Chapter: Clinical Cases in Anesthesia : Ambulatory Surgery
What are the etiologies of nausea and vomiting, and what measures can be taken to decrease their incidence and severity?
What are the etiologies of
nausea and vomiting, and what measures can be taken to decrease their incidence
and severity?
Unfortunately, postoperative nausea and
vomiting remain a significant problem in patients who receive either general
anesthesia or intravenous sedation. They are among the most commonly reported
complications associated with ambulatory surgery, and hospitalization following
an ambulatory procedure is often attributable to them. Persistent and severe
retching or vomiting can disrupt sur-gical repairs and cause increased
bleeding; left untreated, they may lead to dehydration and electrolyte
imbalance. From 10% to 40% of patients who have not received anti-emetic prophylaxis
may be expected to experience some degree of nausea or frank vomiting. The
incidence of nausea and vomiting depends on the type of surgical proce-dure
performed, as well as the anesthetic administered. It has been demonstrated
that patients undergoing laparoscopy have a 35% incidence of nausea and
vomiting. This may be due to manipulation of abdominal viscera, retained
intraperitoneal carbon dioxide, and the use of electrocautery. Symptoms occur
regardless of whether a general anesthetic or epidural technique is employed.
Arthroscopic surgical procedures are associated with a much lower incidence of
symptoms than laparoscopic surgeries or ovum retrievals.
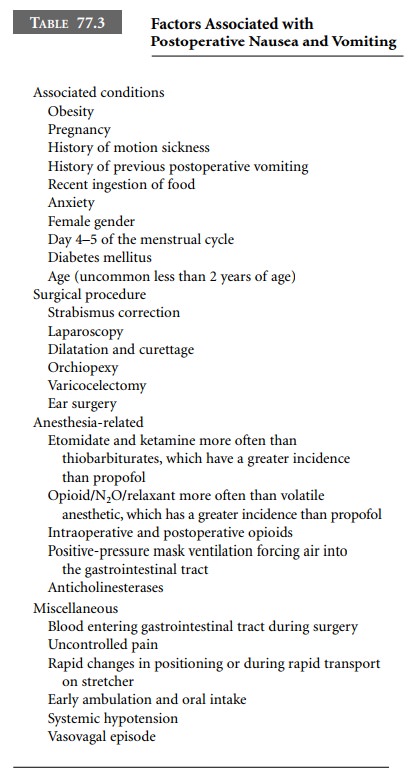
The cause of postoperative nausea and vomiting
is multifactorial (Table 77.3). Obesity, sudden movement or changes in patient
position, a history of motion sickness, postoperative hypotension, female
gender, days 4 and 5 of the menstrual cycle, pain, opioid administration, the
anes-thetic technique used, and site of surgery may all contribute to the
establishment and persistence of these symptoms. They are often disquieting and
sometimes incapacitating. Physical measures as well as pharmacologic agents
have been employed in an attempt to reduce the incidence of these distressing
sequelae. Examples include the attempted removal of stomach contents by
intraoperative gastric suc-tioning; avoidance of excessive positive pressure
during mask ventilation, which may force gas into the stomach; and diminished
use of opioid-based general anesthesia. These have proven to have variable
effects in the reduction of nausea and vomiting, probably because the problem
is strongly multifactorial in nature.
Nitrous oxide has been both implicated and
exonerated in multiple studies. It is unlikely that this gas plays a major role
in influencing the presence or absence of nausea in the postoperative period.
However, the selection of induction agent does influence the incidence of
postoperative symp-tomatology. Etomidate and ketamine are associated with a
much higher incidence of these symptoms when compared with thiopental. General
anesthesia induced and main-tained with propofol is associated with the least
number of episodes of nausea and emesis.
To help prevent symptoms, moving patients
slowly from the operating room table to the stretcher, avoiding sudden turns
during transport to the PACU, and allowing patients to wake up slowly have been
applied with some measure of success. Warm blankets and repeated verbal
reassurance may reduce overall anxiety by increasing feelings of well-being and
a sense of security. A vigorous stir-up, sit-them-up reg-imen with early oral
intake is likely to precipitate nausea and vomiting. The end result of
significant symptomatology is an increased length of stay in the PACU. For the
patient with unremitting symptoms, overnight admission for observation and
further treatment with anti-emetics and intravenous fluids to prevent
dehydration may be required.
Adequate hydration must be ensured during the
opera-tive period as well as maintained in the PACU. To avoid pre-cipitating
episodes of nausea or vomiting postoperatively, it is recommended to hydrate
vigorously intraoperatively with at least 15–20 mL/kg of crystalloid solutions
and to avoid pushing oral fluids and food. Intravenous fluid repletion allows
oral fluids to be offered sparingly. Solids should be withheld until the
patient expresses hunger. In addition, postponing early ambulation may help to
reduce symptoms.
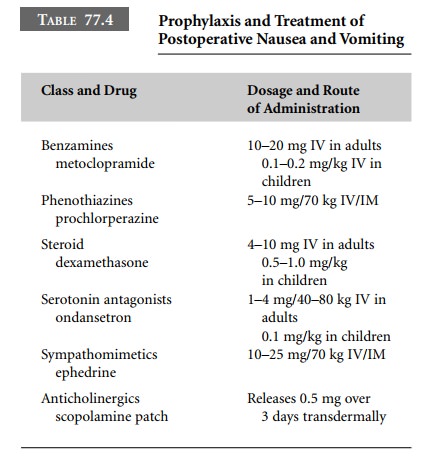
Prophylactic administration of dexamethasone
(4–10 mg IV) at the beginning of the procedure, and metoclopramide (10 mg IV)
have been advocated. Droperidol, a potent anti-emetic, has fallen into disfavor
because of its association with QT prolongation and torsades de pointes. This
led the FDA to issue a black-box warning regarding its use. The FDA’s
rec-ommendations have been challenged because of droperi-dol’s long history of
efficacy and rare occurrence of adverse events. If one decides to administer
droperidol, a baseline ECG should be performed, and the QT interval should be
measured. Furthermore, the ECG should be monitored during its administration
(Table 77.4).
Unfortunately, clinically significant
side-effects have been reported with these agents. These include prolonged
sedation and delayed awakening, an increase in anxiety as well as restlessness,
and extrapyramidal symptoms. Acute dystonic reactions including torticollis,
tics, or an oculogyric crisis can be treated with diphenhydramine, 25–50 mg, or
with benztropine, 1–2 mg, intravenously or intramuscularly.
Transdermal scopolamine, proven earlier to be
effica-cious in the prevention of motion sickness, has been studied for the
prevention of postoperative nausea and vomiting. Although effective in reducing
symptoms when applied 12 hours before surgery, significant side-effects
including dry mouth as well as sedation, dysphoria, and urinary retention may
occur. It is often reserved for preoperative use in patients who have a strong
history of motion sickness. In the pediatric age group, the incidence of visual
distur-bances and hallucinations after application of the patch is increased.
Some clinicians have placed the patch before discharge in patients whose nausea
has not completely resolved. However, the patch should be avoided in the geriatric
population, pregnant or lactating patients, and in patients with glaucoma.
Ephedrine has been used in the treatment of
nausea and vomiting in the PACU. Hypotension or documented postural hypotension
in the postoperative period is often due to an intravascular volume deficit and
should be ruled out. Treatment consists of crystalloid infusion to correct
hemo-dynamic instability. Ephedrine has been demonstrated to be useful in
patients whose symptoms are causally related to assuming the upright position.
Ephedrine, 0.5 mg/kg given intramuscularly, has been used in laparoscopy
patients with some success. Patients who received ephedrine also had lower
sedation scores, and no differences in mean arterial blood pressure were noted.
It may be indicated in other-wise healthy patients who have a history of motion
sickness or in those patients who experience dizziness, nausea, or vomiting
when attempting to ambulate in the postopera-tive period.
A popular drug in the anesthesiologist’s
armamen-tarium against nausea and vomiting, ondansetron, is a serotonin
receptor antagonist with possible central and peripheral sites of action. It
does not appear to affect awakening from general anesthesia and has no
extra-pyramidal effects or sedative qualities. Ondansetron appears to offer
improved control over both nausea and vomiting. The effective dose is 2–4 mg
intravenously and has a duration of action of up to 24 hours. An oral
for-mulation is also available. It has been demonstrated that a combination of
agents, perhaps in conjunction with propofol, will prove to be most efficacious
in the prophyl-axis of nausea and vomiting.
Many surgical centers have abandoned the
routine administration of prophylactic anti-emetics to every patient. However,
anti-emetic regimens should be admin-istered for specific surgical procedures,
such as strabismus repair or laparoscopic surgery, that are associated with an
extraordinarily high incidence of postoperative nausea and vomiting.
Sometimes simply relieving postoperative pain
may alleviate nausea. The use of acupuncture has been reported in some studies
to be effective, but its use is not wide-spread. A propofol-based anesthetic is
associated with fewer emetic symptoms, earlier ability to tolerate oral
ali-mentation, and shorter stays in the PACU when compared with induction with
a thiobarbiturate and maintenance with isoflurane. Unfortunately, despite
careful anes-thetic management including propofol and even prophyl-actic
medication, symptoms of nausea and vomiting in the postoperative period still
remain a problem.
Related Topics