Chapter: Medical Surgical Nursing: Management of Patients With Oral and Esophageal Disorders
Nursing Process: The Patient With a Condition of the Esophagus
NURSING
PROCESS: THE PATIENT WITH A CONDITION OF THE ESOPHAGUS
Assessment
Emergency
conditions of the esophagus (perforation, chemical burns) usually occur in the
home or away from medical help and require emergency medical care. The patient
is treated for shock and respiratory distress and transported as quickly as
possible to a medical facility. Foreign bodies in the esophagus do not pose an
immediate threat to life unless pressure is exerted on the trachea, resulting
in dyspnea or interfering with respiration, or unless there is leakage of
caustic alkali from a battery. Educating the public to prevent inadvertent
swallowing of foreign bodies or cor-rosive agents is a major health issue.
For
nonemergency symptoms, a complete health history may reveal the nature of the
esophageal disorder. The nurse asks about the patient’s appetite. Has it
remained the same, increased, or de-creased? Is there any discomfort with swallowing?
If so, does it occur only with certain foods? Is it associated with pain? Does
a change in position affect the discomfort? The patient is asked to describe
the pain. Does anything aggravate it? Are there any other symptoms that occur
regularly, such as regurgitation, nocturnal regurgitation, eructation
(belching), heartburn, substernal pres-sure, a sensation that food is sticking
in the throat, a feeling of becoming full after eating a small amount of food,
nausea, vomiting, or weight loss? Are the symptoms aggravated by emotional
upset? If the patient reports any of these symptoms, the nurse asks about the
time of their occurrence, their relationship to eating, and factors that
relieve or aggravate them (eg, position change, belching, antacids, vomiting).
This
history also includes questions about past or present causative factors, such
as infections and chemical, mechanical, or physical irritants; the degree to
which alcohol and tobacco are used; and the amount of daily food intake. The
nurse determines whether the patient appears emaciated and auscultates the
patient’s chest to determine whether pulmonary complications exist.
Nursing Diagnosis
Based
on the assessment data, the nursing diagnoses may include the following:
a) Imbalanced nutrition, less
than body requirements, related to difficulty swallowing
b) Risk for aspiration
related to difficulty swallowing or to tube feeding
c) Acute pain related to
difficulty swallowing, ingestion of an abrasive agent, tumor, or frequent
episodes of gastric reflux
d) Deficient knowledge
about the esophageal disorder, diag-nostic studies, medical management,
surgical intervention, and rehabilitation
Planning and Goals
The
major goals for the patient may include attainment of ade-quate nutritional
intake, avoidance of respiratory compromise from aspiration, relief of pain,
and increased knowledge level.
Nursing Interventions
ENCOURAGING ADEQUATE NUTRITIONAL INTAKE
The
patient is encouraged to eat slowly and to chew all food thor-oughly so that it
can pass easily into the stomach. Small, frequent feedings of nonirritating
foods are recommended to promote di-gestion and to prevent tissue irritation.
Sometimes liquid swal-lowed with food helps the food pass through the
esophagus. Food should be prepared in an appealing manner to help stimulate the
appetite. Irritants such as tobacco and alcohol should be avoided. A baseline
weight is obtained, and daily weights are recorded. The patient’s intake of
nutrients is assessed.
DECREASING RISK OF ASPIRATION
The
patient who has difficulty swallowing or difficulty handling secretions should
be kept in at least a semi-Fowler’s position to decrease the risk of
aspiration. The patient can be instructed in the use of oral suction to
decrease the risk of aspiration further.
RELIEVING PAIN
Small,
frequent feedings are recommended, because large quanti-ties of food overload
the stomach and promote gastric reflux. The patient is advised to avoid any
activities that increase pain, and to remain upright for 1 to 4 hours after
each meal to prevent reflux. The head of the bed should be placed on 4- to
8-inch (10- to 20-cm) blocks. Eating before bedtime is discouraged.
The patient is advised that excessive use of over-the-counter antacids can cause rebound acidity. Antacid use should be directed by the primary care provider, who can recommend the daily, safe dose needed to neutralize gastric juices and prevent esophageal irritation. Histamine2 antagonists are administered as prescribed to decrease gastric acid irritation.
PROVIDING PATIENT EDUCATION
The
patient is prepared physically and psychologically for diag-nostic tests,
treatments, and possible surgical intervention. The principal nursing
interventions include reassuring the patient and discussing the procedures and
their purposes. Some disorders of the esophagus evolve over time, whereas
others are the result of trauma (eg, chemical burns, perforation). In instances
of trauma, the emotional and physical preparation for treatment is more
dif-ficult because of the short time available and the circumstances of the
injury. Treatment interventions must be evaluated continu-ally; the patient is
given sufficient information to participate in care and diagnostic tests. If
endoscopic diagnostic methods are used, the patient is instructed regarding the
moderate sedation that will be used during the procedure. If procedures are
being performed on an outpatient basis with the use of moderate seda-tion, the
patient is instructed to have someone available to drive him or her home after
the procedure. If surgery is required, im-mediate and long-term evaluation is
similar to that for a patient undergoing thoracic surgery.
PROMOTING HOME AND COMMUNITY-BASED CARE
Teaching Patients Self-Care
The
self-care required of the patient depends on the nature of the disorder and on
the surgery or treatment measures used (eg, diet, positioning, medications). If
an ongoing condition exists, the nurse helps the patient plan for needed
physical and psychologi-cal adjustments and for follow-up care (Chart 35-4).
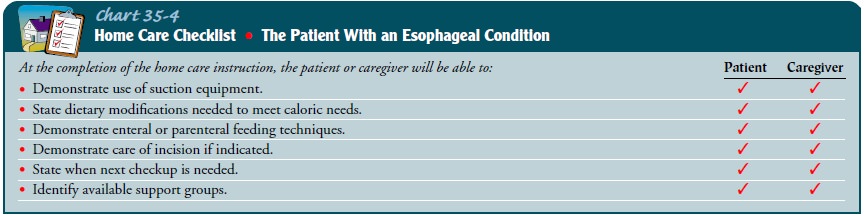
Special
equipment, such as suction or enteral or parenteral feeding devices, may be
required. The patient may need assistance in planning meals, using medications
as prescribed, and resum-ing activities. Education about nutritional
requirements and how to measure the adequacy of nutrition is important. Elderly
and debilitated patients in particular often need assistance and edu-cation in
ways to adjust to their limitations and to resume activ-ities that are
important to them.
Continuing Care
Patients
with chronic esophageal conditions require an individ-ualized approach to their
management at home. Foods may need to be prepared in a special way (blenderized
foods, soft foods), and the patient may need to eat more frequently (eg, four
to six small servings per day). The medication schedule is adjusted to the
patient’s daily activities as much as possible. Anal-gesic medications and
antacids can usually be taken as needed every 3 to 4 hours.Postoperative home
health care focuses on nutritional sup-port, management of pain, and
respiratory function. Some pa-tients are discharged from the hospital with
enteral feeding by means of a gastrostomy or jejunostomy tube or parenteral
nutri-tion. The patient and care provider need specific instructions re-garding
management of the equipment and treatments. Home care visits by a nurse may be
necessary to assess the patient’s care and the care provider’s ability to
provide the necessary care. For some pa-tients, a multidisciplinary team comprising
a dietitian, a social worker, and family members is helpful. Hospice care is
appro-priate for some patients.
Evaluation
EXPECTED PATIENT OUTCOMES
Expected
patient outcomes may include:
1) Achieves an adequate
nutritional intake
a. Eats small, frequent meals
b. Drinks water with small
servings of food
c. Avoids irritants
(alcohol, tobacco, very hot beverages)
d. Maintains desired weight
2) Does not aspirate or
develop pneumonia
a. Maintains upright
position during feeding
b. Uses oral suction
equipment effectively
3) Is free of pain or able
to control pain within a tolerable level
a. Avoids large meals and
irritating foods
b. Takes medications as
prescribed and with adequate flu-ids (at least 4 ounces), and remains upright
for at least 10 minutes after taking medications
c. Maintains an upright
position after meals for 1 to 4 hours
d. Reports that there is
less eructation and chest pain
4) Increases knowledge
level of esophageal condition, treatment, and prognosis
a. States cause of
condition
b. Discusses rationale for
medical or surgical management and diet or medication regimen
c. Describes treatment
program
Practices preventive measures so
injuries are avoided
Related Topics