Chapter: Medical Physiology: Renal Regulation of Potassium, Calcium, Phosphate, and Magnesium; Integration of Renal Mechanisms for Control of Blood Volume and Extracellular Fluid Volume
Control of Renal Calcium Excretion and Extracellular Calcium Ion Concentration
Control of Renal Calcium Excretion and Extracellular Calcium Ion Concentration
The mechanisms for regulating calcium ion concentration are discussed in detail, along with the endocrinology of the calcium-regulating hormones parathyroid hormone (PTH) and calcitonin.
Extracellular fluid calcium ion concentration normally remains tightly controlled within a few percentage points of its normal level, 2.4 mEq/L. When calcium ion concentration falls to low levels (hypocalcemia), the excitability of nerve and muscle cells increases markedly and can in extreme cases result in hypocalcemic tetany. This is characterized by spastic skeletal muscle contractions.Hypercalcemia (increased calcium concentration) depresses neuromus-cular excitability and can lead to cardiac arrhythmias.
About 50 per cent of the total calcium in the plasma (5 mEq/L) exists in the ionized form, which is the form that has biological activity at cell membranes. The remainder is either bound to the plasma proteins (about 40 per cent) or complexed in the non-ionized form with anions such as phosphate and citrate (about 10 per cent).
Changes in plasma hydrogen ion concentration can influence the degree of calcium binding to plasma pro-teins. With acidosis, less calcium is bound to the plasma proteins. Conversely, in alkalosis, a greater amount of calcium is bound to the plasma proteins. Therefore, patients with alkalosis are more susceptible to hypocal-cemic tetany.
As with other substances in the body, the intake of calcium must be balanced with the net loss of calcium over the long term. Unlike ions such as sodium and chloride, however, a large share of calcium excretion occurs in the feces. The usual rate of dietary calcium intake is about 1000 mg/day, with about 900 mg/day of calcium excreted in the feces. Under certain condi-tions, fecal calcium excretion can exceed calcium ingestion because calcium can also be secreted into the intestinal lumen. Therefore, the gastrointestinal tract and the regulatory mechanisms that influence intestinal calcium absorption and secretion play a major role in calcium homeostasis.
Almost all the calcium in the body (99 per cent) is stored in the bone, with only about 1 per cent in the extracellular fluid and 0.1 per cent in the intracellular fluid. The bone, therefore, acts as a large reservoir for storing calcium and as a source of calcium when extracellular fluid calcium concentration tends to decrease.
One of the most important regulators of bone uptake and release of calcium is PTH. When extracellular fluid calcium concentration falls below normal, the parathy-roid glands are directly stimulated by the low calcium levels to promote increased secretion of PTH. This hormone then acts directly on the bones to increase the resorption of bone salts (release of salts from the bones) and, therefore, to release large amounts of calcium into the extracellular fluid, thereby returning calcium levels back toward normal. When calcium ion concentration is elevated, PTH secretion decreases, so that almost no bone resorption now occurs; instead, excess calcium is deposited in the bones because of new bone formation. Thus, the day-to-day regulation of calcium ion concentration is mediated in large part by the effect of PTH on bone resorption.
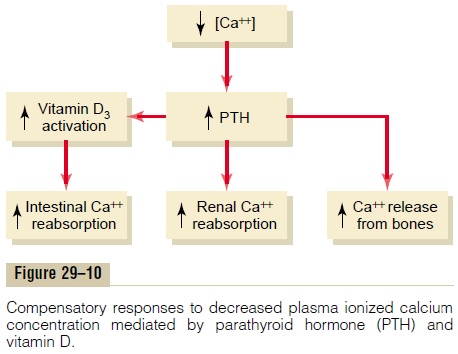
The bones, however, do not have an inexhaustible supply of calcium. Therefore, over the long term, the intake of calcium must be balanced with calcium excretion by the gastrointestinal tract and the kidneys. The most important regulator of calcium reabsorption at both of these sites is PTH. Thus, PTH regulatesplasma calcium concentration through three main effects: (1) by stimulating bone resorption; (2) by stim-ulating activation of vitamin D, which then increases intestinal reabsorption of calcium; and (3) by directly increasing renal tubular calcium reabsorption (Figure29–10). The control of gastrointestinal calcium reab-sorption and calcium exchange in the bones is dis-cussed elsewhere, and the remainder of this section focuses on the mechanisms that control renal calcium excretion.
Control of Calcium Excretion by the Kidneys
Because calcium is both filtered and reabsorbed in the kidneys but not secreted, the rate of renal calcium excretion is calculated as
Renal calcium excretion = Calcium filtered - Calcium reabsorbed
Only about 50 per cent of the plasma calcium is ionized, with the remainder being bound to the plasma proteins or complexed with anions such as phosphate. Therefore, only about 50 per cent of the plasma calcium can be filtered at the glomerulus. Normally, about 99 per cent of the filtered calcium is reabsorbed by the tubules, with only about 1 per cent of the fil-tered calcium being excreted. About 65 per cent of the filtered calcium is reabsorbed in the proximal tubule, 25 to 30 per cent is reabsorbed in the loop of Henle, and 4 to 9 per cent is reabsorbed in the distal and col-lecting tubules. This pattern of reabsorption is similar to that for sodium.
As is true with the other ions, calcium excretion is adjusted to meet the body’s needs. With an increase in calcium intake, there is also increased renal calcium excretion, although much of the increase of calcium intake is eliminated in the feces. With calcium deple-tion, calcium excretion by the kidneys decreases as a result of enhanced tubular reabsorption.
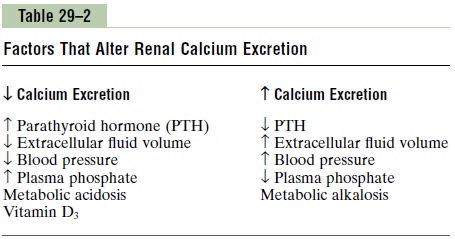
One of the primary controllers of renal tubular calcium reabsorption is PTH. With increased levels of PTH, there is increased calcium reabsorption in the thick ascending loops of Henle and distal tubules, which reduces urinary excretion of calcium. Con-versely, reduction of PTH promotes calcium excretion by decreasing reabsorption in the loops of Henle and distal tubules.
In the proximal tubule, calcium reabsorption usually parallels sodium and water reabsorption. Therefore, in instances of extracellular volume expansion or increased arterial pressure—both of which decrease proximal sodium and water reabsorption—there is also reduction in calcium reabsorption and, con-sequently, increased urinary excretion of calcium. Conversely, with extracellular volume contraction or decreased blood pressure, calcium excretion decreases primarily because of increased proximal tubular reabsorption.
Another factor that influences calcium reabsorption is the plasma concentration of phosphate. An increase in plasma phosphate stimulates PTH, which increases calcium reabsorption by the renal tubules, thereby reducing calcium excretion. The opposite occurs with reduction in plasma phosphate concentration.
Calcium reabsorption is also stimulated by meta-bolic acidosis and inhibited by metabolic alkalosis. Most of the effect of hydrogen ion concentration on calcium excretion results from changes in calcium reabsorption in the distal tubule.
A summary of the factors that are known to influence calcium excretion by the renal tubules is shown in Table 29–2.
Regulation of Renal Phosphate Excretion
Phosphate excretion by the kidneys is controlled primarily by an overflow mechanism that can be explained as follows: The renal tubules have a normal transport maximum for reabsorbing phosphate of about 0.1 mM/min. When less than this amount of phosphate is present in the glomerular filtrate, essentially all the filtered phosphate is reabsorbed.
When more than this is present, the excess is excreted. Therefore, phosphate normally begins to spill into the urine when its concentration in the extracellular fluid rises above a threshold of about 0.8 mM/L, which gives a tubular load of phosphate of about 0.1 mM/min, assuming a GFR of 125 ml/min. Because most people ingest large quantities of phosphate in milk products and meat, the concentration of phosphate is usually maintained above 1 mM/L, a level at which there is continual excretion of phosphate into the urine.
Changes in tubular phosphate reabsorption can also influence phosphate excretion. For instance, a diet low in phosphate can, over time, increase the reabsorptive transport maximum for phosphate, thereby reducing the tendency for phosphate to spill over into the urine.
PTH can play a significant role in regulating phos-phate concentration through two effects: (1) PTH promotes bone resorption, thereby dumping large amounts of phosphate ions into the extracellular fluid from the bone salts, and (2) PTH decreases the trans-port maximum for phosphate by the renal tubules, so that a greater proportion of the tubular phosphate is lost in the urine. Thus, whenever plasma PTH isincreased, tubular phosphate reabsorption is decreased and more phosphate is excreted.
Related Topics