Chapter: Medical Physiology: Reproductive and Hormonal Functions of the Male (and Function of the Pineal Gland)
Spermatogenesis
Spermatogenesis
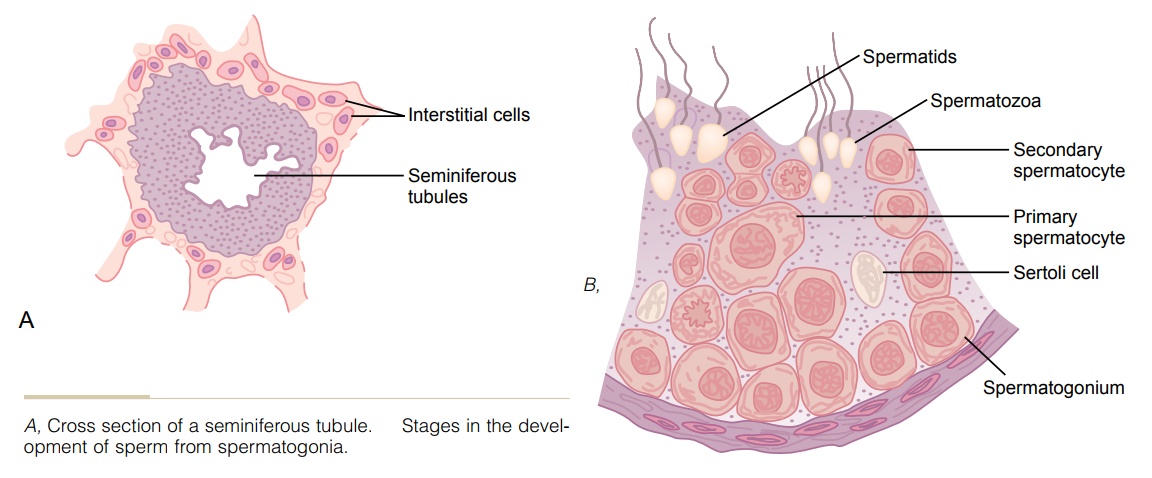
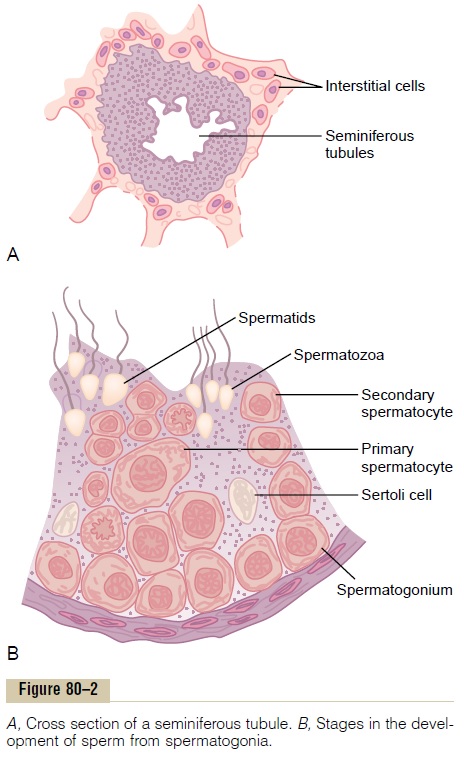
During formation of the embryo, the primordial germ cells migrate into the testes and become immature germ cells called spermatogonia which lie in two or three layers of the inner surfaces of the seminiferous tubules (a cross section of one is shown in Figure 80–2A). The spermatogonia begin to undergo mitotic division, beginning at puberty, and continually proliferate and differentiate through definite stages of development to form sperm, as shown in Figure 80–2B.
Steps of Spermatogenesis
Spermatogenesis occurs in the seminiferous tubules during active sexual life as the result of stimulation by anterior pituitary gonadotropic hormones, begin-ning at an average age of 13 years and continuing throughout most of the remainder of life but decreasing markedly in old age.
In the first stage of spermatogenesis, the spermatogonia migrate among Sertoli cells toward the central lumen of the seminiferous tubule. The Sertoli cells are very large, with overflowing cytoplasmic envelopes that surround the developing spermatogo-nia all the way to the central lumen of the tubule.
Meiosis. Spermatogonia that cross the barrier into theSertoli cell layer become progressively modified and enlarged to form large primary spermatocytes (Figure 80–3). Each of these, in turn, undergoes meiotic division to form two secondary spermatocytes. After another few days, these too divide to form spermatids that are eventually modified to become spermatozoa (sperm).
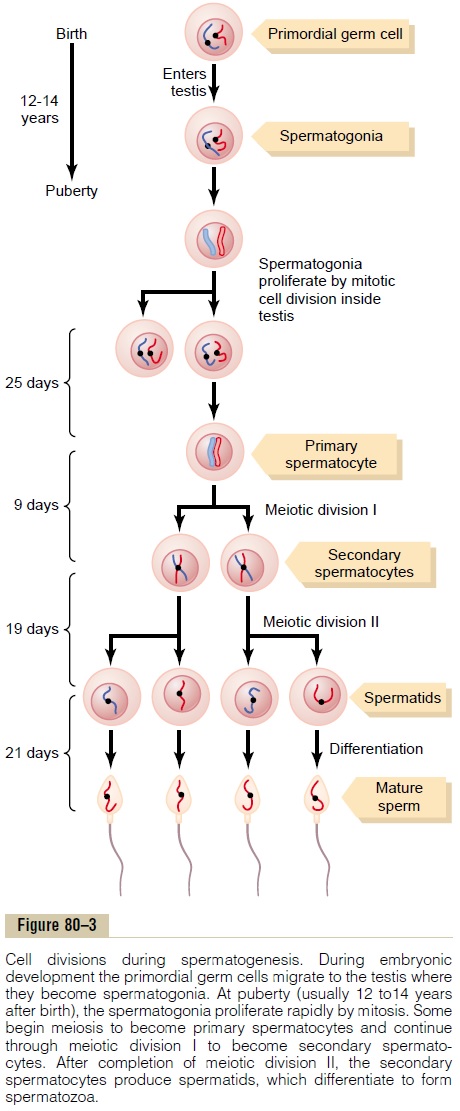
During the change from the spermatocyte stage to the spermatid stage, the 46 chromosomes (23 pairs of chromosomes) of the spermatocyte are divided, so that 23 chromosomes go to one spermatid and the other 23 to the second spermatid. This also divides the chro-mosomal genes so that only one half of the genetic characteristics of the eventual fetus are provided by the father, while the other half are derived from the oocyte provided by the mother.
The entire period of spermatogenesis, from sper-matogonia to spermatozoa, takes about 74 days.
Sex Chromosomes. In each spermatogonium, one of the23 pairs of chromosomes carries the genetic informa-tion that determines the sex of each eventual offspring. This pair is composed of one X chromosome, which is called the female chromosome, and one Y chromo-some, the male chromosome. During meiotic division, the male Y chromosome goes to one spermatid that then becomes a male sperm, and the female X chro-mosome goes to another spermatid that becomes a female sperm. The sex of the eventual offspring isdetermined by which of these two types of sperm fertilizes the ovum.
Formation of Sperm. When the spermatids are firstformed, they still have the usual characteristics of epithelioid cells, but soon they begin to differentiate and elongate into spermatozoa. As shown in Figure 80–4, each spermatozoon is composed of a head and a
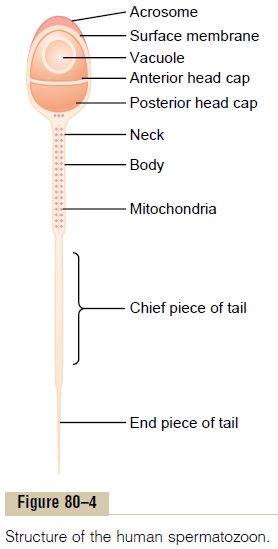
tail. The head comprises the condensed nucleus of thecell with only a thin cytoplasmic and cell membrane layer around its surface. On the outside of the anterior two thirds of the head is a thick cap called the acro-some that is formed mainly from the Golgi apparatus. This contains a number of enzymes similar to those found in lysosomes of the typical cell, including hyaluronidase (which can digest proteoglycan fila-ments of tissues) and powerful proteolytic enzymes (which can digest proteins). These enzymes play important roles in allowing the sperm to enter the ovum and fertilize it.
The tail of the sperm, called the flagellum, has three major components: (1) a central skeleton constructed of 11 microtubules, collectively called theaxoneme— the structure of this is similar to that of cilia found on the surfaces of other types of cells; (2) a thin cell membrane covering the axoneme; and (3) a collection of mitochondria sur-rounding the axoneme in the proximal portion of the tail (called the body of the tail).
Back-and-forth movement of the tail (flagellar movement) provides motility for the sperm. This movement results from a rhythmical longitudinal sliding motion between the anterior and posterior tubules that make up the axoneme. The energy for this process is supplied in the form of adenosine triphos-phate that is synthesized by the mitochondria in the body of the tail.
Normal sperm move in a fluid medium at a velocity of 1 to 4 mm/min. This allows them to move through the female genital tract in quest of the ovum.
Hormonal Factors That Stimulate Spermatogenesis
We shall discuss the role of hormones in reproduction later, but at this point, let us note that several hor-mones play essential roles in spermatogenesis. Some of these are as follows:
1. Testosterone, secreted by the Leydig cells locatedin the interstitium of the testis, is essential for growth and division of the testicular germinal cells, which is the first stage in forming sperm.
2. Luteinizing hormone, secreted by the anteriorpituitary gland, stimulates the Leydig cells to secrete testosterone.
3. Follicle-stimulating hormone, also secreted by theanterior pituitary gland, stimulates the Sertolicells; without this stimulation, the conversion of the spermatids to sperm (the process of spermiogenesis) will not occur.
4. Estrogens, formed from testosterone by theSertoli cells when they are stimulated by follicle-stimulating hormone, are probably also essential for spermiogenesis.
5. Growth hormone (as well as most of the otherbody hormones) is necessary for controlling background metabolic functions of the testes. Growth hormone specifically promotes early division of the spermatogonia themselves; in its absence, as in pituitary dwarfs, spermatogenesis is severely deficient or absent, thus causing infertility.
Maturation of Sperm in the Epididymis
After formation in the seminiferous tubules, the sperm require several days to pass through the 6-meter-long tubule of the epididymis. Sperm removed from the seminiferous tubules and from the early portions of the epididymis are nonmotile, and they cannot fertil-ize an ovum. However, after the sperm have been in the epididymis for some 18 to 24 hours, they deve-lop the capability of motility, even though several inhibitory proteins in the epididymal fluid still prevent final motility until after ejaculation.
Storage of Sperm. The two testes of the human adultform up to 120 million sperm each day. A small quan-tity of these can be stored in the epididymis, but most are stored in the vas deferens. They can remain stored, maintaining their fertility, for at least a month. During this time, they are kept in a deeply suppressed inactive state by multiple inhibitory substances in the secre-tions of the ducts. Conversely, with a high level of sexual activity and ejaculations, storage may be no longer than a few days.
After ejaculation, the sperm become motile, and they also become capable of fertilizing the ovum, a process called maturation. The Sertoli cells and the epithelium of the epididymis secrete a special nutrient fluid that is ejaculated along with the sperm. This fluid contains hormones (including both testosterone and estrogens), enzymes, and special nutrients that are essential for sperm maturation.
Physiology of the Mature Sperm. The normal motile, fertilesperm are capable of flagellated movement though the fluid medium at velocities of 1 to 4 mm/min. The activity of sperm is greatly enhanced in a neutral and slightly alkaline medium, as exists in the ejacu-lated semen, but it is greatly depressed in a mildly acidic medium. A strong acidic medium can cause rapid death of sperm.
The activity of sperm increases markedly with in-creasing temperature, but so does the rate of metabo-lism, causing the life of the sperm to be considerably shortened. Although sperm can live for many weeks in the suppressed state in the genital ducts of the testes, life expectancy of ejaculated sperm in the female genital tract is only 1 to 2 days.
Function of the Seminal Vesicles
Each seminal vesicle is a tortuous, loculated tube lined with a secretory epithelium that secretes a mucoid material containing an abundance of fructose, citric acid, and other nutrient substances, as well
as large quantities of prostaglandins and fibrinogen. During the process of emission and ejaculation, each seminal vesicle empties its contents into the ejacula-tory duct shortly after the vas deferens empties the sperm. This adds greatly to the bulk of the ejaculated semen, and the fructose and other substances in the seminal fluid are of considerable nutrient value for the ejaculated sperm until one of the sperm fertilizes the ovum.
Prostaglandins are believed to aid fertilization in two ways: (1) by reacting with the female cervical mucus to make it more receptive to sperm movement and (2) by possibly causing backward, reverse peri-staltic contractions in the uterus and fallopian tubes to move the ejaculated sperm toward the ovaries (a few sperm reach the upper ends of the fallopian tubes within 5 minutes).
Function of the Prostate Gland
The prostate gland secretes a thin, milky fluid that con-tains calcium, citrate ion, phosphate ion, a clotting enzyme, and a profibrinolysin. During emission, the capsule of the prostate gland contracts simultaneously with the contractions of the vas deferens so that the thin, milky fluid of the prostate gland adds further to the bulk of the semen. A slightly alkaline characteris-tic of the prostatic fluid may be quite important for successful fertilization of the ovum, because the fluid of the vas deferens is relatively acidic owing to the presence of citric acid and metabolic end products of the sperm and, consequently, helps to inhibit sperm fertility. Also, the vaginal secretions of the female are acidic (pH of 3.5 to 4.0). Sperm do not become opti-mally motile until the pH of the surrounding fluids rises to about 6.0 to 6.5. Consequently, it is probable that the slightly alkaline prostatic fluid helps to neu-tralize the acidity of the other seminal fluids during ejaculation, and thus enhances the motility and fertil-ity of the sperm.
Semen
Semen, which is ejaculated during the male sexual act, is composed of the fluid and sperm from the vas deferens (about 10 per cent of the total), fluid from the seminal vesicles (almost 60 per cent), fluid from the prostate gland (about 30 per cent), and small amounts from the mucous glands, especially the bulbourethral glands. Thus, the bulk of the semen is seminal vesicle fluid, which is the last to be ejaculated and serves to wash the sperm through the ejaculatory duct and urethra.
The average pH of the combined semen is about 7.5, the alkaline prostatic fluid having more than neutral-ized the mild acidity of the other portions of the semen. The prostatic fluid gives the semen a milky appearance, and fluid from the seminal vesicles and mucous glands gives the semen a mucoid consistency. Also, a clotting enzyme from the prostatic fluid causes the fibrinogen of the seminal vesicle fluid to form a weak fibrin coagulum that holds the semen in the deeper regions of the vagina where the uterine cervix lies. The coagulum then dissolves during the next 15 to 30 minutes because of lysis by fibrinolysin formed from the prostatic profibrinolysin. In the early minutes after ejaculation, the sperm remain relatively immo-bile, possibly because of the viscosity of the coagulum. As the coagulum dissolves, the sperm simultaneously become highly motile.
Although sperm can live for many weeks in the male genital ducts, once they are ejaculated in the semen, their maximal life span is only 24 to 48 hours at body temperature. At lowered temperatures, however, semen can be stored for several weeks, and when frozen at temperatures below -100°C, sperm have been preserved for years.
Related Topics