Chapter: Medical Surgical Nursing: Management of Patients With Oral and Esophageal Disorders
Benign Tumors and Cancer of the Esophagus
BENIGN TUMORS OF THE ESOPHAGUS
Benign
tumors can arise anywhere along the esophagus. The most common lesion is a
leiomyoma (tumor of the smooth muscle), which can occlude the lumen of the
esophagus. Most benign tu-mors are asymptomatic and are distinguished from cancerous
le-sions by a biopsy. Small lesions are excised during esophagoscopy; lesions
that occur within the wall of the esophagus may require treatment via a
thoracotomy.
CANCER OF THE ESOPHAGUS
In the
United States, carcinoma of the esophagus occurs more than three times as often
in men as in women. It is seen more fre-quently in African Americans than in
Caucasians and usually oc-curs in the fifth decade of life. Cancer of the
esophagus has a much higher incidence in other parts of the world, including
China and northern Iran (Greenlee, 2001; Castell & Richter, 1999).
Chronic
irritation is a risk factor for esophageal cancer. In the United States, cancer
of the esophagus has been associated with ingestion of alcohol and with the use
of tobacco. There seems to be an association between GERD and adenocarcinoma of
the esophagus. People with Barrett’s esophagus (which is caused by chronic
irritation of mucous membranes due to reflux of gastric and duodenal contents)
have a higher incidence of esophageal cancer (Stein, 1999).
Pathophysiology
Esophageal
cancer is usually of the squamous cell epidermoid type; however, the incidence
of adenocarcinoma of the esopha-gus is increasing in the United States. Tumor
cells may spread be-neath the esophageal mucosa or directly into, through, and
beyond the muscle layers into the lymphatics. In the latter stages,obstruction
of the esophagus is noted, with possible perforation into the mediastinum and
erosion into the great vessels.
Clinical Manifestations
Many
patients have an advanced ulcerated lesion of the esopha-gus before symptoms
are manifested. Symptoms include dyspha-gia, initially with solid foods and
eventually with liquids; a sensation of a mass in the throat; painful
swallowing; substernal pain or fullness; and, later, regurgitation of
undigested food with foul breath and hiccups. The patient first becomes aware
of in-termittent and increasing difficulty in swallowing. As the tumor
progresses and the obstruction becomes more complete, even liq-uids cannot pass
into the stomach. Regurgitation of food and saliva occurs, hemorrhage may take
place, and progressive loss of weight and strength occurs from starvation.
Later symptoms in-clude substernal pain, persistent hiccup, respiratory
difficulty, and foul breath. The delay between the onset of early symptoms and
the time when the patient seeks medical advice is often 12 to 18 months. Anyone
with swallowing difficulties should be en-couraged to consult a physician
immediately.
Assessment and Diagnostic Findings
Although
new endoscopic techniques are being studied for screening and diagnosis of
esophageal cancer, currently diagno-sis is confirmed most often by EGD with
biopsy and brushings. Bronchoscopy usually is performed, especially in tumors
of the middle and the upper third of the esophagus, to determine whether the
trachea has been affected and to help determine whether the le-sion can be
removed. Endoscopic ultrasound or mediastinoscopy is used to determine whether
the cancer has spread to the nodes and other mediastinal structures. Cancer of
the lower end of the esophagus may be caused by adenocarcinoma of the stomach
that extends upward into the esophagus.
Medical Management
If
esophageal cancer is found at an early stage, treatment goals may be directed toward
cure; however, it is often found in late stages, making relief of symptoms the
only reasonable goal of therapy. Treatment may include surgery, radiation,
chemotherapy, or a com-bination of these modalities, depending on the extent of
the disease.
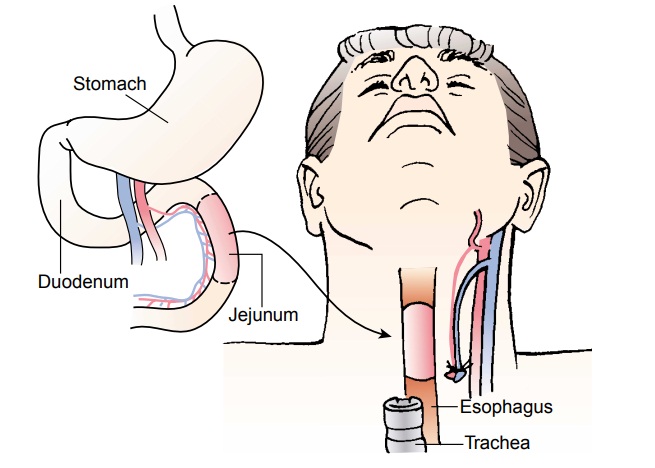
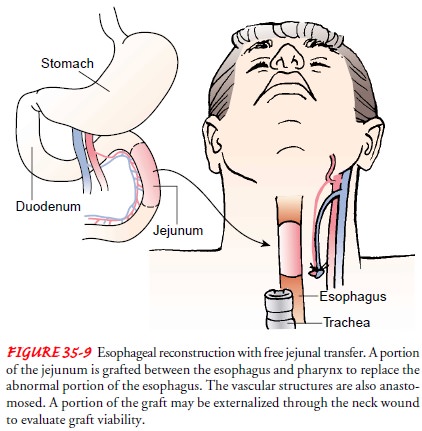
Standard
surgical management includes a total resection of the esophagus (esophagectomy)
with removal of the tumor plus a wide tumor-free margin of the esophagus and
the lymph nodes in the area. The surgical approach may be through the thorax or
the abdomen, depending on the location of the tumor. When tu-mors occur in the
cervical or upper thoracic area, esophageal con-tinuity may be maintained by
free jejunal graft transfer, in which the tumor is removed and the area is
replaced with a portion of the jejunum (Fig. 35-9). A segment of the colon may
be used, or the stomach can be elevated into the chest and the proximal section
of the esophagus anastomosed to the stomach.
Tumors
of the lower thoracic esophagus are more amenable to surgery than are tumors
located higher in the esophagus, and gastrointestinal tract integrity is
maintained by anastomosing the lower esophagus to the stomach.
Surgical resection of the esophagus has a relatively high mor-tality rate because of infection, pulmonary complications, or leak-age through the anastomosis. Postoperatively, the patient will have a nasogastric tube in place that should not be manipulated. The patient is given nothing by mouth until x-ray studies confirm that the anastomosis is secure and not leaking. Preoperative radiation therapy or chemotherapy, or both, may be used; however, treatment is based on type of cell, tumor spread, and patient condition.
Palliative
treatment may be necessary to keep the esophagus open, to assist with
nutrition, and to control saliva. Palliation may be accomplished with dilation
of the esophagus, laser therapy, placement of an endoprosthesis (stent),
radiation, or chemother-apy. Because the ideal method of treating esophageal
cancer has not yet been found, treatment is individually determined.
Nursing Management
Intervention
is directed toward improving the patient’s nutri-tional and physical condition
in preparation for surgery, radia-tion therapy, or chemotherapy. A program to
promote weight gain based on a high-calorie and high-protein diet, in liquid or
soft form, is provided if adequate food can be taken by mouth. If this is not
possible, parenteral or enteral nutrition is initiated. Nutritional status is
monitored throughout treatment. The pa-tient is informed about the nature of
the postoperative equipment that will be used, including that required for
closed chest drainage, nasogastric suction, parenteral fluid therapy, and
gas-tric intubation. Immediate postoperative care is similar to that pro-vided
for patients undergoing thoracic surgery. After recovering from the effects of
anesthesia, the patient is placed in a low Fowler’s position, and later in a
Fowler’s position, to assist in preventing re-flux of gastric secretions. The
patient is observed carefully for re-gurgitation and dyspnea. A common
postoperative complication is aspiration pneumonia. The patient’s temperature
is monitored to detect any elevation that may indicate aspiration or seepage of
fluid through the operative site into the mediastinum.
If
jejunal grafting has been performed, the nurse checks for graft viability
hourly for at least the first 12 hours. To make the graft visible, the surgeon
usually brings a portion of the jejunum to the exterior neck by way of a small
incision. Moist gauze cov-ers the external portion of the graft. The gauze is
removed briefly to assess the graft for color and to assess for the presence of
a pulse by means of Doppler ultrasonography.If an endoprosthesis has been
placed or an anastomosis has been performed, a functioning continuum will exist
between the throat and the stomach. Immediately after surgery, the nasogas-tric
tube should be marked for position, and the physician is no-tified if
displacement occurs. The nurse does not attempt to reinsert a displaced
nasogastric tube, because damage to the anas-tomosis may occur. The nasogastric
tube is removed 5 to 7 days after surgery, and a barium swallow is performed to
assess for any anastomotic leak before the patient is allowed to eat.
Once
feeding begins, the nurse encourages the patient to swal-low small sips of
water and, later, small amounts of pureed food. When the patient is able to
increase food intake to an adequate amount, parenteral fluids are discontinued.
If an endoprosthesis is used, it may easily become obstructed if food is not
chewed suf-ficiently. After each meal, the patient remains upright for at least
2 hours to allow the food to move through the gastrointestinal tract. It is a
challenge to encourage the patient to eat, because ap-petite is usually poor.
Family involvement and home-cooked fa-vorite foods may help the patient to eat.
Antacids may help those with gastric distress.
If
radiation is part of the therapy, the patient’s appetite is fur-ther depressed
and esophagitis may occur, causing pain when food is eaten. Liquid supplements
may be more easily tolerated.
Often,
in either the preoperative or the postoperative period, an obstructed or nearly
obstructed esophagus causes difficulty with ex-cess saliva, so that drooling
becomes a problem. Oral suction may be used if the patient is unable to handle
oral secretions, or a wick-type gauze may be placed at the corner of the mouth
to direct se-cretions to a dressing or emesis basin. The possibility that the
patient may aspirate saliva into the tracheobronchial tree and de-velop
pneumonia is of great concern.
When
the patient is ready to go home, the family is instructed about how to promote
nutrition, what observations to make, what measures to take if complications
occur, how to keep the pa-tient comfortable, and how to obtain needed physical
and emo-tional support.
Related Topics