Chapter: Medical Surgical Nursing: Management of Patients With Oral and Esophageal Disorders
Achalasia - Disorders of the Esophagus
ACHALASIA
Achalasia is absent or ineffective peristalsis of the
distal esopha-gus, accompanied by failure of the esophageal sphincter to relax
in response to swallowing. Narrowing of the esophagus just above the stomach
results in a gradually increasing dilation of the esoph-agus in the upper
chest. Achalasia may progress slowly and occurs most often in people 40 years
of age or older.
Clinical Manifestations
The
primary symptom of achalasia is difficulty in swallowing both liquids and
solids. The patient has a sensation of food sticking in the lower portion of
the esophagus. As the condition progresses, food is commonly regurgitated,
either spontaneously or intention-ally by the patient to relieve the discomfort
produced by prolonged distention of the esophagus by food that will not pass
into the stomach. The patient may also complain of chest pain and heart-burn (pyrosis). Pain may or may not be
associated with eating. There may be secondary pulmonary complications from
aspiration of gastric contents.
Assessment and Diagnostic Findings
X-ray studies show esophageal dilation above the narrowing at the gastroesophageal junction. Barium swallow, computed tomography (CT) of the esophagus, and endoscopy may be used for diagnosis; however, the diagnosis is confirmed by manometry, a process in which the esophageal pressure is measured by a radiologist or gas-troenterologist.
Management
The
patient should be instructed to eat slowly and to drink flu-ids with meals. As
a temporary measure, calcium channel block-ers and nitrates have been used to
decrease esophageal pressure and improve swallowing. Injection of botulinum
toxin (Botox) to quadrants of the esophagus via endoscopy has been helpful
because it inhibits the contraction of smooth muscle. Periodic injections are
required to maintain remission. If these methods are unsuccessful, pneumatic
(forceful) dilation or surgical sep-aration of the muscle fibers may be
recommended (Streeter, 1999; Annese et al., 2000).
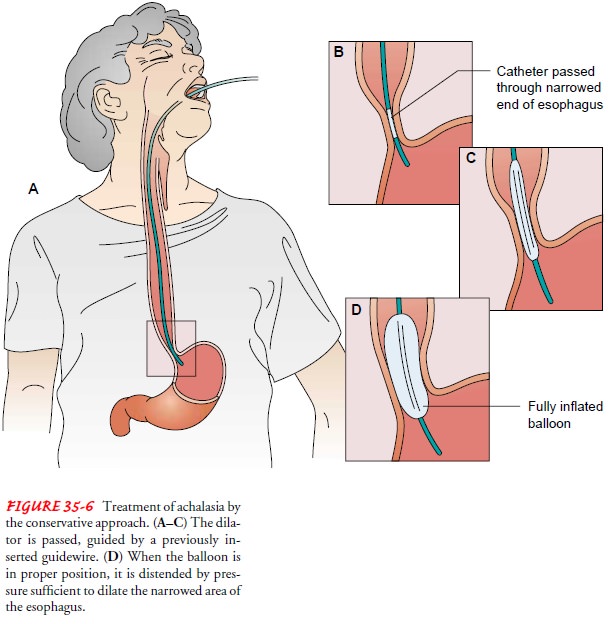
Achalasia
may be treated conservatively by pneumatic dilation to stretch the narrowed
area of the esophagus (Fig. 35-6). Pneu-matic dilation has a high success rate.
Although perforation is a potential complication, its incidence is low. The
procedure can be painful; therefore, moderate sedation in the form of an
anal-gesic or tranquilizer, or both, is administered for the treatment. The
patient is monitored for perforation. Complaints of abdom-inal tenderness and
fever may be indications of perforation (see later discussion).
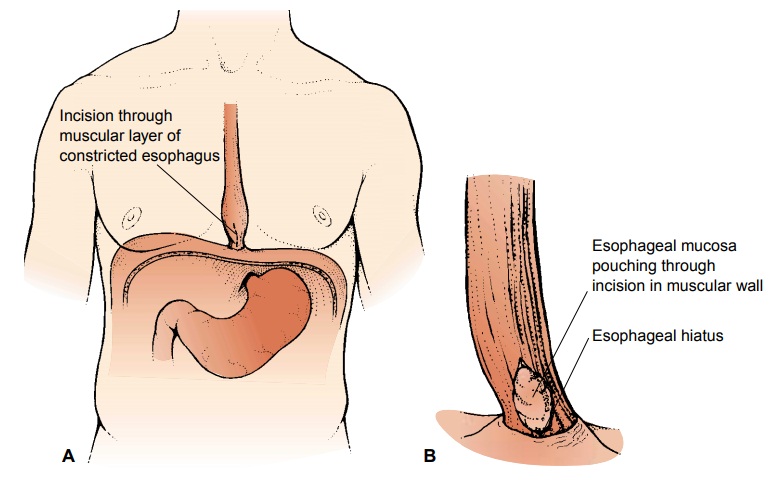
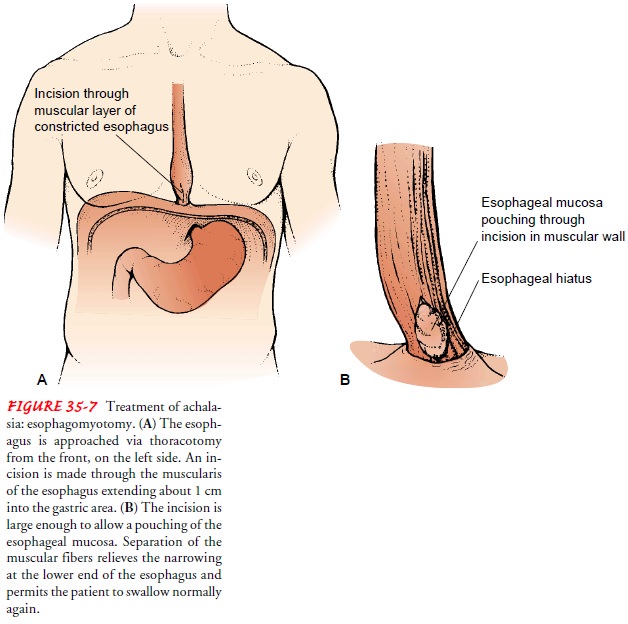
Achalasia
may be treated surgically by esophagomyotomy (Fig. 35-7). The procedure usually
is performed laparoscopically, either with a complete lower esophageal
sphincter myotomy and an antireflux procedure (see later discussion of
fundoplasty), or without an antireflux procedure. The esophageal muscle fibers
are separated to relieve the lower esophageal stricture. Although pa-tients
with a history of achalasia have a slightly higher incidence of esophageal
cancer, long-term follow-up with esophagoscopy for early detection has not
proved beneficial.
Related Topics