Chapter: Essentials of Anatomy and Physiology: Reproductive System
Female Reproductive System
FEMALE REPRODUCTIVE SYSTEM
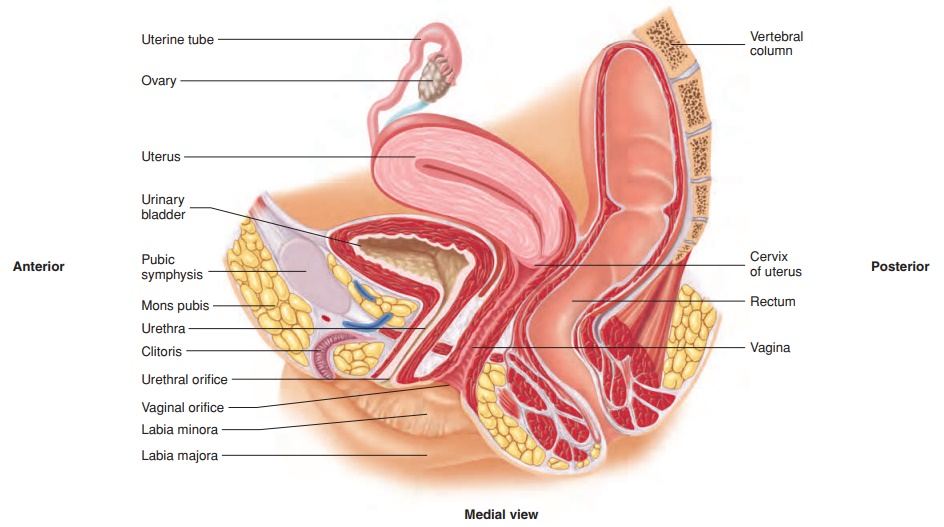
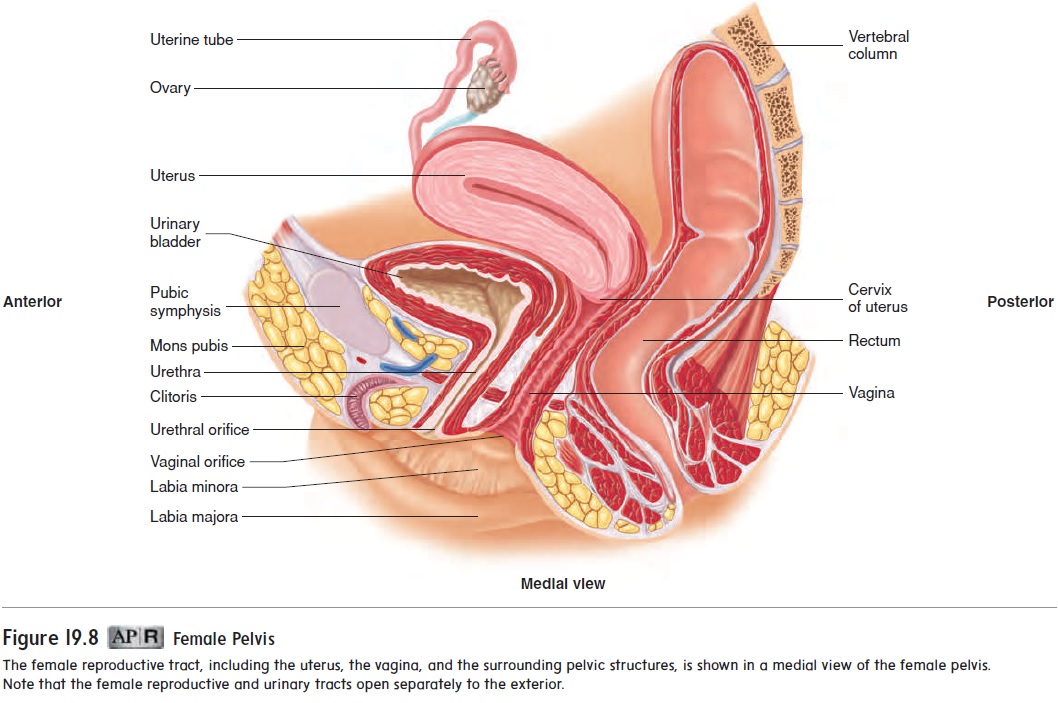
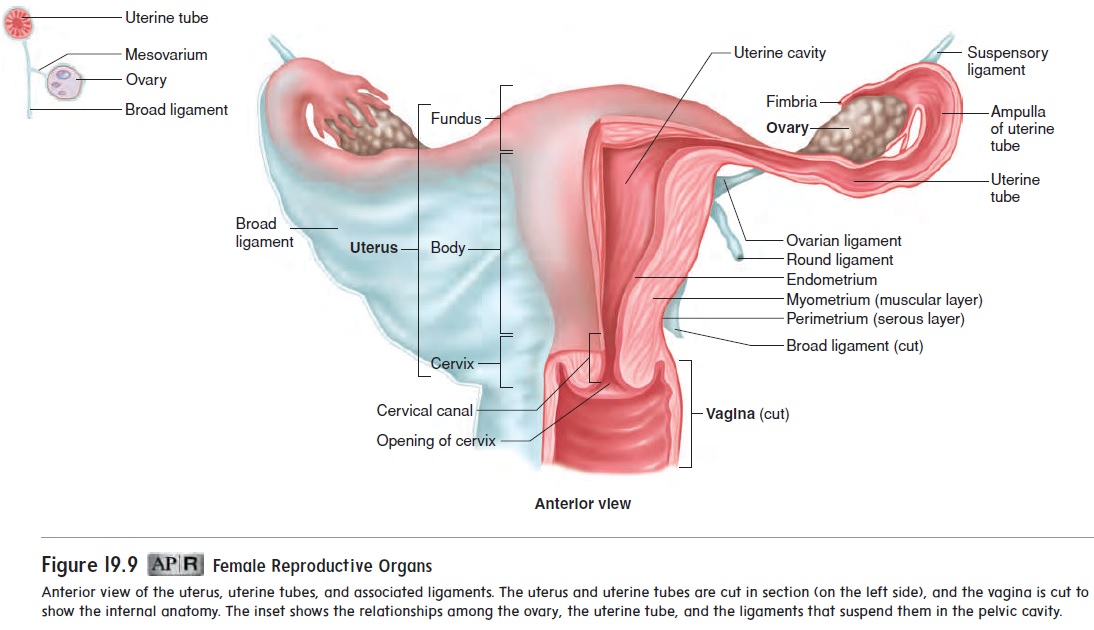
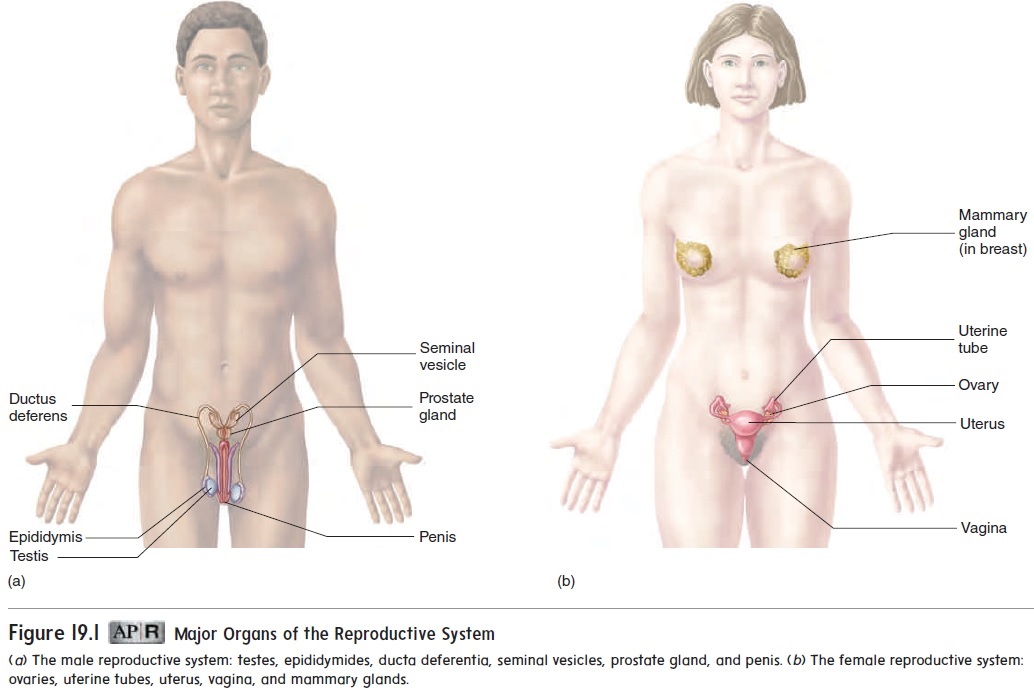
The female reproductive organs consist of the ovaries, the uter-ine tubes (or fallopian tubes), the uterus, the vagina, the external genitalia, and the mammary glands (see figure 19.1b). The internal reproductive organs of the female are located within the pelvis, between the urinary bladder and the rectum (figure 19.8). The uterus and the vagina are in the midline, with an ovary to each side of the uterus (figure 19.9). The internal reproductive organs are held in place within the pelvis by a group of ligaments. The most conspicuous is the broad ligament, which spreads out on both sides of the uterus and attaches to the ovaries and uterine tubes.
Ovaries
The two ovaries (̄o ′ v̆a -r̄e z; ovum, egg) are small organs suspended in the pelvic cavity by ligaments. The suspensory ligament extends from each ovary to the lateral body wall, and the ovarianligamentattaches the ovary to the superior margin of the uterus(figure 19.9). In addition, the ovaries are attached to the poste-rior surface of the broad ligament by folds of peritoneum called the mesovarium (mez′ ̄o -v̄a ′ r̄e -̆u m). The ovarian arteries, veins, and nerves traverse the suspensory ligament and enter the ovary through the mesovarium.
A layer of visceral peritoneum covers the surface of the ovary. The outer part of the ovary is composed of dense connective tissue and contains ovarian follicles (figure 19.10). Each of the ovarian
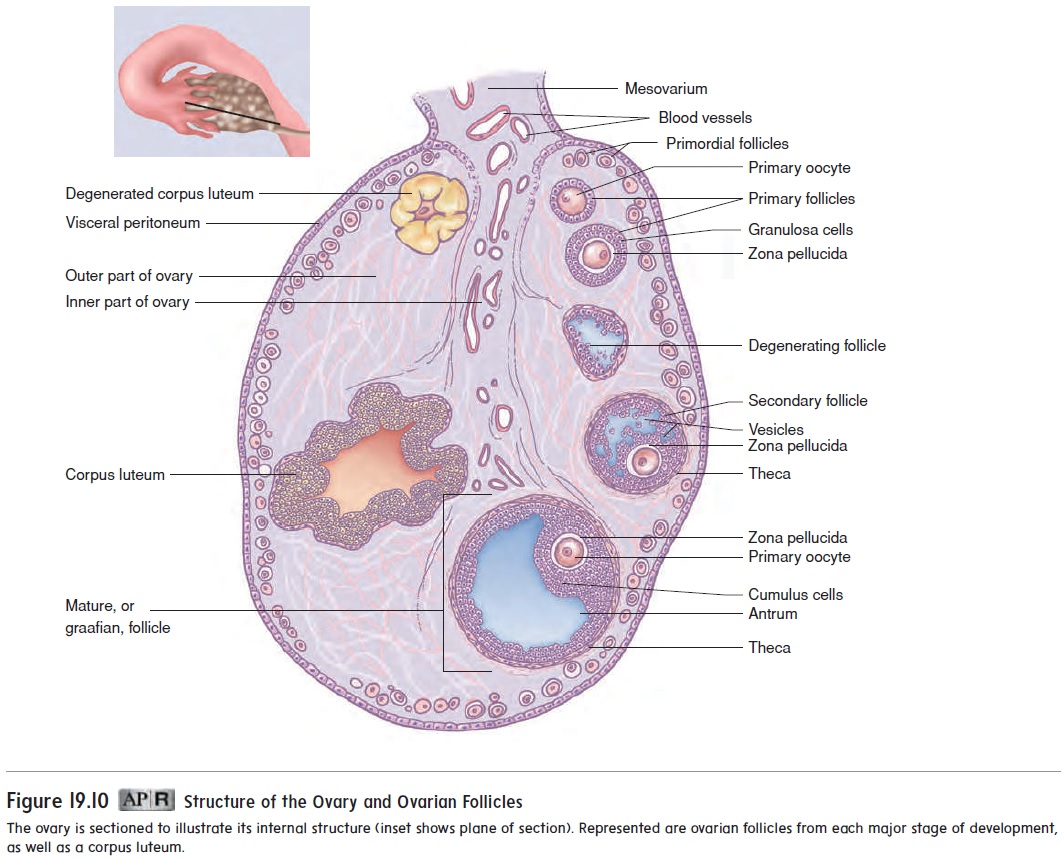
follicles contains an oocyte (ō′ ō-sı̄t; o¯on, egg), the female sex cell. Loose connective tissue makes up the inner part of the ovary, where blood vessels, lymphatic vessels, and nerves are located.
Oogenesis and Fertilization
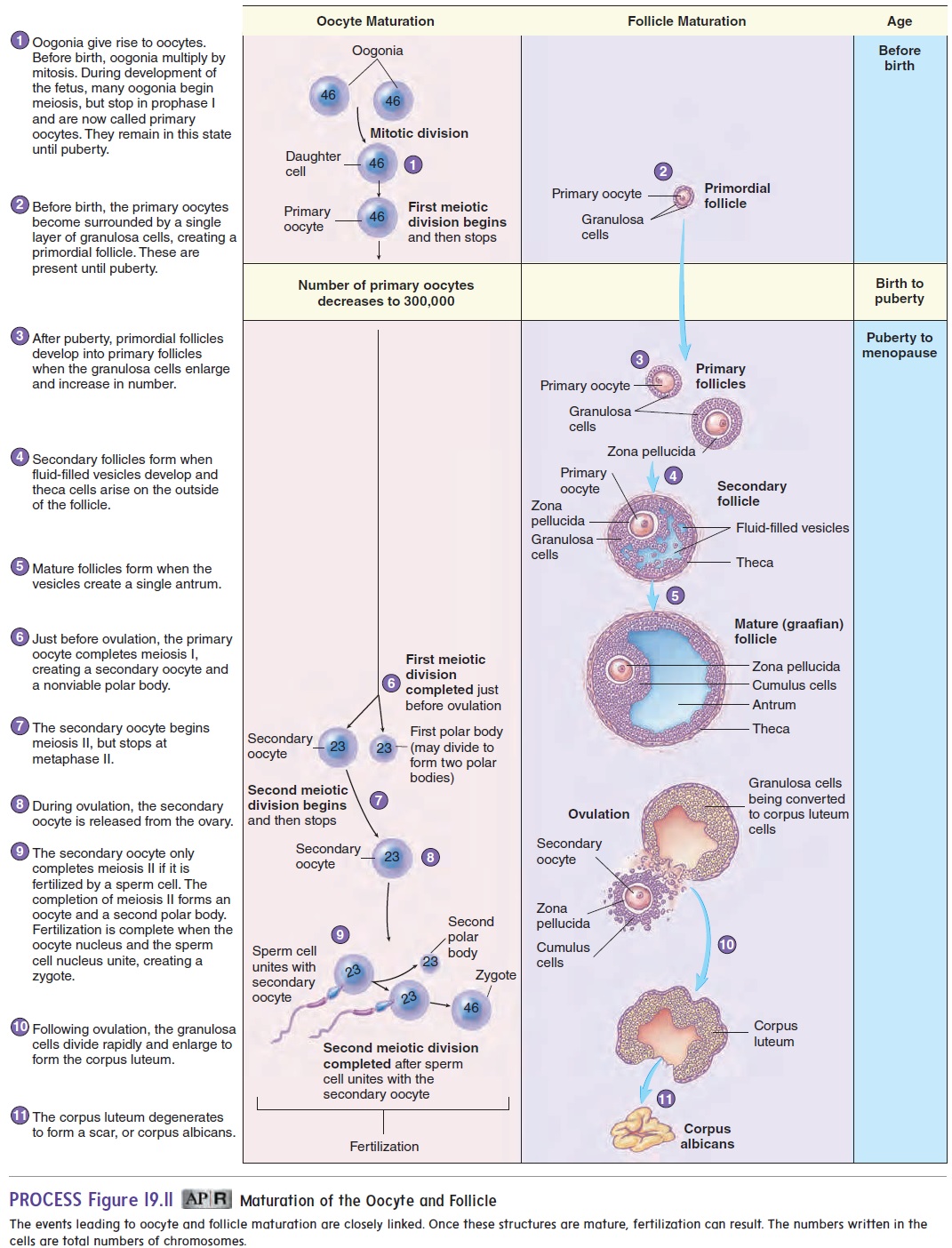
Ovulation is the release of an oocyte from an ovary (figure 19.11,step 8). Just before ovulation, the primary oocyte completes the first meiotic division to produce a secondary oocyte and a polar body.Unlike meiosis in males, cytoplasm is not split evenly between the two cells. Most of the cytoplasm of the primary oocyte remains with the secondary oocyte. The polar body either degenerates or divides to form two polar bodies. The secondary oocyte begins the second meiotic division but stops in metaphase II.
The zygote has 23 pairs of chromosomes (a total of 46 chromosomes). All cells of the human body contain 23 pairs of chromosomes, except for the male and female gametes. The zygote divides by mitosis to form 2 cells, which divide to form 4 cells, and so on. The mass of cells formed may eventually implant in, or attach to, the uterine wall and develop into a new individual .
Follicle Development
As we discussed, when a female is in her mother’s uterus, her ovaries have already begun oocyte formation. The primary oocytes present at birth are surrounded by a primordial follicle. A primordial follicleis a primary oocyte surrounded by a single layer of flat cells, called granulosa cells (figure 19.11). Once puberty begins, some of the pri-mordial follicles are converted to primary follicles when the oocyte enlarges and the single layer of granulosa cells becomes enlarged and cuboidal. Subsequently, several layers of granulosa cells form, and a layer of clear material called the zona pellucida (z̄o ′ n̆a pel-l̄u ′ sid-d̆a ) is deposited around the primary oocyte.
Approximately every 28 days, hormonal changes stimulate some of the primary follicles to continue to develop (figure 19.11). The primary follicle becomes a secondary follicle as fluid-filled spaces calledvesicles form among the granulosa cells, and a cap-sule called the theca (thē ′ kă ; a box) forms around the follicle.
The mature follicle forms a lump on the surface of the ovary. During ovulation, the mature follicle ruptures, forcing a small amount of blood, follicular fluid, and the secondary oocyte, surround-ed by the cumulus cells, into the peritoneal cavity. In most cases, only one of the follicles that begin to develop forms a mature follicle and undergoes ovulation. The other follicles degenerate. After ovu-lation, the remaining cells of the ruptured follicle are transformed into a glandular structure called the corpus luteum (k̄o r′ p̆u s, body; loo′ t̄e -̆u m, yellow). If pregnancy occurs, the corpus luteum enlarges in response to a hormone secreted by the placenta called humanchorionic gonadotropin hormone (hCG) (k̄o-r̄e-on′ik ḡo′nad-o-tr̄o ′ pin) (see table 19.1). If pregnancy does not occur, the corpus luteum lasts for 10–12 days and then begins to degenerate.
Uterine tubes
A uterine tube, also called a fallopian (fa-lō ′ pē -an) tube or oviductoviduct (ō ′ vi-d̆u ct), is associated with each ovary. The uterine tubes extend from the area of the ovaries to the uterus. They open directly into the peritoneal cavity near each ovary and receive the secondary oocyte. The opening of each uterine tube is surrounded by long, thin processes called fimbriae (fim′ brē -ē ; fringes) (see figure 19.9).
The fimbriae nearly surround the surface of the ovary. As a result, as soon as the secondary oocyte is ovulated, it comes into contact with the surface of the fimbriae. Cilia on the fimbriae surface sweep the oocyte into the uterine tube. Fertilization usu-ally occurs in the part of the uterine tube near the ovary, called the ampulla (am-pul′ l ă). The fertilized oocyte then travels to the uterus, where it embeds in the uterine wall in a process called implantation.
Uterus
The uterus (ū ′ ter-̆u s; womb) is as big as a medium-sized pear (see figures 19.8 and 19.9). It is oriented in the pelvic cavity with the larger, rounded part directed superiorly. The part of the uterus superior to the entrance of the uterine tubes is called the fundus (f̆u n′ d̆u s). The main part of the uterus is called the body, and the narrower part, the cervix (ser′ viks; neck), is directed inferiorly. Internally, the uterine cavity in the fundus and uterine body continues through the cervix as the cervical canal, which opens into the vagina. The cervical canal is lined by mucous glands.
The uterine wall is composed of three layers: a serous layer, a muscular layer, and a layer of endometrium (see figure 19.9). The outer layer, called the perimetrium (per-i-mē ′ trē -̆u m), or serouslayer, of the uterus is formed from visceral peritoneum. The mid-dle layer, called the myometrium (mı̄ ′ ō -mē ′ trē -̆u m), or muscularlayer, consists of smooth muscle, is quite thick, and accounts forthe bulk of the uterine wall. The innermost layer of the uterus is the endometrium (en′ dō -mē ′ trē -̆u m), which consists of simple columnar epithelial cells with an underlying connective tissue layer. Simple tubular glands, called spiral glands, are formed by folds of the endometrium. The superficial part of the endometrium is sloughed off during menstruation.
The uterus is supported by the broad ligament and the roundligament. In addition to these ligaments, much support is providedinferiorly to the uterus by skeletal muscles of the pelvic floor. If ligaments that support the uterus or muscles of the pelvic floor are weakened, as may occur due to childbirth, the uterus can extend inferiorly into the vagina, a condition called a prolapsed uterus. Severe cases require surgical correction.
Vagina
The vagina (vă-j ı̄′ nă) is the female organ of copulation; it receives the penis during intercourse. It also allows menstrual flow and childbirth. The vagina extends from the uterus to the outside of the body (see figures 19.8 and 19.9). The superior portion of the vagina is attached to the sides of the cervix, so that a part of the cervix extends into the vagina.
The wall of the vagina consists of an outer muscular layer and an inner mucous membrane. The muscular layer is smooth muscle and contains many elastic fibers. Thus, the vagina can increase in size to accommodate the penis during intercourse, and it can stretch greatly during childbirth. The mucous membrane is moist stratified squamous epithelium that forms a protective surface layer. Lubricating fluid passes through the vaginal epithelium into the vagina.
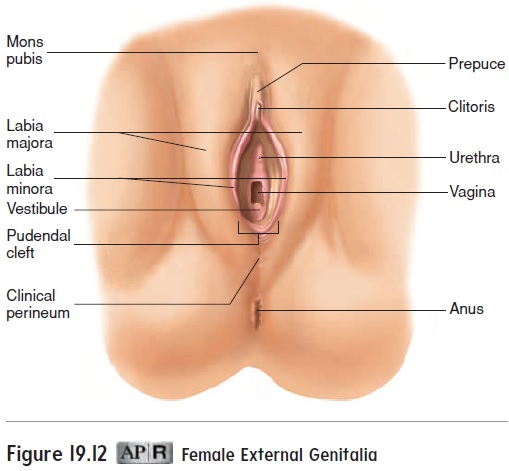
In young females, the vaginal opening is covered by a thin mucous membrane called the hymen (hı̄′ men; membrane). In rare cases, the hymen may completely close the vaginal orifice and it must be removed to allow menstrual flow. More commonly, the hymen is perforated by one or several holes. The openings in the hymen are usually greatly enlarged during the first sexual intercourse. The hymen can also be perforated or torn earlier in a young female’s life during a variety of activities, including strenu-ous exercise. The condition of the hymen is therefore an unreliable indicator of virginity.
The region between the vagina and the anus is the clinicalperineum (per′i-nē′um; area between the thighs). The skin andmuscle of this region can tear during childbirth. To prevent such tearing, an incision called an episiotomy (e-piz-ē-ot′ ō-mē) is sometimes made in the clinical perineum. Traditionally, this clean, straight incision has been thought to result in less injury, less trouble in healing, and less pain. However, many studies report less injury and pain when no episiotomy is performed.
Mammary Glands
The mammary (mam′ ă-rē; relating to breasts) glands are the organs of milk production and are located in the breasts (fig-ure 19.13). The mammary glands are modified sweat glands. Externally, each of the breasts of both males and females has a raised nipple surrounded by a circular, pigmented area called the areola (ă-rē′ō-lă).
In prepubescent children, the general structure of the male and female breasts is similar, and both males and females possess a rudimentary duct system. The female breasts begin to enlarge during puberty, under the influence of estrogen and progesterone. Some males also experience a minor and temporary enlargement of the breasts at puberty. Occasionally, the breasts of a male can become permanently enlarged, a condition called gynecomastia (gı̄′ nĕ-kō-mas′ t ē-ă). Causes of gynecomastia include hormonal imbalances and the abuse of anabolic steroids.
Each adult female breast contains mammary glands con-sisting of usually 15–20 glandular lobes covered by adipose tissue (figure 19.13a,b). It is primarily this superficial adipose tissue that gives the breast its form. Each lobe possesses a single lactiferous duct that opens independently to the surface of the
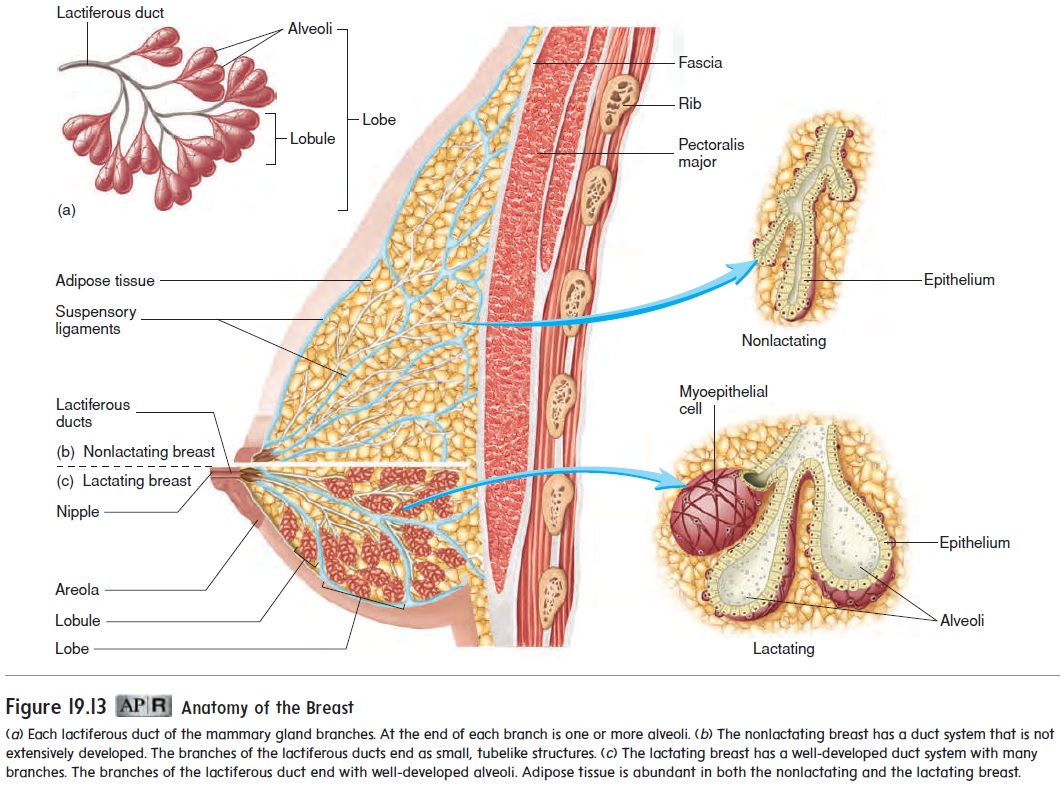
nipple. The duct of each lobe is formed as several smaller ducts, which originate from lobules, converge. Within a lobule, the ducts branch and become even smaller. In the milk-producing, or lactating, mammary gland, the ends of these small ducts expand to form secretory sacs called alveoli. Myoepithelial cells sur-round the alveoli and contract to expel milk from the alveoli (figure 19.13c).
The breasts are supported by suspensory ligaments that extend from the fascia over the pectoralis major muscles to the skin over the breasts (figure 19.13b).
The nipples are very sensitive to tactile stimulation and contain smooth muscle. When the smooth muscle contracts in response to stimuli, such as touch, cold, and sexual arousal, the nipple becomes erect.
Related Topics