Chapter: Surgical Pathology Dissection : The Female Genital System
Hysterectomy for Nonmalignant Disease - Uterus : Surgical Pathology Dissection
Hysterectomy for Nonmalignant Disease
zpThe
category of hysterectomy of nonmalig-nant disease includes hysterectomies for
uterine prolapse, persistent abnormal bleeding, intracta-ble pelvic pain,
leiomyomas, and endometrial hy-perplasia. The procedure can be performed either
vaginally or abdominally. The fallopian tubes and ovaries may also be present.
Orient
the uterus by identifying the stubs of the round ligaments that insert anterior
to the fallopian tubes. The ovaries should lie posteri-orly. In addition,
because the anterior peritoneum reflects onto the bladder, the anterior
perito-neum does not extend as far inferiorly along the uterus as does the
posterior peritoneum. Vaginal and abdominal hysterectomies may be distin-guished
by examining the peritoneal surface in the region of the posterior cul-de-sac.
The peri-toneum appears V-shaped in a vaginal and U-shaped in an abdominal
hysterectomy specimen.![]()
If the
adnexa are present, remove them from the right and left cornual regions, and
examine them separately. Weigh the uterus, and record the following
measurements: fundus to ectocervix, cornu to cornu, and anterior to posterior.
Measure the length of the cervix from the level of the internal os to the
ectocer-vix and the diameter of the cervix from side to side and from anterior
to posterior.
The
uterus can now be evaluated with a sys-tematic examination of each of its main
compo-nents. Begin by examining the uterine serosa. Look for and describe any
adhesions or small ‘‘powder burn’’ spots, which may signify endo-metriosis.
These may be seen more frequently on the posterior aspect.
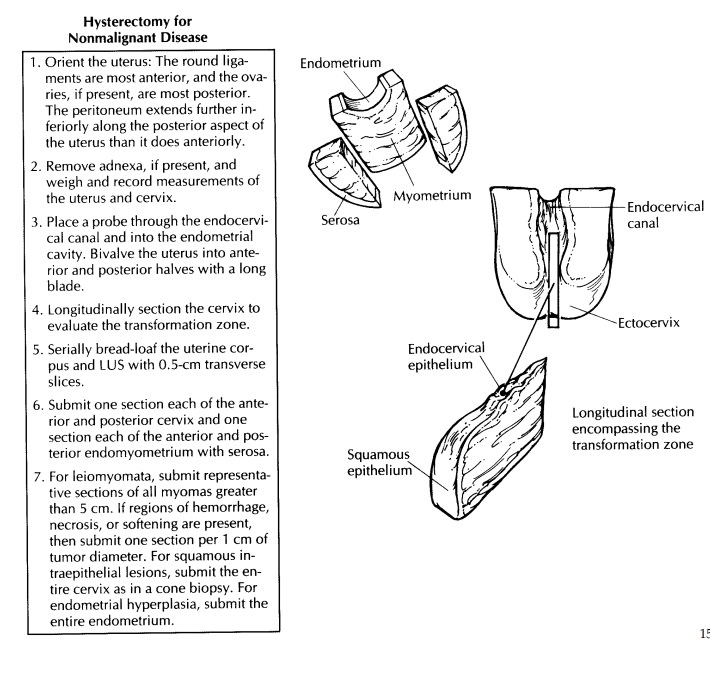
Next,
evaluate the cervix. Note the shape of the external os, which is usually
circular in nul-liparous women and slit-like in parous women. Examine the
ectocervix for any lacerations, scars, masses, ulcers, or cysts. Place a probe
through the cervical canal and into the endometrial cavity. Beginning at the
cervix, incise the uterus with a large blade using the probe as a guide to
divide it into anterior and posterior halves. Another method for bivalving the
uterus is to use a pair of scissors to cut along the lateral margins from the
ectocervix to the cornu. Gently remove the excess mucus from the endocervical
canal, and examine it for the presence of polyps. At this point, the uterus may
be photographed and then pinned to a wax tablet for fixation. Be sure to avoid
placing pins through the mucosal surfaces. After fixation, longitudinally
section the cervix at 0.2- to 0.3-cm intervals, and evaluate the transformation
zone and stroma.
Now, measure the thickness of the endome-trium, and look for any unusual thickenings or polyps. Keep in mind the age and reproductive status of the patient. If the woman is postmeno-pausal, an endometrial thickness greater than 2 mm may signify a hyperplastic process. Con-versely, a thick endometrium in a premenopausal woman may reflect only the normal secretory phase.
The
myometrium is examined last. Make serial 0.5-cm-thick transverse cuts through
the uterine corpus and lower uterine segment, and record the maximum myometrial
thickness. Look for intramural leiomyomas or evidence of adeno-myosis.
Adenomyosis is usually more extensive in the posterior wall and may be
recognized by a thickened wall with trabeculations and small hemorrhagic or
cystic foci.
If no
lesions are identified, standard sections of the uterus include longitudinal
sections of the anterior and posterior cervix (including the transformation zone)
and full-thickness sec-tions of the anterior and posterior walls of the uterus
to include endometrium, myometrium, and serosa. At our institution, sections of
the anterior and posterior lower uterine segment regions are routinely
submitted as well.
Additional
sampling may also be required if the standard sections reveal either
endometrial hyperplasia or a cervical intraepithelial lesion. In the case of
endometrial hyperplasia, the en-tire endometrium may need to be evaluated to
rule out an invasive process. Multiple thin strips of endometrium with only a
small amount of underlying myometrium can be submitted in a limited number of
tissue cassettes. If a high-grade squamous intraepithelial lesion is
iden-tified, the cervix should be processed and submitted as described for cone
biopsies. For low-grade squamous intraepithelial lesions, a section from each
quadrant may suffice.
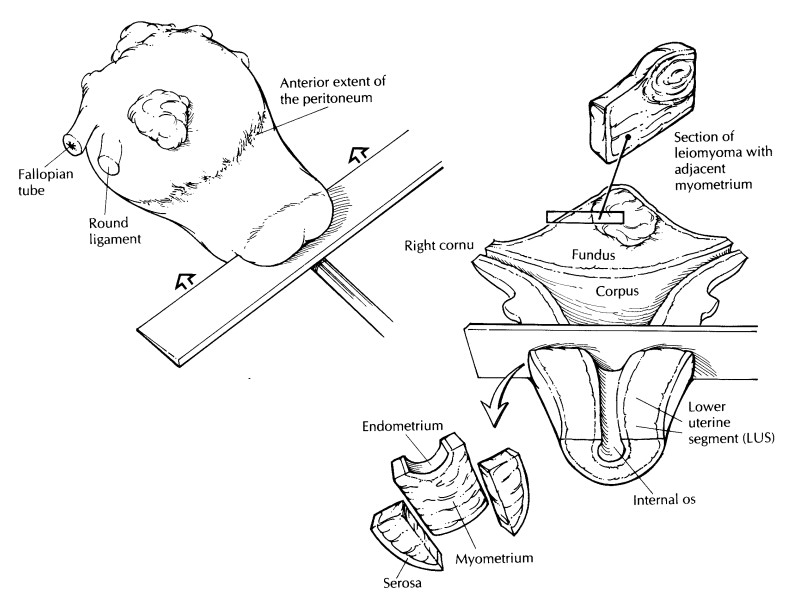
The
evaluation of a uterus with multiple leio-myomas deserves special mention. A
leiomyo-matous uterus is one of the most frequently encountered specimens, and
the gross exam-ination of these specimens is the key to their proper handling.
Orient, weigh, measure, and section the uterus as described above. Record the
number of nodules present and their size. Specifically state whether they are
submucosal, intramural, or subserosal in location. All nodules should be
sectioned at 1- to 2-cm intervals and examined grossly but not necessarily
microscopi-cally. Benign leiomyomas are firm and white with a whorled cut
surface. Their border with the surrounding myometrium is smooth and
well-circumscribed. If these criteria are met, representative sampling of each
leiomyoma is sufficient. Always include sections demonstrat-ing the border
between the leiomyoma and the surrounding myometrium or overlying endome-trium.
Any leiomyomas with areas of hemor-rhage, necrosis, or softening need to be
sampled more extensively. In these cases, the general rule of one section per 1
cm of tumor diameter should be followed. Smooth muscle tumors less than 5 cm do
not need to be sampled, as they rarely metastasize, regardless of their
micro-scopic appearance.![]()
Important Issues to Address in Your Surgical Pathology Report on Hysterectomies for Non-Malignant Disease
· What
procedure was performed, and what structures/organs are present?
· Cervix:
Are any preinvasive or invasive lesions identified?
· Endometrium:
Is the endometrium hyper-plastic, atrophic, or functional? If functional,
specify whether it is in the proliferative or secretory phase. Are any polyps
present?
· Myometrium:
Are any leiomyomas or regions of adenomyosis identified? Specify whether the
leiomyomas are submucosal, intramural, or subserosal.
· Serosa:
Are any adhesions or regions of endo-metriosis identified?
Related Topics