Chapter: Medical Surgical Nursing: Management of Patients With Oral and Esophageal Disorders
Cancer of the Oral Cavity
Cancer of the Oral Cavity
Cancers
of the oral cavity, which can occur in any part of the mouth or throat, are
curable if discovered early. These cancers are associated with the use of
alcohol and tobacco. The combi-nation of alcohol and tobacco seems to have a
synergistic carcinogenic effect. About 95% of cases of oral cancer occur in
people older than 40 years of age, but the incidence is increas-ing in men
younger than age 30 because of the use of smokeless tobacco, especially snuff
(Centers for Disease Control and Pre-vention, 2002).
Cancer
of the oral cavity accounts for less than 2% of all can-cer deaths in the
United States. Men are afflicted more often than women; however, the incidence
of oral cancer in women is increasing, possibly because they use tobacco and
alcohol more frequently than they did in the past. The 5-year survival rate for
cancer of the oral cavity and pharynx is 55% for whites and 33% for African
Americans. Of the 7400 annual deaths from oral cancer, the distribution by site
is estimated as follows: tongue, 1700; mouth, 2000; pharynx, 2100; other, 1600
(American Cancer Society, Cancer Facts and Figures, 2002).
Chronic
irritation by a warm pipestem or prolonged exposure to the sun and wind may
predispose a person to lip cancer. Pre-disposing factors for other oral cancers
are exposure to tobacco (including smokeless tobacco), ingestion of alcohol,
dietary defi-ciency, and ingestion of smoked meats.
Pathophysiology
Malignancies
of the oral cavity are usually squamous cell cancers. Any area of the
oropharynx can be a site for malignant growths, but the lips, the lateral
aspects of the tongue, and the floor of the mouth are most commonly affected.
Clinical Manifestations
Many
oral cancers produce few or no symptoms in the early stages. Later, the most
frequent symptom is a painless sore or mass that will not heal. A typical
lesion in oral cancer is a painless indurated (hardened) ulcer with raised
edges. Tissue from any ulcer of the oral cavity that does not heal in 2 weeks
should be ex-amined through biopsy. As the cancer progresses, the patient may
complain of tenderness; difficulty in chewing, swallowing, or speaking;
coughing of blood-tinged sputum; or enlarged cervical lymph nodes.
Assessment and Diagnostic Findings
Diagnostic
evaluation consists of an oral examination as well as an assessment of the
cervical lymph nodes to detect possible metastases. Biopsies are performed on
suspicious lesions (those that have not healed in 2 weeks). High-risk areas
include the buccal mu-cosa and gingiva for people who use snuff or smoke cigars
or pipes. For those who smoke cigarettes and drink alcohol, high-risk areas
include the floor of the mouth, the ventrolateral tongue, and the soft palate
complex (soft palate, anterior and posterior tonsillar area, uvula, and the
area behind the molar and tongue junction).
Medical Management
Management
varies with the nature of the lesion, the preference of the physician, and
patient choice. Surgical resection, radiation therapy, chemotherapy, or a
combination of these therapies may be effective.
In
cancer of the lip, small lesions are usually excised liberally; larger lesions
involving more than one third of the lip may be more appropriately treated by
radiation therapy because of su-perior cosmetic results. The choice depends on
the extent of the lesion and what is necessary to cure the patient while
preserving the best appearance. Tumors larger than 4 cm often recur.
Cancer
of the tongue may be treated with radiation therapy and chemotherapy to
preserve organ function and maintain quality of life. A combination of
radioactive interstitial implants (surgical implantation of a radioactive
source into the tissue ad-jacent to or at the tumor site) and external beam
radiation may be used. If the cancer has spread to the lymph nodes, the
sur-geon may perform a neck dissection. Surgical treatments leave a less
functional tongue; surgical procedures include hemiglossec-tomy (surgical
removal of half of the tongue) and total glossectomy (removal of the tongue).
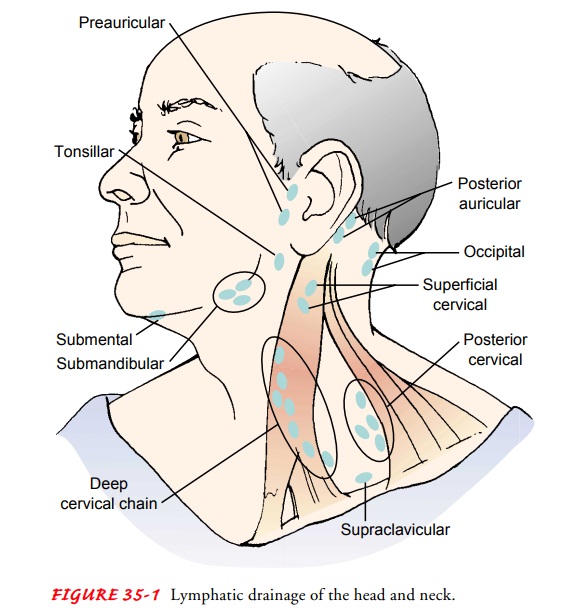
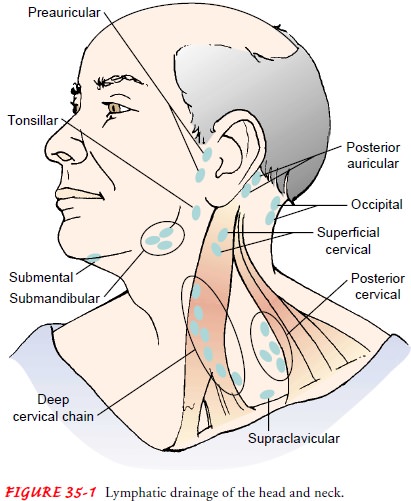
Often cancer of the oral cavity has metastasized through the extensive lymphatic channel in the neck region (Fig. 35-1), re-quiring a neck dissection and reconstructive surgery of the oral cavity. A common reconstructive technique involves use of a radial forearm free flap (a thin layer of skin from the forearm along with the radial artery).
Nursing Management
The
nurse assesses the patient’s nutritional status preoperatively, and a dietary
consultation may be necessary. The patient may re-quire enteral (through the
intestine) or parenteral (intravenous) feedings before and after surgery to
maintain adequate nutrition. If a radial graft is to be performed, an Allen
test on the donor arm must be performed to ensure that the ulnar artery is
patent and can provide blood flow to the hand after removal of the radial
artery. The Allen test is performed by asking the patient to make a fist and
then manually compressing the ulnar artery. The pa-tient is then asked to open
the hand into a relaxed, slightly flexed position. The palm will be pale.
Pressure on the ulnar artery is re-leased. If the ulnar artery is patent, the
palm will flush within about 3 to 5 seconds.
Postoperatively,
the nurse assesses for a patent airway. The pa-tient may be unable to manage
oral secretions, making suction-ing necessary. If grafting was included in the
surgery, suctioning must be performed with care to prevent damage to the graft.
The graft is assessed postoperatively for viability. Although color should be
assessed (white may indicate arterial occlusion, and blue mottling may indicate
venous congestion), it can be difficult to assess the graft by looking into the
mouth. A Doppler ultra-sound device may be used to locate the radial pulse at
the graft site and to assess graft perfusion.
Related Topics