Chapter: Medical Physiology: Reproductive and Hormonal Functions of the Male (and Function of the Pineal Gland)
Abnormalities of Male Sexual Function
Abnormalities of Male Sexual Function
Prostate Gland and Its Abnormalities
The prostate gland remains relatively small throughout childhood and begins to grow at puberty under the stimulus of testosterone. This gland reaches an almost stationary size by the age of 20 years and remains at this size up to the age of about 50 years. At that time, in some men it begins to involute, along with decreased production of testosterone by the testes.
A benign prostatic fibroadenoma frequently develops in the prostate in many older men and can cause urinary obstruction. This hypertrophy is caused not by testos-terone but instead by abnormal overgrowth of prostate tissue itself.
Cancer of the prostate gland is a different problem and is a common cause of death, accounting for about 2 to 3 per cent of all male deaths. Once cancer of the prostate gland does occur, the cancerous cells are usually stimulated to more rapid growth by testosterone and are inhibited by removal of both testes so that testosterone cannot be formed. Prostatic cancer usually can be inhibited by administration of estrogens. Even some patients who have prostatic cancer that has already metastasized to almost all the bones of the body can be successfully treated for a few months to years by removal of the testes, by estrogen therapy, or by both; after this therapy the metastases usually diminish in size and the bones partially heal. This treatment does not stop the cancer but does slow it and sometimes greatly diminishes the severe bone pain.
Hypogonadism in the Male
When the testes of a male fetus are nonfunctional during fetal life, none of the male sexual characteristics develop in the fetus. Instead, female organs are formed. The reason for this is that the basic genetic characteris-tic of the fetus, whether male or female, is to form female sexual organs if there are no sex hormones. But in the presence of testosterone, formation of female sexual organs is suppressed, and instead, male organs are induced.
When a boy loses his testes before puberty, a state of eunuchism ensues in which he continues to have infan-tile sex organs and other infantile sexual characteristics throughout life. The height of an adult eunuch is slightly greater than that of a normal man because the bone epiphyses are slow to unite, although the bones are quite thin and the muscles are considerably weaker than those of a normal man. The voice is childlike, there is no loss of hair on the head, and the normal adult masculine hair distribution on the face and elsewhere does not occur.
When a man is castrated after puberty, some of his male secondary sexual characteristics revert to those of a child and others remain of adult masculine character. The sexual organs regress slightly in size but not to a childlike state, and the voice regresses from the bass quality only slightly. Conversely, there is loss of mascu-line hair production, loss of the thick masculine bones, and loss of the musculature of the virile male.
Also in a castrated adult male, sexual desires are decreased but not lost, provided sexual activities have been practiced previously. Erection can still occur as before, although with less ease, but it is rare that ejacu-lation can take place, primarily because the semen-forming organs degenerate and there has been a loss of the testosterone-driven psychic desire.
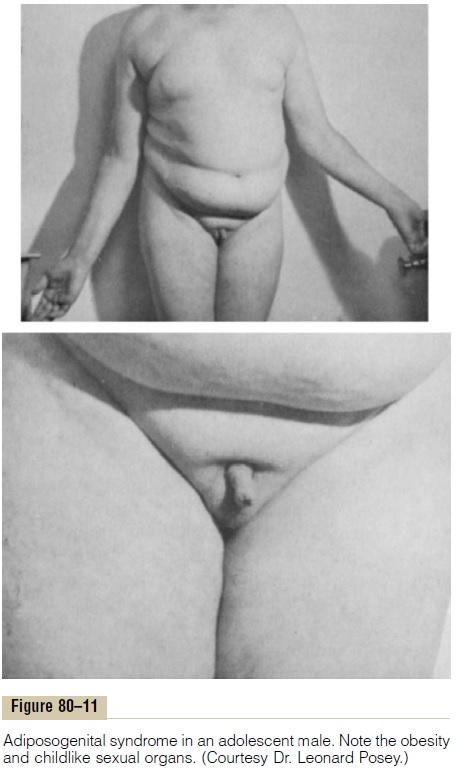
Some instances of hypogonadism are caused by a genetic inability of the hypothalamus to secrete normal amounts of GnRH. This often is associated with a simultaneous abnormality of the feeding center of the hypothalamus, causing the person to greatly overeat. Consequently, obesity occurs along with eunuchism. A patient with this condition is shown in Figure 80–11; the condition is called adiposogenital syndrome, Fröhlich’ssyndrome, orhypothalamic eunuchism.
Testicular Tumors and Hypergonadism in the Male
Interstitial Leydig cell tumors develop in rare instancesin the testes, but when they do develop, they sometimes produce as much as 100 times the normal quantities of testosterone. When such tumors develop in young chil-dren, they cause rapid growth of the musculature and bones but also cause early uniting of the epiphyses, so that the eventual adult height actually is considerably less than that which would have been achieved other-wise. Such interstitial cell tumors also cause excessive development of the male sexual organs, all skeletal muscles, and other male sexual characteristics. In the adult male, small interstitial cell tumors are difficult to diagnose because masculine features are already present.
Much more common than the interstitial Leydig cell tumors are tumors of the germinal epithelium. Because germinal cells are capable of differentiating into almost any type of cell, many of these tumors contain multiple tissues, such as placental tissue, hair, teeth, bone, skin, and so forth, all found together in the same tumorous mass called a teratoma. These tumors often secrete few hormones, but if a significant quantity of placental tissue develops in the tumor, it may secrete large quantities of hCG with functions similar to those of LH. Also, estrogenic hormones are sometimes secreted by these tumors and cause the condition called gynecomastia (overgrowth of the breasts).
Related Topics