Chapter: Medical Surgical Nursing: Management of Patients With Oral and Esophageal Disorders
Nursing Process: The Patient Undergoing a Neck Dissection
NURSING
PROCESS: THE PATIENT UNDERGOING A NECK DISSECTION
Assessment
Preoperatively,
the patient’s physical and psychological prepara-tion for major surgery is
assessed, along with his or her knowl-edge of the preoperative and
postoperative procedures. Postoperatively, the patient is assessed for
complications such as altered respiratory status, wound infection, and
hemorrhage. As healing occurs, neck range of motion is assessed to determine
whether there has been a decrease in range of motion due to nerve or muscle
damage.
Diagnosis
NURSING DIAGNOSES
Based
on all the assessment data, major nursing diagnoses may include the following:
•
Deficient knowledge about preoperative and
postoperative procedures
•
Ineffective airway clearance related to obstruction
by mucus, hemorrhage, or edema
•
Acute pain related to surgical incision
•
Risk for infection related to surgical intervention
secondary to decreased nutritional status, or immunosuppression from
chemotherapy or radiation therapy
•
Impaired tissue integrity secondary to surgery and
grafting
•
Imbalanced nutrition, less than body requirements,
related to disease process or treatment
•
Situational low self-esteem related to diagnosis or
prognosis
•
Impaired verbal communication secondary to surgical
re-section
•
Impaired physical mobility secondary to nerve
injury
COLLABORATIVE PROBLEMS/POTENTIAL COMPLICATIONS
Potential
postoperative complications that may develop include the following:
1) Hemorrhage
2) Chyle fistula
3) Nerve injury
Planning and Goals
The
major goals for the patient include participation in the treat-ment plan,
maintenance of respiratory status, absence of infec-tion, viability of the
graft, maintenance of adequate intake of food and fluids, effective coping
strategies, attainment of comfort, effective communication, and absence of
complications.
Nursing Interventions
PROVIDING PREOPERATIVE PATIENT EDUCATION
Before
surgery, the patient should be informed about the nature and extent of the
surgery, and what the postoperative period will be like. The patient is
encouraged to ask questions and to express concerns about the upcoming surgery
and the expected results. During this exchange, the nurse has an opportunity to
assess the patient’s cop-ing abilities, answer questions, and develop a plan
for offering assis-tance. A sense of mutual understanding and rapport will make
the postoperative experience less traumatic for the patient. The patient’s
expressions of concern, anxieties, and fears can guide the nurse in providing
support postoperatively.
PROVIDING GENERAL POSTOPERATIVE CARE
For
the patient who has had extensive neck surgery, specific postoperative
interventions include mainte-nance of a patent airway and continuous assessment
of respiratory status, wound care and oral hygiene, maintenance of adequate nutrition,
and observation for hemorrhage or nerve injury.
MAINTAINING THE AIRWAY
After
the endotracheal tube or airway has been removed and the ef-fects of the
anesthesia have worn off, the patient may be placed in Fowler’s position to
facilitate breathing and promote comfort. This position also increases
lymphatic and venous drainage, facilitates swallowing, and decreases venous
pressure on the skin flaps.
In the
immediate postoperative period, the nurse assesses for stridor (coarse,
high-pitched sound on inspiration) by listening frequently over the trachea
with a stethoscope. This finding must be reported immediately because it
indicates obstruction of the airway. Signs of respiratory distress, such as
dyspnea, cyanosis, changes in mental status, and changes in vital signs, are
assessed because they may suggest edema, hemorrhage, inadequate oxy-genation,
or inadequate drainage.
Pneumonia
may occur in the postoperative phase if pulmonary secretions are not removed.
Coughing and deep breathing are en-couraged to aid in the removal of
secretions. The patient should assume a sitting position, with the nurse
supporting the neck so that the patient can bring up excessive secretions. If
this is in-effective, the patient’s respiratory tract may have to be suctioned.
Care is taken to protect the suture lines during suctioning. If a tra-cheostomy
tube is in place, suctioning is performed through the tube. The patient may
also be instructed on use of Yankauer suc-tion (tonsil tip suction) to remove
oral secretions. Temperature should not be taken orally.
RELIEVING PAIN
Pain
and the patient’s fear of pain are assessed and managed. Pa-tients with head
and neck cancer often report less pain than patients with other types of
cancer; however, the nurse needs to be aware that each person’s pain experience
is individual. The nurse admin-isters analgesics as prescribed and assesses
their effectiveness.
PROVIDING WOUND CARE
Wound
drainage tubes are usually inserted during surgery to pre-vent the collection
of fluid subcutaneously. The drainage tubes are connected to portable suction
device (eg, Jackson-Pratt), and the container is emptied periodically. Between
80 and 120 mL of serosanguineous secretions may drain over the first 24 hours.
Excessive drainage may be indicative of a chyle fistula or hemor-rhage (see
later discussion). If dressings are present, they may need to be reinforced
from time to time. Dressings are observed for evidence of hemorrhage and
constriction, which impairs res-piration and perfusion of the graft. The graft
is assessed for color and temperature, and for the presence of a pulse if
applicable, to determine viability. The graft should be pale pink and warm to
the touch. The surgical incisions are also assessed for infection, which is
reported immediately. Prophylactic antibiotics may be prescribed.
MAINTAINING ADEQUATE NUTRITION
Nutritional
status is assessed preoperatively; early intervention to correct nutritional
imbalances may decrease the risk of postopera-tive complications. Frequently,
nutrition is less than optimal be-cause of inadequate intake, and the patient
often requires enteral or parenteral supplements preoperatively to attain a
positive nitro-gen balance. This therapy may need to be continued
postopera-tively if the patient cannot take enough nutrients by mouth.
Supplements (eg, Ensure, Sustacal) that are nutritionally dense may help
reestablish a positive nitrogen balance. They may be taken en-terally by mouth,
by nasogastric feeding tube, or by gastrostomy feeding tube. (See the Plan of
Nursing Care for further discussion.)
The
patient who is able to chew may take food by mouth; the level of the patient’s
chewing ability will determine whether some diet modification (eg, soft,
pureed, or liquid foods) is necessary. Food preferences should also be
discussed with the patient. Oral care before eating may enhance the patient’s
appetite, and oral care after eating is important to prevent infection and
dental caries. Most patients are able to maintain and gain weight.
SUPPORTING COPING MEASURES
Preoperatively,
information about the planned surgery is given to the patient and family. The
psychological postoperative nursing intervention is aimed at supporting the
patient who has had a change in body image or who has major concerns regarding
the prognosis. The patient may have difficulty communicating and may be
concerned about his or her ability to breathe and swallow normally. The nurse
enlists the support of family or friends in en-couraging and reassuring the
patient that adjusting to the results of this surgery will take time.
The
person who has had extensive neck surgery often is sensi-tive about his or her
appearance. This can occur when the oper-ative area is covered by bulky
dressings, when the incision line is visible, or later after healing has
occurred but the appearance of the neck and possibly the lower face has been
significantly altered. If the nurse accepts the patient’s appearance and
expresses a pos-itive, optimistic attitude, the patient is more likely to be
encour-aged. The patient also needs an opportunity to express concerns
regarding the success of the surgery and the prognosis. The Amer-ican Cancer
Society may be a resource to provide a volunteer to meet with the patient
either preoperatively or postoperatively.
People
with cancer of the head and neck frequently have used alcohol or tobacco before
surgery; postoperatively, the patient is encouraged to abstain from these
substances. Alternative methods of coping need to be explored. A referral to
Alcoholics Anonymous may be appropriate.
PROMOTING EFFECTIVE COMMUNICATION
If a
laryngectomy was performed, the nurse explores other methods of communicating
with the patient and obtains a con-sultation with a speech/language therapist.
Alternatives to verbal communication may include use of a pencil and paper or
point-ing to needed items on a picture pad. Alternative speech tech-niques,
such as an electrolarynx (a mechanical device held against the neck) or
esophageal speech, may be taught by a speech/language therapist.
MAINTAINING PHYSICAL MOBILITY
Excision
of muscles and nerves results in weakness at the shoulder that can cause
shoulder drop, a forward curvature of the shoulder. Many problems can be
avoided with a conscientious exercise pro-gram. These exercises are usually begun
after the drains have been removed and the neck incision is sufficiently
healed. The purpose of the exercises depicted in Figure 35-5 is to promote
maximal shoulder function and neck motion after surgery. Physical thera-pists
and occupational therapists can assist patients in performing these exercises.
MONITORING AND MANAGING POTENTIAL COMPLICATIONS
Hemorrhage
Hemorrhage
may occur from carotid artery rupture as a result of necrosis of the graft or
damage to the artery itself from tumor or infection. The following measures are
indicated:
•
Vital signs are assessed. Tachycardia, tachypnea,
and hy-potension may indicate hemorrhage and impending hypo-volemic shock.
•
The patient is instructed to avoid the Valsalva
maneuver to prevent stress on the graft and carotid artery.
•
Signs of impending rupture, such as high epigastric
pain or discomfort, are reported.
•
Dressings and wound drainage are observed for
excessive bleeding.
•
If hemorrhage occurs, assistance is summoned immediately.
•
Hemorrhage requires the continuous application of
pressure to the bleeding site or major associated vessel.
•
Although some advocate placing the patient in
modified Trendelenburg position to maintain blood pressure, others recommend
that the head of the patient’s bed be elevated to maintain airway patency and
prevent aspiration.
•
A controlled, calm manner will allay the patient’s
anxiety.
•
The surgeon is notified immediately, because a
vascular or ligature tear requires surgical intervention.
Chyle Fistula
A
chyle fistula (milk-like drainage from the thoracic duct into the thoracic
cavity) may develop as a result of damage to the tho-racic duct during surgery.
The diagnosis is made if there is ex-cess drainage which has a 3% fat content
and a specific gravity of 1.012 or greater. Treatment of a small leak (500 mL
or less) includes application of a pressure dressing and a diet of medium-chain
fatty acids or parenteral nutrition. Surgical intervention to repair the
damaged duct is necessary for larger leaks.
Nerve Injury
Nerve
injury can occur if the cervical plexus or spinal accessory nerves are severed
during surgery. Because lower facial paralysis may occur as a result of injury
to the facial nerve, this complica-tion is observed for and reported. Likewise,
if the superior laryn-geal nerve is damaged, the patient may have difficulty
swallowing liquids and food because of the partial lack of sensation of the
glottis. Speech therapy may be indicated to assist with the prob-lems related
to nerve injury.
PROMOTING HOME AND COMMUNITY-BASED CARE
Teaching Patients Self-Care
The
patient and care provider will require instructions about management of the
wound, the dressing, and any drains that re-main in place. Patients who require
oral suctioning or who have a tracheostomy may be very anxious about their care
at home; the transition to home can be eased if the care provider is given
sev-eral opportunities to demonstrate the ability to meet the patient’s needs
(Chart 35-3).
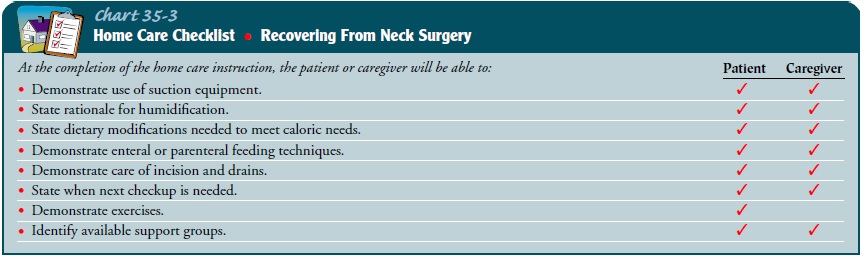
If the patient cannot take food by mouth, detailed instructions and demonstration of enteral or parenteral feedings will be required. Education in techniques of effective oral hygiene is also important.
Continuing Care
A
referral for home care nursing may be necessary in the early pe-riod after
discharge. The nurse will assess healing, ensure that feedings are being
administered properly, and detect any compli-cations. The home care nurse
assesses the patient’s adjustment to changes in physical appearance and status,
ability to communi-cate, and ability to eat normally. Physical and speech
therapy also may be continued at home.
The
patient is given information regarding local support groups such as “I Can
Cope” or “New Voice Club,” if indicated.
Evaluation
EXPECTED PATIENT OUTCOMES
Expected
patient outcomes may include:
1) Discusses expected
course of treatment
2) Demonstrates good
respiratory exchange
i.
Lungs are clear to auscultation
ii.
Breathes easily with no shortness of breath
iii.
Demonstrates ability to use suction effectively
3) Remains free of
infection
i.
Maintains normal laboratory values
ii.
Is afebrile
4) Graft is pink and warm
to touch
5) Maintains adequate
intake of foods and fluids
i.
Accepts altered route of feeding
ii.
Is well hydrated
iii.
Maintains or gains weight
6) Demonstrates ability to
cope
a.
Discusses emotional responses to the diagnosis
b.
Attends support group meetings
7) Verbalizes comfort
8) Attains maximal mobility
i.
Adheres to physical therapy exercises
ii.
Attains maximal range of motion
The
Plan of Nursing Care presents an overview of the care of a patient undergoing a
neck dissection.
Related Topics