Chapter: Medical Surgical Nursing: Management of Patients With Oral and Esophageal Disorders
Nursing Process: The Patient With Conditions of the Oral Cavity
NURSING
PROCESS: THE PATIENT WITH CONDITIONS OF THE ORAL CAVITY
Assessment
Obtaining
a health history allows the nurse to determine the pa-tient’s learning needs
concerning preventive oral hygiene and to identify symptoms requiring medical
evaluation. The history in-cludes questions about the patient’s normal brushing
and flossing routine; frequency of dental visits; awareness of any lesions or
ir-ritated areas in the mouth, tongue, or throat; recent history of sore throat
or bloody sputum; discomfort caused by certain foods; daily food intake; use of
alcohol and tobacco, including smokeless chewing tobacco; and the need to wear
dentures or a partial plate. For more information about dentures, see the
accompanying Gerontologic Considerations box.
A
careful physical assessment follows the health history. Both the internal and
the external structures of the mouth and throat are inspected and palpated.
Dentures and partial plates are re-moved to ensure a thorough inspection of the
mouth. In general, the examination can be accomplished by using a bright light
source (penlight) and a tongue depressor. Gloves are worn to palpate the tongue
and any abnormalities.
LIPS
The
examination begins with inspection of the lips for moisture, hy-dration, color,
texture, symmetry, and the presence of ulcerations or fissures. The lips should
be moist, pink, smooth, and symmetric. The patient is instructed to open the
mouth wide; a tongue blade is then inserted to expose the buccal mucosa for an
assessment of color and lesions. Stensen’s duct of each parotid gland is
visible as a small red dot in the buccal mucosa next to the upper molars.
GUMS
The
gums are inspected for inflammation, bleeding, retraction, and discoloration.
The odor of the breath is also noted. The hard palate is examined for color and
shape.
TONGUE
The dorsum (back) of the tongue is inspected for texture, color, and lesions. A thin white coat and large, vallate papillae in a “V” formation on the distal portion of the dorsum of the tongue are normal findings. The patient is instructed to protrude the tongue and move it laterally. This provides the examiner with an opportunity to estimate the tongue’s size as well as its sym-metry and strength (to assess the integrity of the 12th cranial nerve [hypoglossal]).
Further
inspection of the ventral surface of the tongue and the floor of the mouth is
accomplished by asking the patient to touch the roof of the mouth with the tip
of the tongue. Any lesions of the mucosa or any abnormalities involving the
frenulum or su-perficial veins on the undersurface of the tongue are assessed
for location, size, color, and pain. This is a common area for oral can-cer,
which presents as a white or red plaque, an indurated ulcer, or a warty growth.
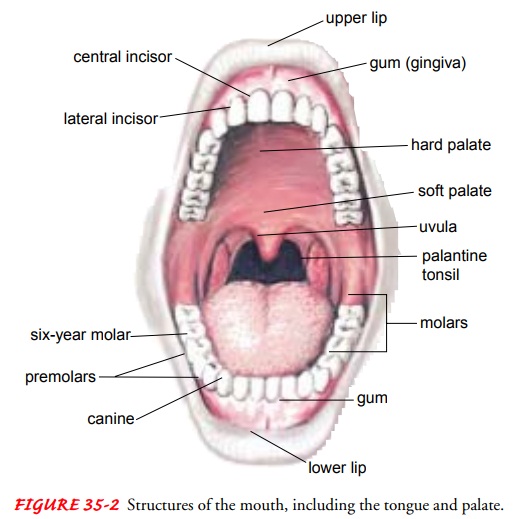
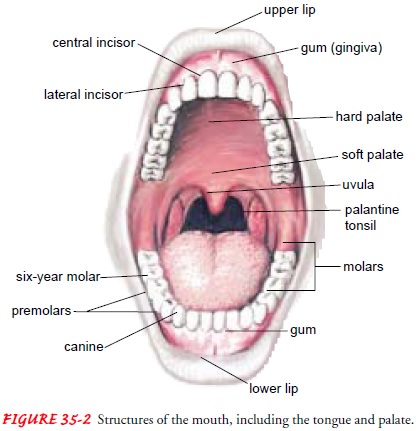
A
tongue blade is used to depress the tongue for adequate visu-alization of the
pharynx. It is pressed firmly beyond the midpoint of the tongue; proper
placement avoids a gagging response. The pa-tient is told to tip the head back,
open the mouth wide, take a deep breath, and say “ah.” Often this flattens the
posterior tongue and briefly allows a full view of the tonsils, uvula, and
posterior phar-ynx (Fig. 35-2). These structures are inspected for color,
symme-try, and evidence of exudate, ulceration, or enlargement. Normally, the
uvula and soft palate rise symmetrically with a deep inspiration or “ah”; this
indicates an intact vagus nerve (10th cranial nerve).
A
complete assessment of the oral cavity is essential because many disorders,
such as cancer, diabetes, and immunosuppres-sive conditions resulting from
medication therapy or AIDS, may be manifested by changes in the oral cavity.
The neck is examined for enlarged lymph nodes (adenopathy).
Nursing Diagnoses
Based
on all the assessment data, major nursing diagnoses may in-clude the following:
•
Impaired oral mucous membrane related to a
pathologic condition, infection, or chemical or mechanical trauma (eg,
medications, ill-fitting dentures)
•
Imbalanced nutrition, less than body requirements,
related to inability to ingest adequate nutrients secondary to oral or dental
conditions
•
Disturbed body image related to a physical change
in ap-pearance resulting from a disease condition or its treatment
•
Fear of pain and social isolation related to
disease or change in physical appearance
•
Pain related to oral lesion or treatment
•
Impaired verbal communication related to treatment
•
Risk for infection related to disease or treatment
•
Deficient knowledge about disease process and
treatment plan
Planning and Goals
The
major goals for the patient may include improved condition of the oral mucous
membrane, improved nutritional intake, at-tainment of a positive self-image,
relief of pain, identification of alternative communication methods, prevention
of infection, and understanding of the disease and its treatment.
Nursing Interventions
PROMOTING MOUTH CARE
The
nurse instructs the patient in the importance and techniques of preventive
mouth care. If a patient cannot tolerate brushing or flossing, an irrigating
solution of 1 teaspoon of baking soda to 8 ounces of warm water, half-strength
hydrogen peroxide, or nor-mal saline solution is recommended. The nurse
reinforces the need to perform oral care and provides such care to patients who
are unable to provide it for themselves.
If a
bacterial or fungal infection is present, the nurse adminis-ters the
appropriate medications and instructs the patient in how to administer the
medications at home. The nurse monitors the patient’s physical and
psychological response to treatment.
Xerostomia, dryness of the mouth, is a frequent sequela
oforal cancer, particularly when the salivary glands have been ex-posed to
radiation or major surgery. It is also seen in patients who are receiving
psychopharmacologic agents, patients with HIV in-fection, and patients who
cannot close the mouth and as a result become mouth-breathers. To minimize this
problem, the patient is advised to avoid dry, bulky, and irritating foods and
fluids, as well as alcohol and tobacco. The patient is also encouraged to
in-crease intake of fluids (when not contraindicated) and to use a hu-midifier
during sleep. The use of synthetic saliva, a moisturizing antibacterial gel
such as Oral Balance, or a saliva production stim-ulant such as Salagen may be
helpful.
Stomatitis, or mucositis, which involves inflammation
andbreakdown of the oral mucosa, is often a side effect of chemother-apy or
radiation therapy. Prophylactic mouth care is started when the patient begins
receiving treatment; however, mucositis may become so severe that a break in
treatment is necessary. If a pa-tient receiving radiation therapy has poor
dentition, extraction of the teeth before radiation treatment in the oral
cavity is often ini-tiated to prevent infection. Many radiation therapy centers
rec-ommend the use of fluoride treatments for patients receiving radiation to
the head and neck.
ENSURING ADEQUATE FOOD AND FLUID INTAKE
The patient’s weight, age, and level of activity are recorded to de-termine whether nutritional intake is adequate. A daily calorie count may be necessary to determine the exact quantity of food and fluid ingested. The frequency and pattern of eating are recorded to determine whether any psychosocial or physiologic factors are affecting ingestion.
The nurse recommends changes in the consis-tency of foods and the
frequency of eating, based on the disorder and the patient’s preferences.
Consultation with a dietitian can be helpful. The goal is to help the patient
attain and maintain desir-able body weight and level of energy, as well as to
promote the heal-ing of tissue.
SUPPORTING A POSITIVE SELF-IMAGE
A
patient who has a disfiguring oral condition or has undergone disfiguring
surgery may experience an alteration in self-image. The patient is encouraged
to verbalize the perceived change in body ap-pearance and to realistically
discuss actual changes or losses. The nurse offers support while the patient
verbalizes fears and negative feelings (withdrawal, depression, anger). The
nurse listens atten-tively and determines whether the patient’s needs are
primarily psychosocial or cognitive-perceptual. This determination will help
the nurse to individualize a plan of care. The patient’s strengths,
achievements, and positive attributes are reinforced.
The
nurse should determine the patient’s anxieties concerning relationships with
others. Referral to support groups, a psychiatric liaison nurse, a social
worker, or a spiritual advisor may be useful in helping the patient to cope
with anxieties and fears. Emphasiz-ing that the patient’s worth is not
diminished by a physical change in a body part can be a helpful approach. The
patient’s progress toward development of positive self-esteem is documented.
The nurse should be alert to signs of grieving and should record emo-tional
changes. By providing acceptance and support, the nurse encourages the patient
to verbalize feelings.
MINIMIZING PAIN AND DISCOMFORT
Oral
lesions can be painful. Strategies to reduce pain and discom-fort include
avoiding foods that are spicy, hot, or hard (eg, pretzels, nuts). The patient
is instructed about mouth care. It may be nec-essary to provide the patient
with an analgesic such as viscous lido-caine (Xylocaine Viscous 2%) or opioids,
as prescribed. The nurse can reduce the patient’s fear of pain by providing
information about pain control methods.
PROMOTING EFFECTIVE COMMUNICATION
Verbal
communication may be impaired by radical surgery for oral cancer. It is
therefore vital to assess the patient’s ability to communicate in writing
before surgery. Pen and paper are pro-vided postoperatively to patients who can
use them to commu-nicate. A communication board with commonly used words or
pictures is obtained preoperatively and given after surgery to pa-tients who
cannot write so that they may point to needed items. A speech therapist is also
consulted postoperatively.
PREVENTING INFECTION
Leukopenia
(a decrease in white blood cells) may result from ra-diation, chemotherapy,
AIDS, and some medications used to treat HIV infection. Leukopenia reduces
defense mechanisms, increas-ing the risk for infections. Malnutrition, which is
also common among these patients, may further decrease resistance to infection.
If the patient has diabetes, the risk of infection is further increased.
Laboratory
results should be evaluated frequently and the pa-tient’s temperature checked
every 4 to 8 hours for an elevation that may indicate infection. Visitors who
might transmit micro-organisms are prohibited because the patient’s immunologic
sys-tem is depressed. Sensitive skin tissues are protected from trauma to
maintain skin integrity and prevent infection. Aseptic tech-nique is necessary
when changing dressings. Desquamation (shedding of the epidermis) is a reaction
to radiation therapy that causes dryness and itching and can lead to a break in
skin integrity and subsequent infection.
As
described earlier, adequate nutrition is helpful in prevent-ing infection.
Signs of wound infection (redness, swelling, drainage, tenderness) are reported
to the physician. Antibiotics may be prescribed prophylactically.
PROMOTING HOME AND COMMUNITY-BASED CARE
Teaching Patients Self-Care
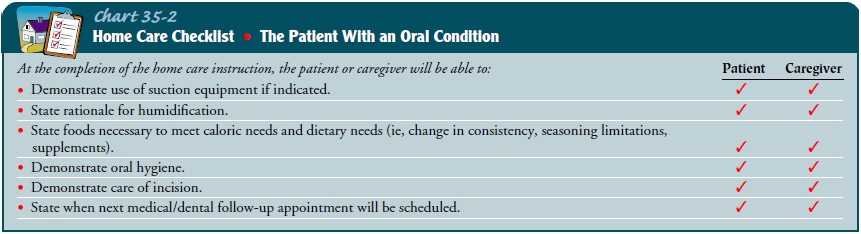
The
patient who is recovering from treatment of an oral condition is instructed
about mouth care, nutrition, prevention of infection, and signs and symptoms of
complications (Chart 35-2). Methods of preparing nutritious foods that are
seasoned according to the pa-tient’s preference and at the preferred
temperature are explained. For some patients, it may be more convenient to use
commercial baby foods than to prepare liquid and soft diets. The patient who
cannot take foods orally may receive enteral or parenteral nutrition; the
administration of these feedings is explained and demonstrated to the patient
and the care provider.
For
patients with cancer, instructions are provided in the use and care of any
prostheses. The importance of keeping dressings clean is emphasized, as is the
need for conscientious oral hygiene.
Continuing Care
The
need for ongoing care in the home depends on the patient’s condition. The
patient, the family members or others responsi-ble for home care, the nurse,
and other health care professionals (eg, speech therapist, nutritionist,
psychologist) work together to prepare an individual plan of care.
If
suctioning of the mouth or tracheostomy tube is required, the necessary equipment
is obtained and the patient and care providers are taught how to use it.
Considerations include the control of odors and humidification of the home to
keep secretions moist. The patient and the care providers are taught how to
assess for ob-struction, hemorrhage, and infection and what actions to take if
they occur. The home care nurse may provide physical care, mon-itor for changes
in the patient’s physical status (eg, skin integrity, nutritional status,
respiratory function), and assess the adequacy of pain control measures. The
nurse also assesses the patient’s and family’s ability to manage incisions,
drains, and feeding tubes and the use of recommended strategies for
communication. The abil-ity of the patient and family to accept physical,
psychological, and role changes is assessed and addressed.
Follow-up
visits to the physician are important to monitor the patient’s condition and to
determine the need for modifications in treatment and general care. The nurse
reinforces instructions in an effort to promote the patient’s self-care and
comfort.
Because
patients and their family members and health care providers tend to focus on
the most obvious needs and issues, the nurse reminds the patient and family
about the importance of continuing health promotion and screening practices.
Those pa-tients who have not been involved in these practices in the past are
educated about their importance and are referred to appropriate health care
providers.
Evaluation
EXPECTED PATIENT OUTCOMES
Expected
patient outcomes may include:
1) Shows evidence of intact
oral mucous membranes
a)
Is free of pain and discomfort in the oral cavity
b)
Has no visible alteration in membrane integrity
c)
Identifies and avoids foods that are irritating
(eg, nuts, pretzels, spicy foods)
d)
Describes measures that are necessary for
preventive mouth care
e)
Complies with medication regimen
f)
Limits or avoids use of alcohol and tobacco
(including smokeless tobacco)
2) Attains and maintains
desirable body weight
3) Has a positive
self-image
a)
Verbalizes anxieties
b)
Is able to accept change in appearance and modify
self-concept accordingly
4) Attains an acceptable
level of comfort
a)
Verbalizes that pain is absent or under control
b)
Avoids foods and liquids that cause discomfort
c)
Adheres to medication regimen
5) Has decreased fears related
to pain, isolation, and the inabil-ity to cope
a)
Accepts that pain will be managed if not eliminated
b)
Freely expresses fears and concerns
6) Is free of infection
a)
Exhibits normal laboratory values
b)
Is afebrile
c)
Performs oral hygiene after every meal and at bedtime
7) Acquires information
about disease process and course of treatment
Related Topics