Chapter: Medical Surgical Nursing: Assessment of Respiratory Function
Physical Assessment of Breathing Ability in the Acutely Ill Patient
PHYSICAL ASSESSMENT OF BREATHING ABILITY IN THE ACUTELY III PATIENT
Tests
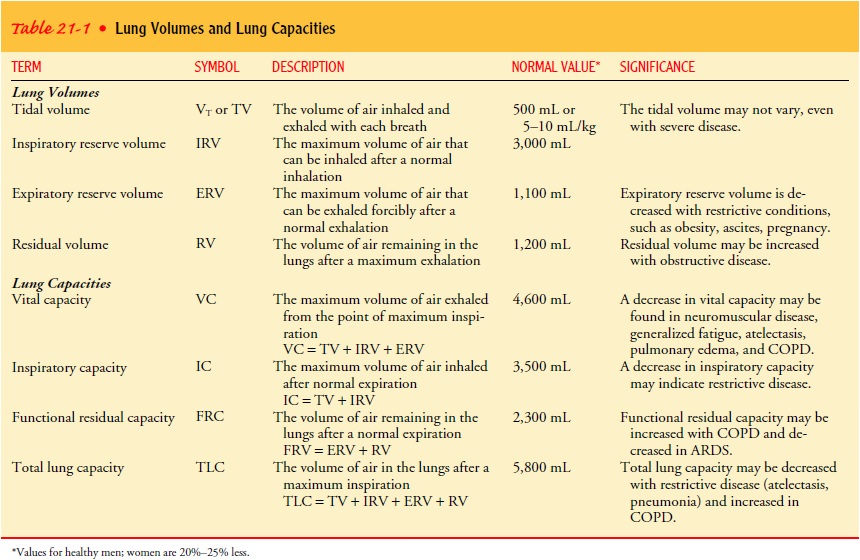
of the patient’s breathing ability are easily performed at the bedside by
measuring the respiratory rate (see the previous section “Breathing Patterns
and Respiratory Rates”), tidal volume, minute ventilation, vital capacity,
inspiratory force, and compliance. These tests are particularly important for
patients at risk for developing pulmonary complications, including those who
have undergone chest or abdominal surgery, have had prolonged anesthesia, have
preexisting pulmonary disease, or are elderly. These tests are also used
routinely for mechanically ventilated patients.
Patients
whose chest expansion is limited by external restric-tions such as obesity or
abdominal distention and who cannot breathe deeply because of postoperative
pain or sedation will inhale and exhale a low volume of air (referred to as low
tidal volumes). Prolonged hypoventilation at low tidal volumes can produce
alve-olar collapse or atelectasis. The amount of air remaining in the lungs
after a normal expiration (functional residual capacity) falls, the ability of
the lungs to expand (compliance) is reduced, and the patient must breathe
faster to maintain the same degree of tis-sue oxygenation. These events can be
exaggerated in patients who have preexisting pulmonary diseases and in elderly
patients whose airways are less compliant, because the small airways may
collapse during expiration.
Tidal Volume
The
volume of each breath is referred to as the tidal volume (see Table 21-1 to
review lung capacities and volumes). A spirometer is an instrument that can be
used at the bedside to measure volumes. If the patient is breathing through an
endotracheal tube or tra-cheostomy, the spirometer is directly attached to it
and the exhaled volume is obtained from the reading on the gauge. In other
pa-tients, the spirometer is attached to a facemask or a mouthpiece po-sitioned
so that it is airtight, and the exhaled volume is measured.
The
tidal volume may vary from breath to breath. To make the measurement reliable,
it is important to measure the volumes of several breaths and to note the range
of tidal volumes, together with the average tidal volume.
Minute Ventilation
Respiratory rates and tidal volume alone are unreliable indicators of adequate ventilation because both can vary widely from breath to breath. Together, however, the tidal volume and respiratory rate are important because the minute ventilation, which is use-ful in detecting respiratory failure, can be determined from them. Minute ventilation is the volume of air expired per minute. It is equal to the product of the tidal volume and the respiratory rate or frequency. In practice, the minute ventilation is not calculated but is measured directly using a spirometer.
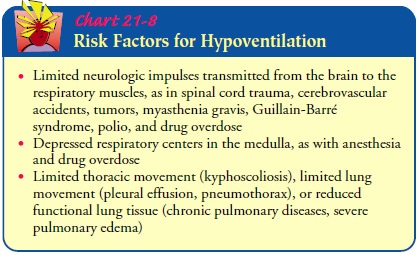
Minute
ventilation may be decreased by a variety of condi-tions that result in
hypoventilation. When the minute ventilation falls, alveolar ventilation in the
lungs also decreases, and the PaCO2
increases. Risk factors for hypoventilation are listed in Chart 21-8.
Vital Capacity
Vital
capacity is measured by having the patient take in a maximal breath and exhale
fully through a spirometer. The normal value depends on the patient’s age,
gender, body build, and weight.
When
the vital capacity is exhaled at a maximal flow rate, the forced vital capacity
is measured. Most patients can exhale at least 80% of their vital capacity in 1
second (forced expiratory volume in 1 second, or FEV1)
and almost all of it in 3 seconds (FEV3
). A reduction in FEV1 suggests
abnormal pulmonary air flow. If the patient’s FEV1
and forced vital capacity are proportionately reduced, maximal lung expansion
is restricted in some way. If the reduction in FEV1
greatly exceeds the reduction in forced vital capacity, the patient may have
some degree of airway obstruction.
Inspiratory Force
Inspiratory
force evaluates the effort the patient is making during inspiration. It does
not require patient cooperation and thus is useful in the unconscious patient.
The equipment needed for this measurement includes a manometer that measures
negative pres-sure and adapters that are connected to an anesthesia mask or a
cuffed endotracheal tube. The manometer is attached and the air-way is
completely occluded for 10 to 20 seconds while the inspi-ratory efforts of the
patient are registered on the manometer. The normal inspiratory pressure is about
100 cm H2O. If the negative pressure
registered after 15 seconds of occluding the airway is less than about 25 cm H2O,
mechanical ventilation is usually re-quired because the patient lacks
sufficient muscle strength for deep breathing or effective coughing.
Related Topics