Chapter: Medical Surgical Nursing: Assessment of Cardiovascular Function
Assessment of Cardiovascular Function: Physical Assessment
PHYSICAL ASSESSMENT
A
physical examination is performed to confirm the data obtained in the health
history. In addition to observing the patient’s gen-eral appearance, a cardiac
physical examination should include an evaluation of the following:
·
Effectiveness of the heart as a pump
·
Filling volumes and pressures
·
Cardiac output
·
Compensatory mechanisms
Indications
that the heart is not contracting sufficiently or functioning effectively as a
pump include reduced pulse pressure, cardiac enlargement, and murmurs and
gallop rhythms (abnor-mal heart sounds).
The
amount of blood filling the atria and ventricles and the re-sulting pressures
(called filling volumes and pressures) are esti-mated by the degree of jugular
vein distention and the presence or absence of congestion in the lungs,
peripheral edema, and postural changes in BP that occur when the individual
sits up or stands.
Cardiac
output is reflected by cognition, heart rate, pulse pres-sure, color and
texture of the skin, and urine output. Examples of compensatory mechanisms that
help maintain cardiac output are increased filling volumes and elevated heart
rate. Note that the findings on the physical examination are correlated with
data ob-tained from diagnostic procedures, such as hemodynamic moni-toring
(discussed later).
The
examination, which proceeds logically from head to toe, can be performed in
about 10 minutes with practice and covers the following areas: (1) general
appearance, (2) cognition, (3) skin, BP, (5) arterial pulses, (6) jugular
venous pulsations and pressures, (7) heart, (8) extremities, (9) lungs, and
(10) abdomen
General Appearance and Cognition
The
nurse observes the patient’s level of distress, level of conscious-ness, and
thought processes as an indication of the heart’s ability to propel oxygen to
the brain (cerebral perfusion). The nurse also observes for evidence of
anxiety, along with any effects emotional factors may have on cardiovascular
status. The nurse attempts to put the anxious patient at ease throughout the
examination.
Inspection of the Skin
Examination
of the skin begins during the evaluation of the gen-eral appearance of the
patient and continues throughout the as-sessment. It includes all body
surfaces, starting with the head and finishing with the lower extremities. Skin
color, temperature, and texture are assessed. The more common findings associated
with cardiovascular disease are as follows.
·
Pallor—a decrease in the color of
the skin—is caused by lack of oxyhemoglobin. It is a result of anemia or
decreased arterial perfusion. Pallor is best observed around the finger-nails,
lips, and oral mucosa. In patients with dark skin, the nurse observes the palms
of the hands and soles of the feet.
·
Peripheral cyanosis—a bluish tinge,
most often of the nails and skin of the nose, lips, earlobes, and
extremities—suggests decreased flow rate of blood to a particular area, which
allows more time for the hemoglobin molecule to become desatu-rated. This may
occur normally in peripheral vasoconstric-tion associated with a cold
environment, in patients with anxiety, or in disease states such as HF.
·
Central cyanosis—a bluish tinge
observed in the tongue and buccal mucosa—denotes serious cardiac disorders
(pulmonary edema and congenital heart disease) in which venous blood passes
through the pulmonary circulation without being oxygenated.
·
Xanthelasma—yellowish, slightly
raised plaques in the skin—may be observed along the nasal portion of one or
both eyelids and may indicate elevated cholesterol levels
(hypercholesterolemia).
·
Reduced skin turgor occurs with
dehydration and aging.
·
Temperature and moistness are controlled
by the auto-nomic nervous system. Normally the skin is warm and dry. Under
stress, the hands may become cool and moist. In car-diogenic shock, sympathetic
nervous system stimulation causes vasoconstriction, and the skin becomes cold
and clammy. During an acute MI, diaphoresis is common.
·
Ecchymosis (bruise)—a purplish-blue
color fading to green, yellow, or brown over time—is associated with blood
out-side of the blood vessels and is usually caused by trauma. Pa-tients who
are receiving anticoagulant therapy should be carefully observed for
unexplained ecchymosis. In these pa-tients, excessive bruising indicates
prolonged clotting times (prothrombin or partial thromboplastin time) caused by
an anticoagulant dosage that is too high.
·
Wounds, scars, and tissue
surrounding implanted devices should also be examined. Wounds are assessed for
adequate healing, and any scars from previous surgeries are noted. The skin
surrounding a pacemaker or implantable cardio-verter defibrillator generator is
examined for thinning, which could indicate erosion of the device through the
skin.
Blood Pressure
Systemic
arterial BP is the pressure exerted on the walls of the ar-teries during
ventricular systole and diastole. It is affected by fac-tors such as cardiac
output, distention of the arteries, and the volume, velocity, and viscosity of
the blood. BP usually is expressed as the ratio of the systolic pressure over
the diastolic pressure, with normal adult values ranging from 100/60 to 140/90
mm Hg. The average normal BP usually cited is 120/80 mm Hg. An in-crease in BP
above the upper normal range is called hypertension, whereas a decrease below
the lower range is called hypotension.
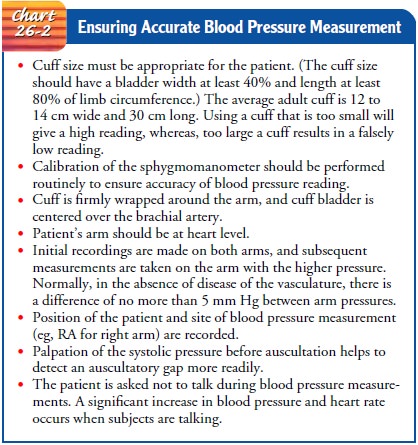
BLOOD PRESSURE MEASUREMENT
BP
can be measured with the use of invasive arterial monitoring systems (discussed
later) or noninvasively by a sphygmomanometer and stethoscope or by an
automated BP monitoring device. A de-tailed description of the procedure for
obtaining BP can be found in nursing skills textbooks, and specific
manufacturer’s instruc-tions review the proper use of the automated monitoring
devices. Several important details must be observed to ensure that BP
measurements are accurate; these are highlighted in Chart 26-2.
PULSE PRESSURE
The difference between the systolic and the diastolic pressures is called the pulse pressure. It is a reflection of stroke volume, ejection velocity, and systemic vascular resistance. Pulse pressure, which normally is 30 to 40 mm Hg, indicates how well the patient main-tains cardiac output. The pulse pressure increases in conditions that elevate the stroke volume (anxiety, exercise, bradycardia), reduce systemic vascular resistance (fever), or reduce distensibility of the arteries (atherosclerosis, aging, hypertension). Decreased pulse pres-sure is an abnormal condition reflecting reduced stroke volume and ejection velocity (shock, HF, hypovolemia, mitral regurgitation) or obstruction to blood flow during systole (mitral or aorticstenosis). A pulse pressure of less than 30 mm Hg signifies a serious reduction in cardiac output and requires further cardiovascular assessment.
POSTURAL BLOOD PRESSURE CHANGES
Postural (orthostatic) hypotension occurs
when the BP dropssignificantly after the patient assumes an upright posture. It
is usually accompanied by dizziness, lightheadedness, or syncope.
Although
there are many causes of postural hypotension, the three most common causes in
patients with cardiac problems are a reduced volume of fluid or blood in the
circulatory system (intra-vascular volume depletion, dehydration), inadequate
vasocon-strictor mechanisms, and insufficient autonomic effect on vascular
constriction. Postural changes in BP and an appropriate history help health
care providers differentiate among these causes. The following recommendations
are important when assessing pos-tural BP changes:
·
Position the patient supine and flat
(as symptoms permit) for 10 minutes before taking the initial BP and heart rate
measurements.
·
Check supine measurements before
checking upright mea-surements.
·
Do not remove the BP cuff between
position changes, but check to see that it is still correctly placed.
·
Assess postural BP changes with the
patient sitting on the edge of the bed with feet dangling and, if appropriate, with
the patient standing at the side of the bed.
·
Wait 1 to 3 minutes after each
postural change before mea-suring BP and heart rate.
·
Be alert for any signs or symptoms
of patient distress. If nec-essary, return the patient to a lying position
before com-pleting the test.
·
Record both heart rate and BP and
indicate the correspond-ing position (e.g., lying, sitting, standing) and any
signs or symptoms that accompany the postural change.
Normal
postural responses that occur when a person stands up or goes from a lying to a
sitting position include (1) a heart rate increase of 5 to 20 bpm above the
resting rate (to offset reduced stroke volume and maintain cardiac output); (2)
an unchanged systolic pressure, or a slight decrease of up to 10 mm Hg; and (3)
a slight increase of 5 mm Hg in diastolic pressure.
A
decrease in the amount of blood or fluid in the circulatory system should be
suspected after diuretic therapy or bleeding, when a postural change results in
an increased heart rate and either a decrease in systolic pressure by 15 mm Hg
or a drop in the diastolic pressure by 10 mm Hg. Vital signs alone do not
dif-ferentiate between a decrease in intravascular volume and in-adequate
constriction of the blood vessels as a cause of postural hypotension. With intravascular
volume depletion, the reflexes that maintain cardiac output (increased heart
rate and peripheral vasoconstriction) function correctly; the heart rate
increases, and the peripheral vessels constrict. However, because of lost
vol-ume, the BP falls. With inadequate vasoconstrictor mechanisms, the heart
rate again responds appropriately, but because of di-minished peripheral
vasoconstriction the BP drops. The follow-ing is an example of a postural BP
recording showing either intravascular volume depletion or inadequate
vasoconstrictor mechanisms:
Lying
down, BP 120/70, heart rate 70
Sitting,
BP 100/55, heart rate 90
Standing,
BP 98/52, heart rate 94
In
autonomic insufficiency, the heart rate is unable to increase to completely
compensate for the gravitational effects of an up-right posture. Peripheral
vasoconstriction may be absent or di-minished. Autonomic insufficiency does not
rule out a concurrent decrease in intravascular volume. The following is an
example of autonomic insufficiency as demonstrated by postural BP changes:
Lying
down, BP 150/90, heart rate 60
Sitting,
BP 100/60, heart rate 60
Arterial Pulses
Factors
to be evaluated in examining the pulse are rate, rhythm, quality, configuration
of the pulse wave, and quality of the arte-rial vessel.
PULSE RATE
The
normal pulse rate varies from a low of 50 bpm in healthy, athletic young adults
to rates well in excess of 100 bpm after ex-ercise or during times of
excitement. Anxiety frequently raises the pulse rate during the physical examination.
If the rate is higher than expected, it is appropriate to reassess it near the
end of the physical examination, when the patient may be more relaxed.
PULSE RHYTHM
The
rhythm of the pulse is as important to assess as the rate. Minor variations in regularity
of the pulse are normal. The pulse rate, particularly in young people,
increases during inhalation and slows during exhalation. This is called sinus
arrhythmia.
For
the initial cardiac examination, or if the pulse rhythm is irregular, the heart
rate should be counted by auscultating the apical pulse for a full minute while
simultaneously palpating the radial pulse.
Any
discrepancy between contractions heard and pulses felt is noted. Disturbances
of rhythm (dysrhythmias) often result in a pulse deficit, a difference between
the apical rate (the heart rate heard at the apex of the heart) and the
peripheral rate. Pulse deficits commonly occur with atrial fibrillation, atrial
flutter, premature ventricular contractions, and varying degrees of heart block.
To
understand the complexity of dysrhythmias that may be encountered during the
examination, the nurse needs to have a sophisticated knowledge of cardiac
electrophysiology, obtained through advanced education and training.
PULSE QUALITY
The
quality, or amplitude, of the pulse can be described as absent, diminished,
normal, or bounding. It should be assessed bilater-ally. Scales can be used to
rate the strength of the pulse. The fol-lowing is an example of a 0-to-4 scale:
0
pulse not palpable or absent
+1 weak, thready pulse; difficult to palpate;
obliterated with pressure
+2 diminished pulse; cannot be obliterated
+3 easy to palpate, full pulse; cannot be
obliterated
+4 strong, bounding pulse; may be abnormal
The
numerical classification is quite subjective; therefore, when documenting the
pulse quality, it helps to specify a scale range (eg, “left radial +3/+4”).
PULSE CONFIGURATION
The
configuration (contour) of the pulse conveys important in-formation. In
patients with stenosis of the aortic valve, the valve opening is narrowed,
reducing the amount of blood ejected into the aorta. The pulse pressure is
narrow, and the pulse feels feeble. In aortic insufficiency, the aortic valve
does not close completely, allowing blood to flow back or leak from the aorta
into the left ventricle. The rise of the pulse wave is abrupt and strong, and
its fall is precipitous—a “collapsing” or “water hammer” pulse. The true
configuration of the pulse is best appreciated by palpating over the carotid
artery rather than the distal radial artery, because the dramatic
characteristics of the pulse wave may be distorted when the pulse is
transmitted to smaller vessels.
EFFECT OF VESSEL QUALITY ON PULSE
The
condition of the vessel wall also influences the pulse and is of concern,
especially in older patients. Once rate and rhythm have been determined, the
nurse assesses the quality of the vessel by palpating along the radial artery
and comparing it with nor-mal vessels. Does the vessel wall appear to be
thickened? Is it tortuous?
To assess peripheral circulation, the
nurse locates and evalu-ates all arterial pulses. Arterial pulses are palpated
at points where the arteries are near the skin surface and are easily
compressed against bones or firm musculature. Pulses are detected over the
temporal, carotid, brachial, radial, femoral, popliteal, dorsalis pedis, and
posterior tibial arteries. A reliable assessment of the pulses of the lower
extremities depends on accurate identification of the location of the artery
and careful palpation of the area. Light palpation is essential; firm finger
pressure can easily oblit-erate the dorsalis pedis and posterior tibial pulses
and confuse the examiner. In approximately 10% of patients, the dorsalis pedis
pulses are not palpable. In such circumstances, both are usu-ally absent
together, and the posterior tibial arteries alone pro-vide adequate blood
supply to the feet. Arteries in the extremities are often palpated
simultaneously to facilitate comparison of quality.
Jugular Venous Pulsations
An
estimate of right-sided heart function can be made by observ-ing the pulsations
of the jugular veins of the neck. This provides a means of estimating central
venous pressure, which reflects right atrial or right ventricular end-diastolic
pressure (the pressure immediately preceding the contraction of the right
ventricle).
Pulsations
of the internal jugular veins are most commonly as-sessed. If they are
difficult to see, pulsations of the external jugu-lar veins may be noted. These
veins are more superficial and are visible just above the clavicles, adjacent
to the sternocleido-mastoid muscles. The external jugular veins are frequently
dis-tended while the patient lies supine on the examining table or bed. As the
patient’s head is elevated, the distention of the veins disappears. The veins
normally are not apparent if the head of the bed or examining table is elevated
more than 30 degrees.
Obvious
distention of the veins with the patient’s head elevated 45 degrees to 90
degrees indicates an abnormal increase in the vol-ume of the venous system.
This is associated with right-sided HF, less commonly with obstruction of blood
flow in the superior vena cava, and rarely with acute massive pulmonary
embolism.
Heart Inspection and Palpation
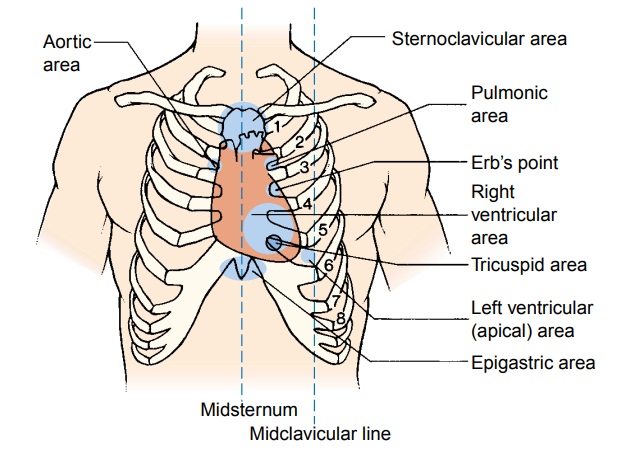
The
heart is examined indirectly by inspection, palpation, per-cussion, and
auscultation of the chest wall. A systematic approach is the cornerstone of a
thorough assessment. Examination of the chest wall is performed in the
following six areas (Fig. 26-6):
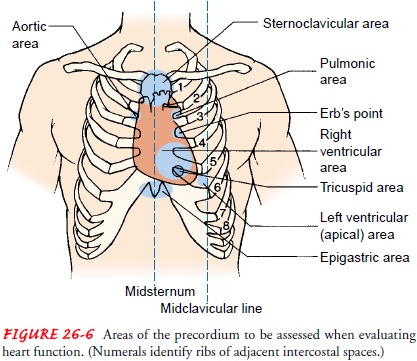
·
Aortic
area—second intercostal space to the right of thesternum. To
determine the correct intercostal space, start at the angle of Louis by
locating the bony ridge near the top of the sternum, at the junction of the
body and the manu-brium. From this angle, locate the second intercostal space
by sliding one finger to the left or right of the sternum. Subsequent
intercostal spaces are located from this refer-ence point by palpating down the
rib cage.
·
Pulmonic
area—second intercostal space to the left of thesternum
·
Erb’s
point—third intercostal space to the left of the sternum
·
Right
ventricular or tricuspid area—fourth and fifth inter-costal
spaces to the left of the sternum
·
Left
ventricular or apical area—the PMI, location on thechest where
heart contractions can be palpated
·
Epigastric
area—below the xiphoid process
For
most of the examination, the patient lies supine, with the head slightly
elevated. The right-handed examiner is positioned at the right side of the
patient and the left-handed examiner at the left side.
In
a systematic fashion, each area of the precordium is inspected and then
palpated. Oblique lighting is used to assist the examiner in identifying subtle
pulsation. A normal impulse that is distinct and located over the apex of the
heart is called the apical impulse
(PMI). It may be observed in young people and in older people who are thin. The
apical impulse is normally located and auscul-tated in the left fifth
intercostal space in the midclavicular line (Fig. 26-7).
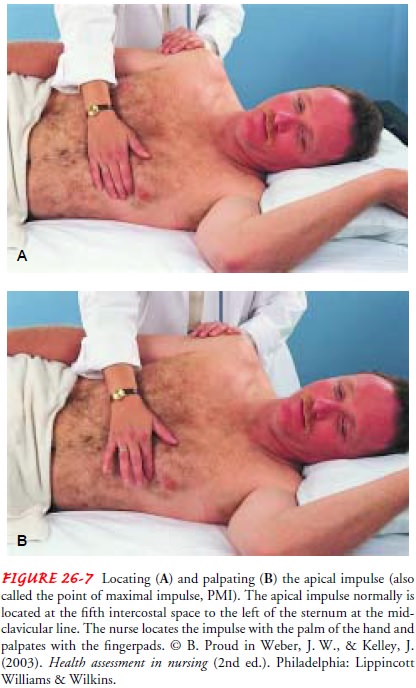
In many cases, the apical impulse is palpable and is normally felt as a light pulsation, 1 to 2 cm in diameter. It is felt at the onset of the first heart sound and lasts for only half of systole. (See the next section for a discussion of heart sounds.) The nurse uses the palm of the hand to locate the apical impulse initially and the fingerpads to assess its size and quality. A broad and forceful apical impulse is known as a left ventricular heave or lift. It is so named because it appears to lift the hand from the chest wall during palpation.
An
apical impulse below the fifth intercostal space or lateral to the
midclavicular line usually denotes left ventricular enlarge-ment from left
ventricular failure. Normally, the apical impulse is palpable in only one
intercostal space; palpability in two or more adjacent intercostal spaces
indicates left ventricular enlargement. If the apical impulse can be palpated
in two distinctly separate areas and the pulsation movements are paradoxical
(not simulta-neous), a ventricular aneurysm should be suspected.
Abnormal,
turbulent blood flow within the heart may be pal-pated with the palm of the
hand as a purring sensation. This phe-nomenon is called a thrill and is
associated with a loud murmur. A thrill is always indicative of significant
pathology within the heart. Thrills also may be palpated over vessels when
blood flow is significantly and substantially obstructed and over the carotid
ar-teries if aortic stenosis is present or if the aortic valve is narrowed.
Chest Percussion
Normally,
only the left border of the heart can be detected by percussion. It extends
from the sternum to the midclavicular line in the third to fifth intercostal
spaces. The right border lies under the right margin of the sternum and is not
detectable. Enlarge-ment of the heart to either the left or right usually can
be noted. In people with thick chests, obesity, or emphysema, the heart may lie
so deep under the thoracic surface that not even its left border can be noted
unless the heart is enlarged. In such cases, unless the nurse detects a
displaced apical impulse and suspects cardiac en-largement, percussion is
omitted.
Related Topics