Chapter: Essentials of Psychiatry: Somatoform Disorders
Somatization Disorder
Somatization Disorder
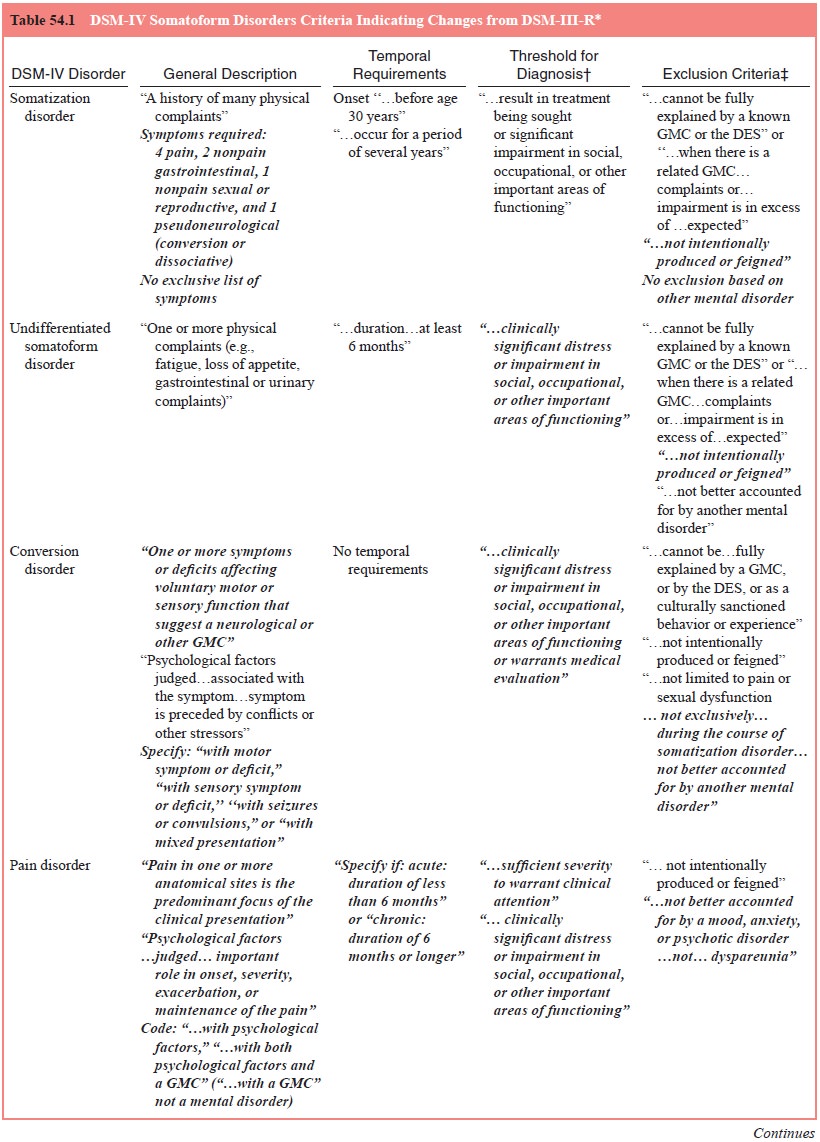
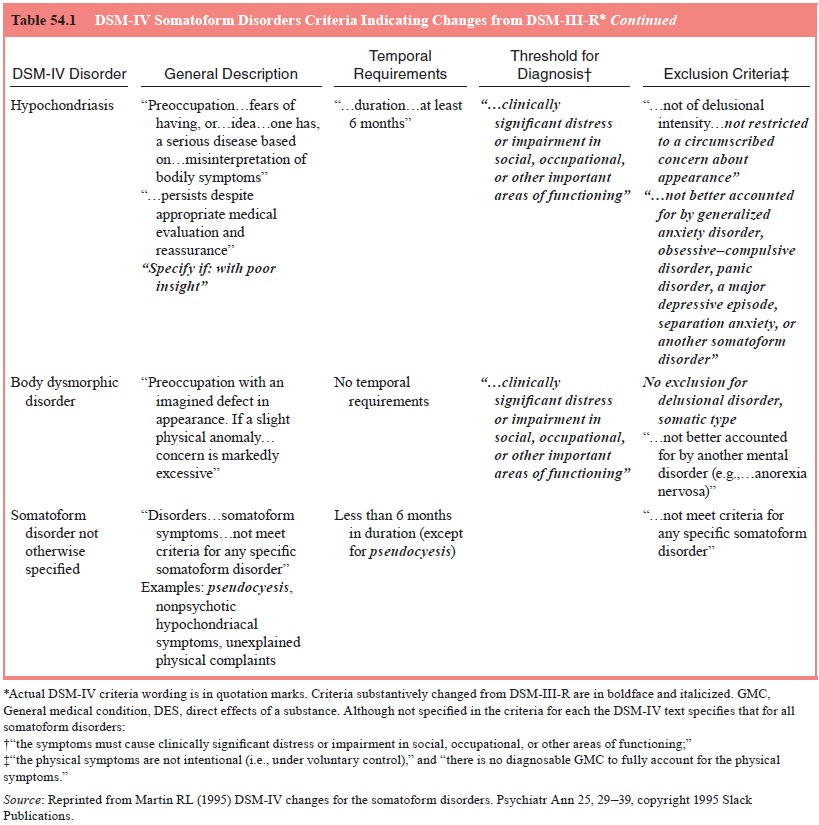
Definition
As defined in DSM-IV, somatization disorder is a polysymp-tomatic
somatoform disorder characterized by multiple recur-ring pains and
gastrointestinal, sexual and pseudoneurological symptoms occurring for a period
of years with onset before age 30 years. The physical complaints are not
intentionally produced and are not fully explained by a general medical
condition or the direct effects of a substance. To warrant diagnosis, they must
result in medical attention or significant impairment in social, occupational,
or other important areas of functioning. Table 54.1 summarizes the criteria for
this disorder.
Despite efforts to simplify it, the somatization disorder construct has
remained somewhat cumbersome.
It remains to be seen whether the DSM-IV diagnosis of somatization
disorder will be used broadly and appropriately. Unresolved problems include
that the term somatization dis-order has acquired a pejorative connotation; a
tendency to di-agnose more readily treatable symptoms such as anxiety and
depressive syndromes without considering the underlying ill-ness; and that
authorization and reimbursement for treatment of this chronic condition are
often challenged or denied. It is rela-tively easier to obtain approval for an
intervention on the basis of major depressive disorder, for example, than on
the basis of a disorder that is much more likely to be poorly understood by
case reviewers.
Epidemiology
In the USA, somatization disorder is found predominantly in women, with
a female/male ratio of approximately 10 : 1 (see Table 54.1). This ratio is not
as large in some other cultures (e.g., in Greeks and Puerto Ricans). Thus,
gender- and culture-specific rates are more meaningful than generalized
figures. The lifetime prevalence of somatization disorder in US women has been
es-timated to be between 0.2 and 2%. The magnitude of this dis-crepancy is
attributable, at least in part, to methodological differ-ences. The
Epidemiological Catchment Area study (Robins et al., 1984), the most recent large-scale general population study
in theUSA to include an assessment for somatization disorder, found a lifetime
risk of somatization disorder of only 0.2 to 0.3% in US women. However, this
study may have underestimated the preva-lence of somatization disorder because
nonphysician interview-ers were used. It is argued that it is difficult for lay
interviewers critically to assess whether somatic symptoms are fully explained
by physical conditions. As a result, they may more readily accept patients’
general medical explanations of symptoms, resulting in fewer diagnoses of
somatization disorder. With age and method of assessment taken into account,
the lifetime risk for somatiza-tion disorder was estimated to be 2% in US
women.
Etiology and Pathophysiology
Many theories on the cause of somatization disorder have been proposed,
however, the etiology remains unknown. Psychody-namic hypotheses regarding the
physical expression of uncon-scious conflict by conversion or somatization have
been influ-ential. Even Freud assumed a “constitutional diathesis”, as had
Charcot before him. Evidence exists for both biological and psy-chosocial
contributions.
Somatization disorder has been shown to be familial. It is observed that
in 10 to 20% of female relatives of patients affected by somatization disorder
there is a lifetime risk in US women 10 to 20 times greater than that of the
general population. Yet, aggregation in families may be attributable to both
genetic and environmental factors. A cross-fostering study of a Swedish
population demonstrated that genetic background and postnatal influences
contribute to the risk of somatization disorder inde-pendently (Bohman et al., 1984). Of additional interest
are obser-vations that male relatives of patients with somatization disorder
show increased rates of antisocial personality and alcoholism, suggesting an
etiological link.
Certain promising theories have focused on learning princi-ples with
possible organic underpinnings. Some have postulated a social communication
model based on learning theory to explain somatization disorder. This theory
hypothesizes that individuals learn to somatize as a means of expressing their
wants and needs and evoking care, nurturance and support from family and
car-egivers. That different sex ratios may exist in different cultures suggests
that such learning differs from culture to culture.
In the 1970s, impaired information-processing problems involving attention and memory were identified in experimental neuropsychological testing. Such deficits may result in vague, nonspecific and impressionistic description for experience. These may underlie a tendency for excessive somatic complaints and, together with tendencies for impulsiveness and monotony intolerance, may contribute to the often associated multiple per-sonal and social problems. Early studies also reported that the pattern of neuropsychological defects found in subjects with so-matization disorder differed from that in normal control, schizo-phrenic and psychotic depression comparison groups. Subjects with somatization disorder had greater bilateral, symmetrical patterns of frontal lobe dysfunction in comparison with normal control subjects and greater dominant hemisphere impairment than control and depressive subjects. Nondominant hemisphere dysfunction was also identified, with greater impairment in the anterior as opposed to posterior regions. However, subjects with somatization disorder had less nondominant hemisphere disor-ganization than schizophrenic subjects. Of interest, these find-ings were similar to findings in male patients with antisocial personality disorder, giving further support to an etiological link with this disorder
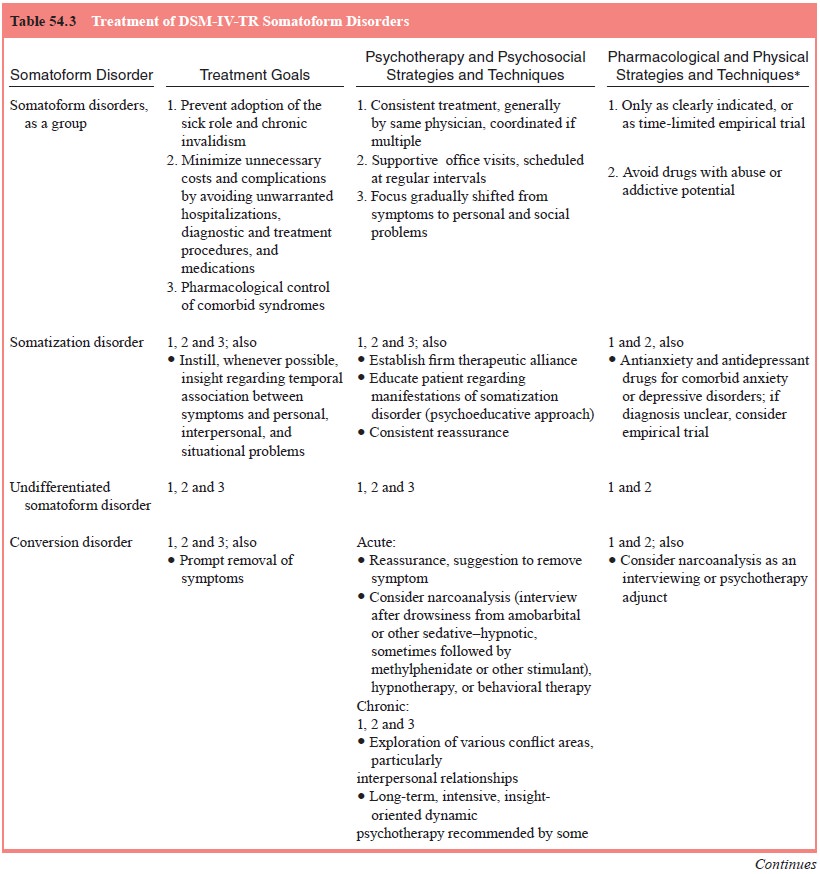
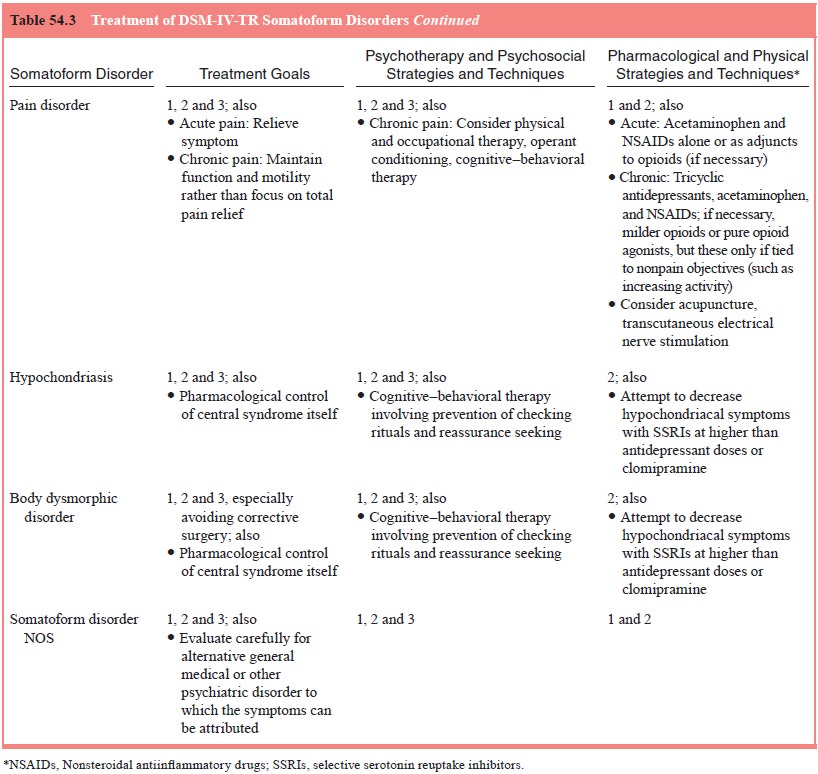
Diagnosis and Differential Diagnosis
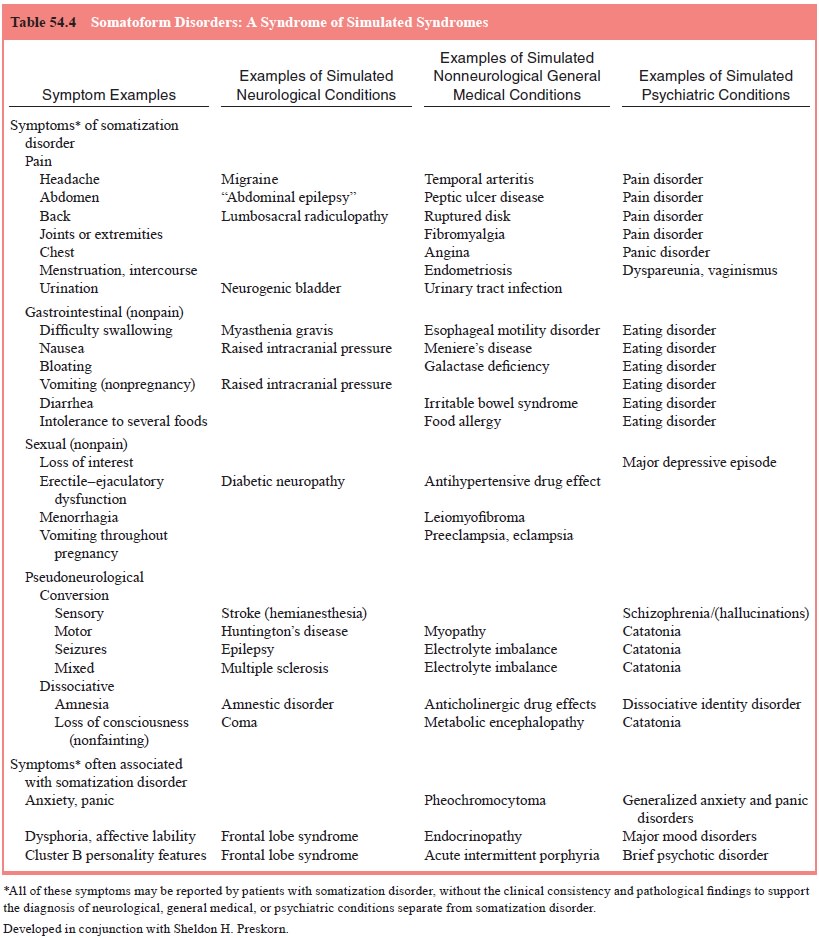
As defined in DSM-IV, somatization disorder is characterized by multiple
recurring physical symptoms and, as will be described, often multiple
psychiatric complaints. Thus, it is not surprising that somatization disorder
may present in a manner suggestive of multiple general medical and, although
too often forgotten, psychiatric disorders (Table 54.3). Indeed, it can be said
that an essential aspect of somatization disorder is its simulation of other
syndromes. As described by Preskorn (1995), “Somatization disorder is
fundamentally a syndrome of apparent syndromes” (see Table 54.4). Thus, the
first task in the diagnosis of somati-zation disorder is the exclusion of other
suggested medical and psychiatric conditions.
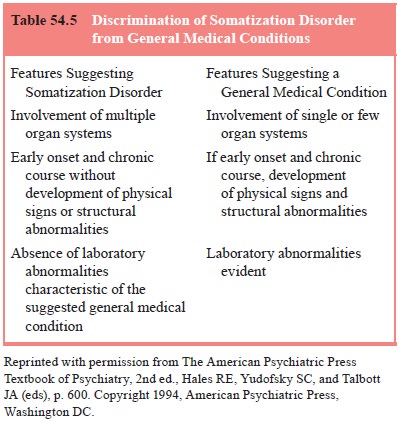
To help in this, Cloninger (1986) identified three features that
generally characterize somatization disorder but rarely gen-eral medical
disorders and these are described in Table 54.5. Another way of characterizing
the distinction is the “reverse fun-nel effect”. With most general medical
conditions, the process of investigation “funnels down” to fewer and fewer
specific diag-nostic possibilities; in somatization disorder, the more
extensive the investigation, the greater the number of suggested disorders.
Several general medical disorders may also fit this pattern and may be confused with somatization disorder. These include multiple sclerosis, other neuropathies, systemic lupus erythema-tosus, acute intermittent porphyria, other hepatic and hemat-opoietic porphyrias, hypercalcemia, certain chronic systemic infections such as brucellosis and trypanosomiasis, myopathies and vasculitides. In general, such conditions begin with dissemi-nated, nonspecific subjective symptoms and transient or equivo-cal physical signs or laboratory abnormalities.
Somatization disorder is characterized by excessive psy-chiatric as well
as physical complaints. Thus, other psychiatric disorders, including anxiety
and mood disorders and schizophre-nia, may be suggested. Although no specific
exclusion criteria regarding other psychiatric disorders are given, one must be
care-ful in accepting “comorbidity” and critically evaluate whether suggested
syndromes are truly additional syndromes or simply manifestations of
somatization disorder.
The overlap between somatization disorder and anxiety disorders may be a
particular problem. Patients with somatiza-tion disorder frequently complain of
many of the same somatic symptoms as patients with anxiety disorders, such as
increased muscle tension, features of autonomic hyperactivity and even discrete
panic attacks. Likewise, anxiety disorder patients may report irrational
disease concerns and such somatic complaints as those involving
gastrointestinal function that are commonly seen in somatization disorder.
However, patients with anxiety disor-ders neither typically report sexual and
menstrual complaints or conversion or dissociative symptoms as in somatization
disorder, nor do they have the associated histrionic presentation and
per-sonal, marital and social maladjustment common in patients with
somatization disorder.
It must be remembered that an anxiety disorder may be co-morbid with
somatization disorder. Here, objective observation of the patient rather than
reliance on the patient’s report may fa-cilitate an additional diagnosis. For
example, patients with soma-tization disorder may report that they are
presently overwhelmed by anxiety while speaking calmly or even cheerfully about
their symptoms, or they may be redirectable while in the midst of a reported
panic attack.
Mood disorders (in particular depression) frequently present with multiple somatic complaints, especially in cer- tain cultures such as in India, where somatic but not mental complaints are acceptable. A longitudinal history identifying age at onset and course of illness may facilitate discrimina-tion of a mood disorder from somatization disorder. In mood disorders, the age at onset of the somatic symptoms is gener-ally later than in somatization disorder; their first appearance generally correlates discretely with the onset of mood symp-toms, and a lengthy pattern of multiple recurring somatic complaints is not seen. Also, resolution of the underlying mood disorder will generally result in disappearance of the somatic complaints.
From the other perspective, patients with somatization disorder often present with depressive complaints. In somatiza-tion disorder, a thorough investigation will reveal a multitude of somatic as well as “depressive” symptoms. Interestingly, soma-tization disorder patients complaining of depression have been found to proffer greater depressive symptoms than individuals with major depression. As in anxiety disorders, major depressive episodes may occur in patients with somatization disorder and must be differentiated from the tendency to have multiple com-plaints, which is characteristic of somatization disorder. As with anxiety disorders, in considering comorbidity with a depressive disorder, the patient’s reports should be corroborated by collat-eral information or by direct observation. Thus, the veracity of the self-report of overwhelming depression and suicidal ideation should be doubted if the patient appears cheerful and charming, at least at times, when interviewed, or if the patient is reported to be actively involved in social activities on an inpatient psychi-atric service.
Schizophrenia may present with generally single but oc-casionally
multiple unexplained somatic complaints. Interview usually uncovers psychotic
symptoms such as delusions, halluci-nations, or disorganized thought. In some
cases, the underlying psychosis cannot be identified initially but, in time,
schizophre-nia will become manifest. Hallucinations are included as exam-ples
of conversion symptoms in DSM-IV. As discussed in the conversion disorder
section, careful analysis of this symptom is warranted so that a misdiagnosis
is not made, relegating a patient to long-term neuroleptic treatment on the
basis of conversion hallucinations.
Patients with histrionic, borderline and antisocial person-ality
disorders frequently have an excess of somatic complaints, at times presenting
with somatization disorder. Antisocial per-sonality disorder and somatization
disorder cluster in individuals and within families and may share common
causes. Dissocia-tive phenomena, in particular dissociative identity disorder,
are commonly associated with somatization disorder. Because dis-sociative
symptoms are included in the diagnostic criteria for so-matization, a separate
diagnosis of a dissociative disorder is not made if such symptoms occur only in
the course of somatization disorder.
Unlike in hypochondriasis and body dysmorphic disor-der, in which
preoccupations and fears concerning the inter-pretation of symptoms
predominate, the focus in somatizationdisorder is on the physical complaints
themselves. Unlike in pain disorder and conversion disorder, multiple
complaints of different types are reported; by definition in DSM-IV, the
his-tory is of pain in at least four sites or functions (e.g., pain with
intercourse, pain in swallowing), at least two nonpain gastroin-testinal
symptoms, at least one nonpain sexual or reproductive symptom, and at least one
conversion or dissociative (i.e., pseu-doneurological) symptom.
Whereas criteria require the onset of symptoms before the age of 30
years, most patients will have had some symptoms at least by adolescence or
early adulthood. Symptoms are often described in a dramatic yet imprecise way
and may be reported inconsistently from interview to interview. The medical
history is usually complicated with multiple medical investigations,
pro-cedures and medication trials. If there have been symptoms for at least 6
months but the onset is later than at age 30 years, or if the required number
and distribution of symptoms are not evi-dent, undifferentiated somatoform
disorder is diagnosed. If the duration has been less than 6 months, somatoform
disorder NOS applies. In general, the greater the number and diversity of
symp-toms, and the longer they have been present without development of signs
of an underlying general medical condition, the greater can be the confidence
that a diagnosis of somatization disorder is correct.
Related Topics