Type III) Decelerations
The most common type of decelerations are
variable (Figure 41–4C). These decelerations
are variable in onset, duration, and magnitude (often >30 beats/ min). They are typically abrupt in
onset and are thought to be related to umbilical cord compression and acute
intermittent decreases in umbilical blood flow. Variable decelerations are
typically associated with fetal asphyxia when fetal heart rate declines to less
than 60 beats/min, last more than 60 s, or occur in a pattern that persists for
more than 30 min.
2. Other Monitoring
Other less commonly used monitors include fetal
scalp pH measurements, scalp lactate concentration, fetal pulse oximetry, and
fetal ST-segment analysis. Clinical experience is limited with all except fetal
scalp pH measurements. Unfortunately the latter is associated with a small but
significant incidence of false negatives and false positives. Fetal blood can
be obtained and analyzed via a small scalp puncture once the membranes are
ruptured. A fetal scalp pH higher than 7.20 is usually associated with a
vigor-ous neonate, whereas a pH less than 7.20 is often, but not always,
associated with a depressed neonate and necessitates prompt (typically
operative) delivery. Because of wide overlap, fetal blood sampling can be
interpreted correctly only in conjunction with heart rate monitoring.
3. Treatment of the Fetus
Treatment of intrauterine fetal asphyxia is aimed at preventing fetal
demise or permanent neurological damage. All interventions
are directed at restoring an adequate uteroplacental circulation. Aortocaval
compression, maternal hypoxemia or hypoten-sion, or excessive uterine activity
(during oxytocin infusions) must be corrected. Changes in maternal position,
supplemental oxygen, and intravenous ephedrine or fluid, or adjustments in an
oxytocin infusion often correct the problem. Failure to relieve fetal stress,
as well as progressive fetal acidosis and asphyxia, necessitate immediate
delivery.
Related Topics