Chapter: Essentials of Anatomy and Physiology: Heart
Anatomy of the Heart
ANATOMY OF THE HEART
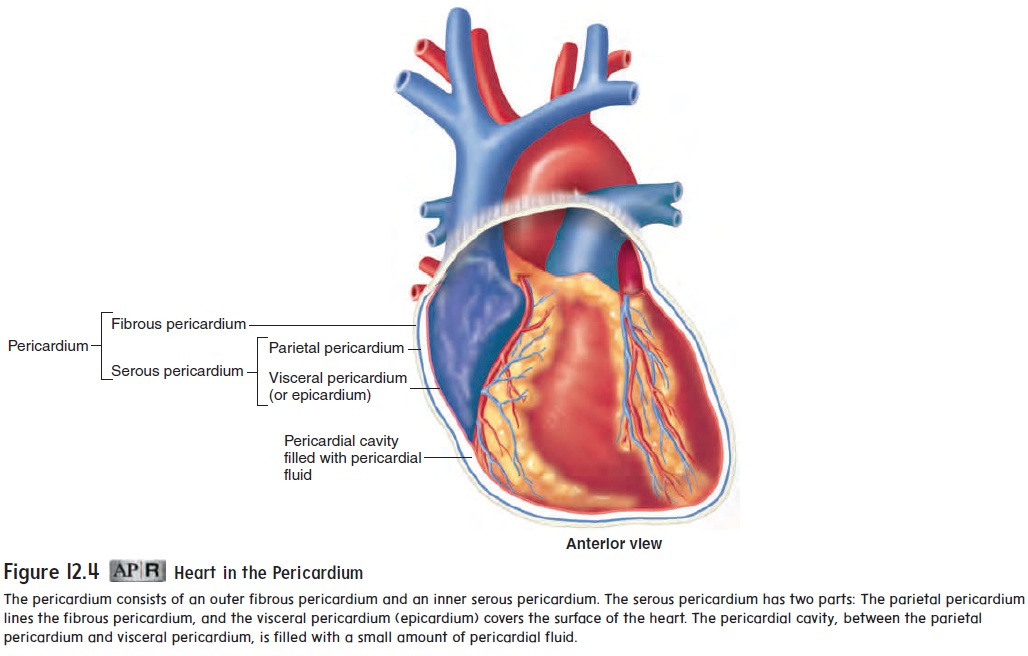
Pericardium
The heart lies in the pericardial cavity. The pericardial cavity is formed by the pericardium (per-i-kar′ d̄e -̆u m), or pericardial sac, tissues that surround the heart and anchor it within the mediasti-num (figure 12.4). The pericardium consists of two layers. The tough, fibrous connective tissue outer layer is called the fibrouspericardium, and the inner layer of flat epithelial cells, with a thinlayer of connective tissue, is called the serous pericardium. The portion of the serous pericardium lining the fibrous pericardium is the parietal pericardium, whereas the portion covering the heart surface is the visceral pericardium, or epicardium (ep-i-kar′ d̄e - ̆u m; upon the heart). The parietal and visceral pericardia are continuous with each other where the great vessels enter or leave the heart. The pericardial cavity, located between the visceral and parietal pericardia, is filled with a thin layer of pericardial fluid produced by the serous pericardium. The pericardial fluid helps reduce friction as the heart moves within the pericardium.
External anatomy
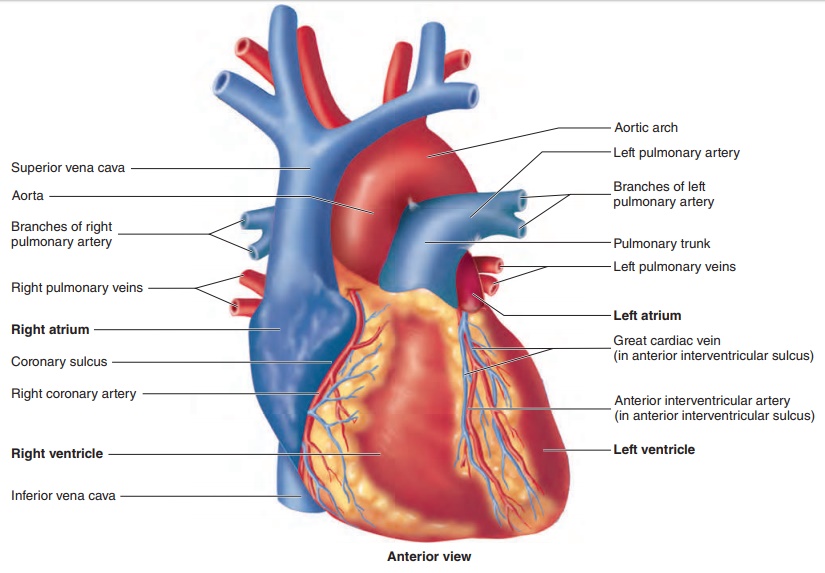
The right and left atria (a′ trē - ă ; sing. atrium, entrance chamber) are located at the base of the heart, and the right and left ven-tricles (ven′tri-klz; cavities) extend from the base of the heart
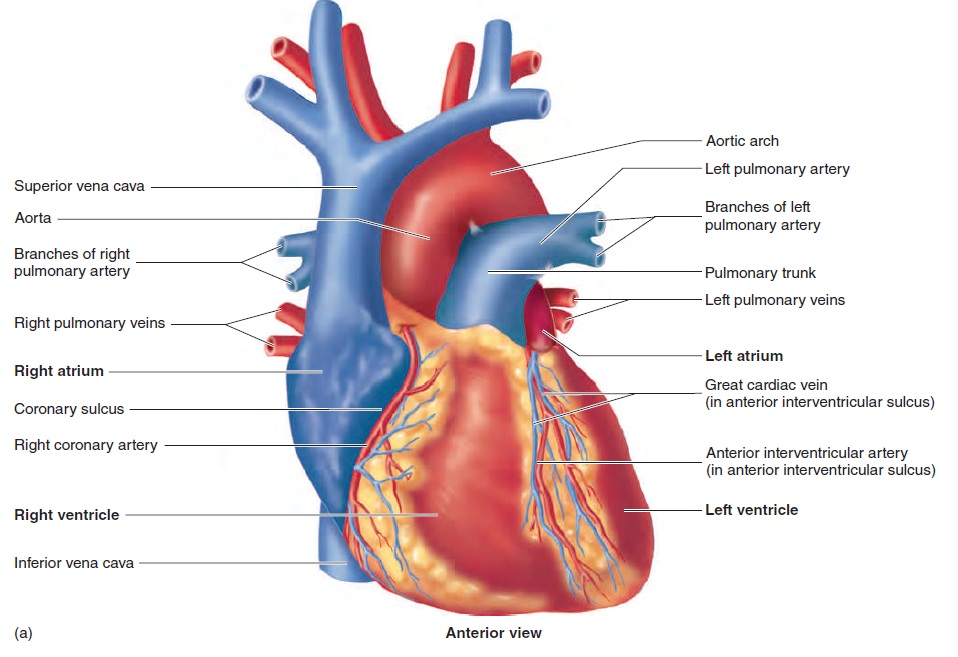
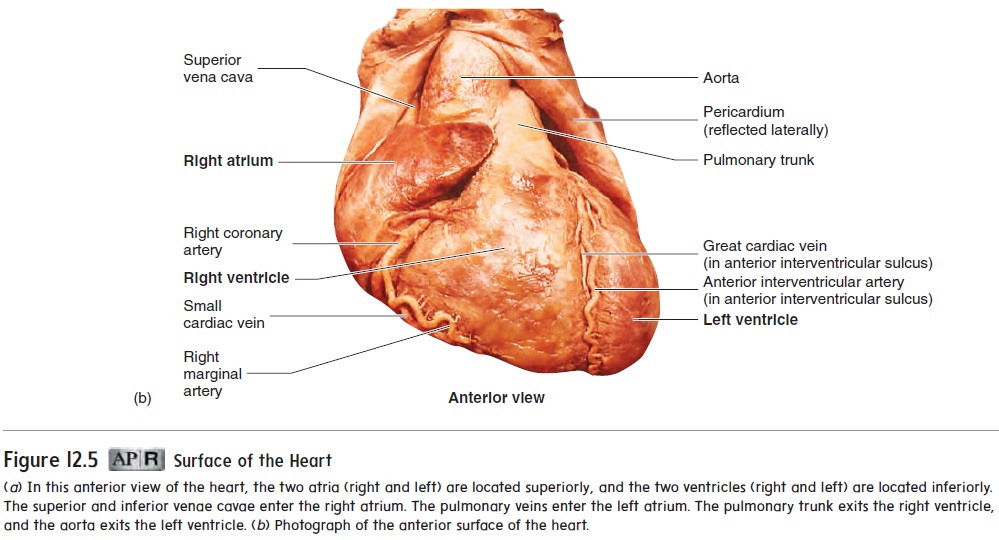
A coronary (k r′ o-n r- ) sulcus (sool′ kus) extends around the heart, separating the atria from the ventricles. In addition, two grooves, or sulci, which indicate the division between the right and left ventricles, extend inferiorly from the coronary sulcus. The anterior interventricular sul-cus extends inferiorly from the coronary sulcus on the anteriorsurface of the heart, and theposterior interventricular sulcusextends inferiorly from the coronary sulcus on the posterior sur-face of the heart.
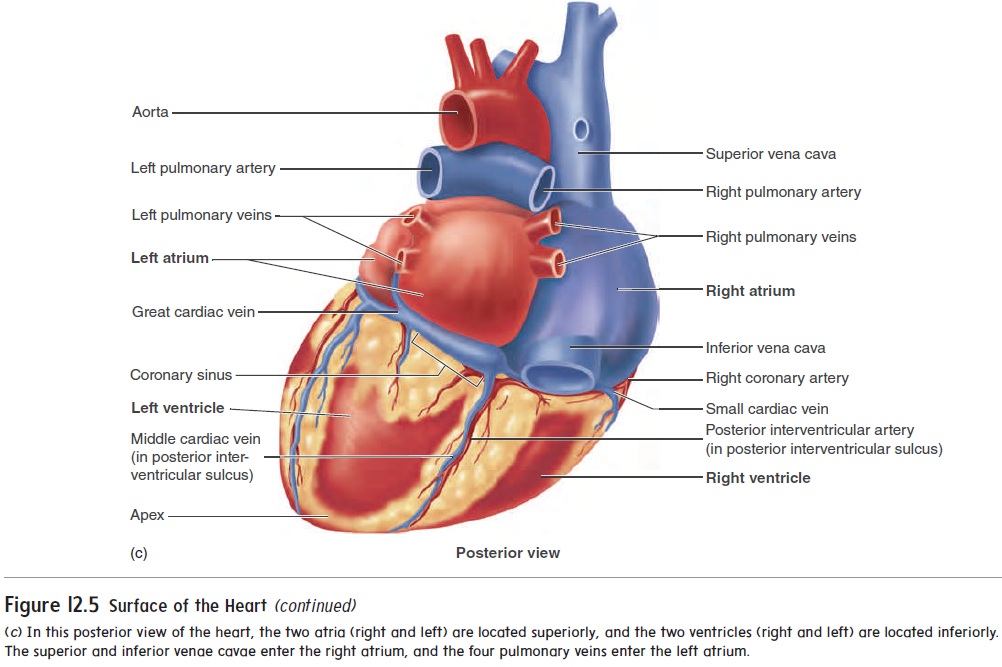
Six large veins carry blood to the heart (figure 12.5a,c): The superior vena cava and inferior vena cava carry blood fromthe body to the right atrium, and four pulmonary (p l′ m -n r- ; lung) veins carry blood from the lungs to the left atrium. Two arteries, the pulmonary trunk and the aorta ( - r′ t ), exit the heart.
The pulmonary trunk, arising from the right ventricle, splits into the right and left pulmonary arteries, which carry blood to the lungs. The aorta, arising from the left ventricle, carries blood to the rest of the body.
Heart chambers and internal anatomy
The heart is a muscular pump consisting of four chambers: the right and left atria and the right and left ventricles (figure 12.6).
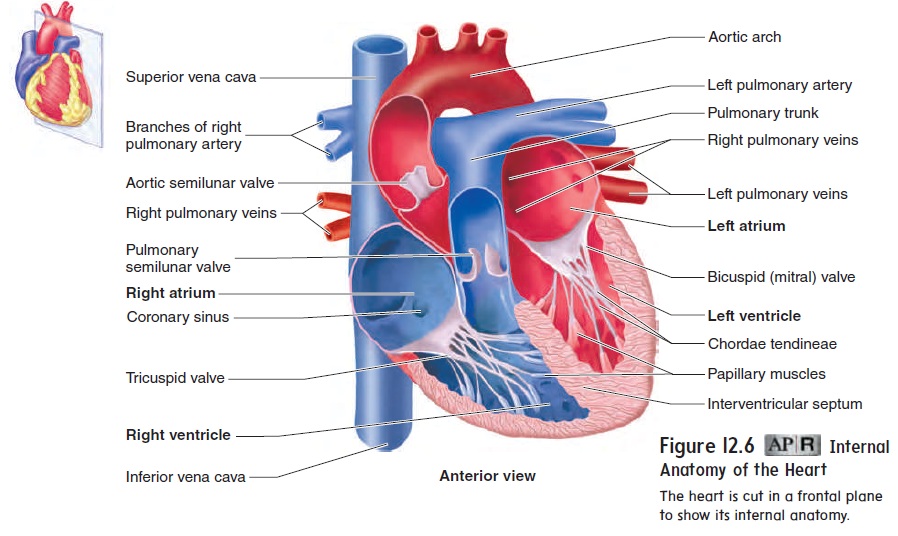
Right and Left Atria
The atria of the heart receive blood from veins. The atria function primarily as reservoirs, where blood returning from veins collects before it enters the ventricles. Contraction of the atria forces blood into the ventricles to complete ventricular filling. The right atrium receives blood through three major openings. The superior vena cava and the inferior vena cava drain blood from most of the body (figure 12.6), and the smaller coronary sinus drains blood from most of the heart muscle. The left atrium receives blood through the four pulmonary veins, which drain blood from the lungs. The two atria are separated from each other by a partition called the interatrial (between the atria) septum.
Right and Left Ventricles
The ventricles of the heart are its major pumping chambers. They eject blood into the arteries and force it to flow through the circulatory system. The atria open into the ventricles, and each ventricle has one large outflow route located superiorly near the midline of the heart. The right ventricle pumps blood into the pul-monary trunk, and the left ventricle pumps blood into the aorta. The two ventricles are separated from each other by the muscular interventricular (between the ventricles) septum (figure 12.6).
The wall of the left ventricle is thicker than the wall of the right ventricle, and the wall of the left ventricle contracts more forcefully and generates a greater blood pressure than the wall of the right ventricle. When the left ventricle contracts, the pressure increases to approximately 120 mm Hg. When the right ventricle contracts, the pressure increases to approximately one-fifth of the pressure in the left ventricle. However, the left and right ventricles pump nearly the same volume of blood. The higher pressure generated by the left ventricle moves blood through the larger systemic circulation, whereas the lower pressure generated by the right ventricle moves blood through the smaller pulmonary circulation (see figure 12.2).
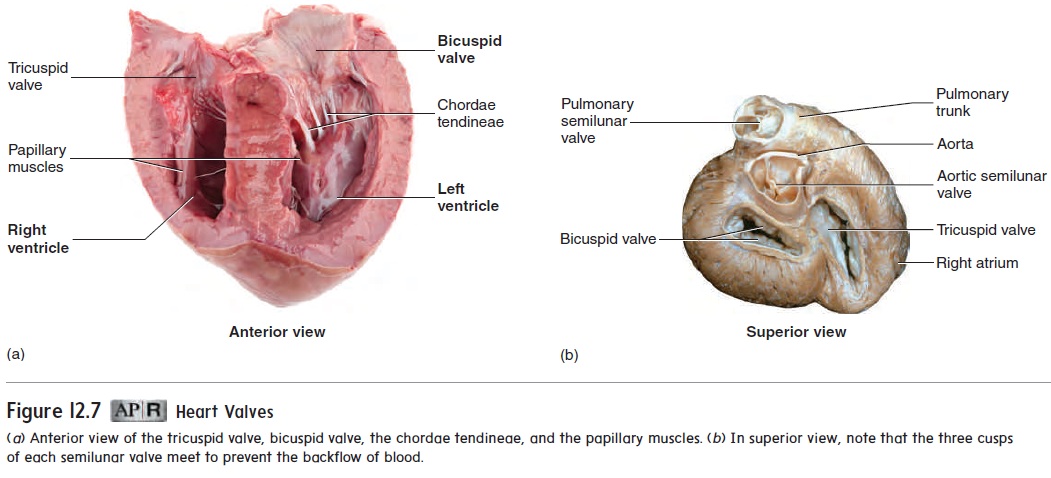
Heart valves
The atrioventricular (AV) valves are located between the right atrium and the right ventricle and between the left atrium and the left ventricle. The AV valve between the right atrium and the right ventricle has three cusps and is called the tricuspid valve (figure 12.7a). The AV valve between the left atrium and the left ventricle has two cusps and is called the bicuspid valve or mitral (resembling a bishop’s miter, a two-pointed hat) valve (figure 12.7b). These valves allow blood to flow from the atria into the ventricles but prevent it from flowing back into the atria. When the ventricles
relax, the higher pressure in the atria forces the AV valves to open, and blood flows from the atria into the ventricles (figure 12.8a). In contrast, when the ventricles contract, blood flows toward the atria and causes the AV valves to close (figure 12.8b).
Each ventricle contains cone-shaped, muscular pillars called papillary (pap′-l̄ar-ē) muscles. These muscles are attached bythin, strong, connective tissue strings called chordae tendineae (kō r′ dē ten′ di-nē -ē ; heart strings) to the free margins of the cusps of the atrioventricular valves. When the ventricles contract, the papillary muscles contract and prevent the valves from opening into the atria by pulling on the chordae tendineae attached to the valve cusps (see figures 12.6 and 12.7a; figure 12.8).
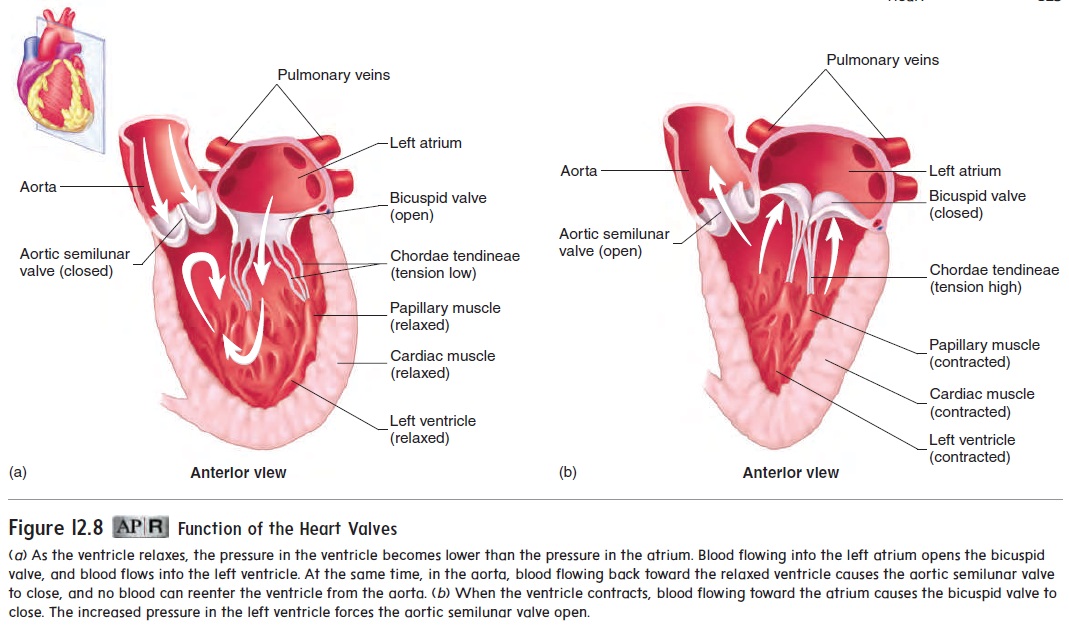
The aorta and pulmonary trunk possess aortic and pulmonarysemilunar valves, respectively (see figure 12.6). Each valve consistsof three pocketlike semilunar (half-moon-shaped) cusps (see fig-ure 12.7b; figure 12.8). When the ventricles relax, the pressures in the aorta and pulmonary trunk are higher than in the ventricles. Blood flows back from the aorta or pulmonary trunk toward the ventricles and enters the pockets of the cusps, causing them to bulge toward and meet in the center of the aorta or pulmonary trunk, thus closing the vessels and blocking blood flow back into the ventricles (figure 12.8a). When the ventricles contract, the increasing pressure within the ventricles forces the semilunar valves to open (figure 12.8b).
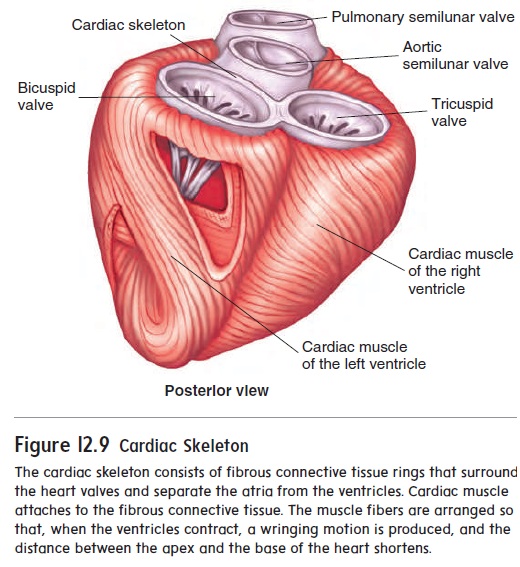
A plate of connective tissue, sometimes called the cardiacskeleton, consists mainly of fibrous rings that surround the atrio-ventricular and semilunar valves and give them solid support (figure 12.9). This connective tissue plate also serves as electrical insulation between the atria and the ventricles and provides a rigid attachment site for cardiac muscle.
Route Of Blood Flow Through The Heart
The route of blood flow through the heart is depicted in figure 12.10. Even though blood flow is described for the right and then the left side of the heart, it is important to understand that both atria contract at the same time, and both ventricles contract at the same time. This concept is most important when considering the electrical activity, pressure changes, and heart sounds.
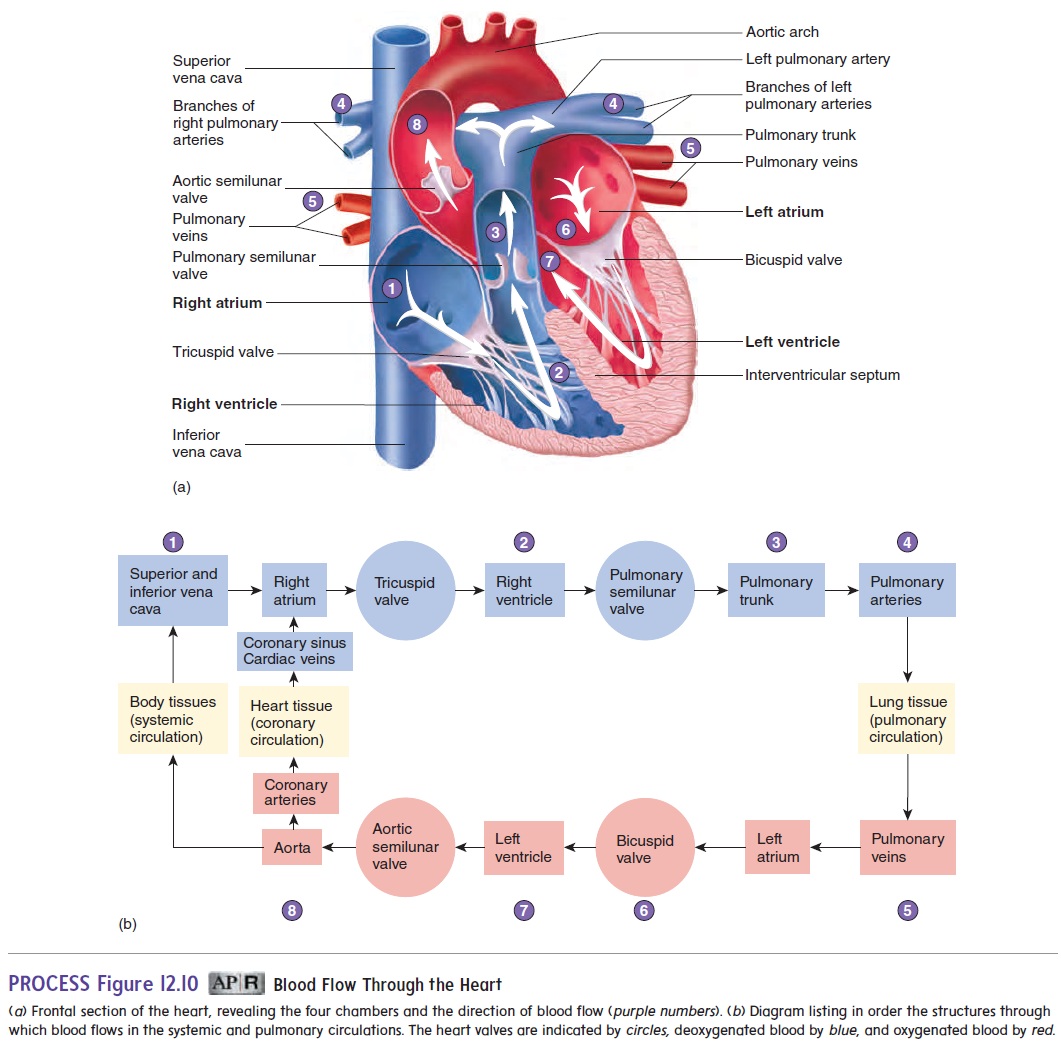
Blood enters the right atrium from the systemic circulation through the superior and inferior venae cavae, and from heart muscle through the coronary sinus. Most of the blood flowing into the right atrium flows into the right ventricle while the right ven-tricle relaxes following the previous contraction. Before the end of ventricular relaxation, the right atrium contracts, and enough blood is pushed from the right atrium into the right ventricle to complete right ventricular filling.
Following right atrial contraction, the right ventricle begins to contract. This contraction pushes blood against the tricuspid valve, forcing it closed. After pressure within the right ventricle increas-es, the pulmonary semilunar valve is forced open, and blood flows into the pulmonary trunk. As the right ventricle relaxes, its pressure falls rapidly, and pressure in the pulmonary trunk becomes greater than in the right ventricle. The backflow of blood forces the pul-monary semilunar valve to close.
The pulmonary trunk branches to form the right and left pulmonary arteries, which carry blood to the lungs, where CO2 is released and O2 is picked up. Blood returning from the lungs enters the left atrium through the four pulmonary veins (figure 12.10).
Most of the blood flowing into the left atrium passes into the left ventricle while the left ventricle relaxes following the previous contraction. Before the end of ventricular relaxation, the left atrium contracts, and enough blood is pushed from the left atrium into the left ventricle to complete left ventricular filling.
Following left atrial contraction, the left ventricle begins to contract. This contraction pushes blood against the bicuspid valve, forcing it closed. After pressure within the left ventricle increases, the aortic semilunar valve is forced open, and blood flows into the aorta. Blood flowing through the aorta is distributed to all parts of thebody, except to those parts of the lungs supplied by the pulmonary blood vessels. As the left ventricle relaxes, its pressure falls rapidly, and pressure in the aorta becomes greater than in the left ventricle. The backflow of blood forces the aortic semilunar valve to close.
Blood Supply to the Heart
Coronary Arteries
The cardiac muscle in the wall of the heart is thick and metabolically very active. Two coronary arteries supply blood to the wall of the heart (figure 12.11a). The coronary arteries originate from the base of the aorta, just above the aortic semilunar valves. The left coro-nary artery originates on the left side of the aorta. It has three majorbranches: The anterior interventricular artery lies in the anterior interventricular sulcus; the circumflex artery extends around the coronary sulcus on the left to the posterior surface of the heart; and the left marginal artery extends inferiorly along the lateral wall of the left ventricle from the circumflex artery. The branches of the left coronary artery supply much of the anterior wall of the heart and most of the left ventricle. The right coronary artery originates on the right side of the aorta. It extends around the coronary sulcus on the right to the posterior surface of the heart and gives rise to the posterior interventricular artery, which lies in the posterior inter-ventricular sulcus. The right marginal artery extends inferiorly along the lateral wall of the right ventricle. The right coronary artery and its branches supply most of the wall of the right ventricle.
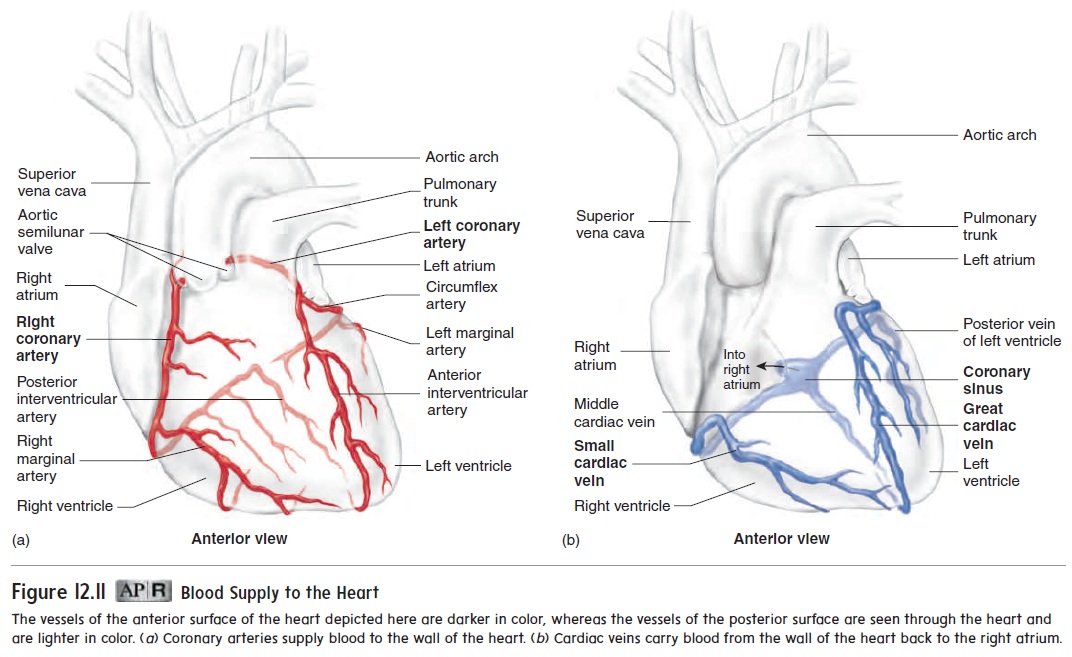
In a resting person, blood flowing through the coronary arter-ies gives up approximately 70% of its O2. In comparison, blood flowing through arteries to skeletal muscle gives up only about 25% of its O2. The percentage of O2 the blood releases to skeletal muscle increases to 70% or more during exercise, but the percent-age of O2 the blood releases to cardiac muscle cannot increase substantially during exercise. Therefore, the rate of blood flow through the coronary arteries must increase above its resting level to provide cardiac muscle with adequate O2 during exercise. Blood flow into the coronary circulation is greatest while the ventricles of the heart are relaxed and contraction of the cardiac muscle does not compress the coronary arteries. Blood flow into other arteries of the body is highest during contraction of the ventricles.
Cardiac Veins
The cardiac veins drain blood from the cardiac muscle. Their path-ways are nearly parallel to the coronary arteries, and most of them drain blood into the coronary sinus, a large vein located within the coronary sulcus on the posterior aspect of the heart. Blood flows from the coronary sinus into the right atrium (figure 12.11b). Some small cardiac veins drain directly into the right atrium.
Related Topics