Chapter: Medicine Study Notes : Infectious Diseases
Vaccination
Vaccination
Vaccination Principles
·
Jenner first vaccinated using
cowpox against smallpox in 1796
·
Characteristics of immunity:
o Specificity: response to specific antigen
o Priming
o Memory: brisk secondary response
·
Results of vaccine:
o Most stimulate serum antibodies (IgG, IgM)
o Some stimulate IgA (eg polio, rubella)
o A few promote cell mediated reaction (eg BCG)
· Types of vaccine:
o Live attenuated vaccine (eg OPV, MMR, VZ, BCG): full and long lasting
immunity after a single dose (except OPV which requires 3 doses)
o Inactivated vaccines:
§ First dose gives a predominantly IgM response. Further doses raise IgG level (depending on potency of the vaccine, maturity of the immune system and time interval)
§ Inactivated whole bacteria or viral vaccines: IPV, Hep A, Whole cell pertussis (being replaced).
§ Modified toxins (toxoids) eg Diphtheria, Tetanus ® antibody response to toxin not infective agent
§ Sub-unit vaccines: eg Hep B, HIB, Pneumococcus, Influenza – the main focus of modern vaccines – conjugated vaccines with fewer side effects and easy to grow from genetically engineered yeasts etc.
o Also passive immunity available from injectable IgG. Immediate
protection lasting from weeks to months
·
Population protection:
o Immunisation is delivered to individuals and provides individual
protection and benefit
o Also provides population protection (herd immunity):
§ Some level of immunisation protects unimmunised people who would
otherwise have caught it Þ don‟t need to immunise those for whom its contraindicated (eg too young
or sick)
§ Virulence Þ coverage necessary to get herd immunity
§ „Free riders‟ – because they perceive costs (needles, hassle, side
effects) to be greater than perceived benefits ® weakens
herd immunity
· Efficacy and effectiveness:
o Efficacy: Does intervention provide a specific outcome (eg an IgG response) under ideal lab circumstances
o Effectiveness: Does it work under normal clinical circumstances
o Apparent paradox: as coverage , so does the proportion of cases that have been vaccinated (but lower absolute numbers of disease), due to vaccination failure. Can create the illusion that the vaccine is ineffective
· Vaccine failure:
o Primary vaccine failure: inadequate physiological response to the vaccine (eg freezing or overheating of the vaccine, or poor host response)
o Secondary vaccine failure: waning immunity
·
Degrees of protection:
o Generally provides 80 – 95% protection (BCG 50%, Influenza 70%)
o May protect against severe disease rather than infection (eg Diphtheria)
·
Vaccination coverage:
o = Proportion of a population who have completed a specific course of
immunisation
o In Northern Region in 1996, 63% by 2 years but only 45% for Maori and 53% for Pacific islanders
o With measles: coverage ® time between epidemics as need a pool of 130 – 150,000 measles susceptible children to sustain an epidemic. Each epidemic ® 50,000 kids contract measles and therefore immune in future. 10,000 unprotected kids added to the pool each year.
o Policy measures: revise schedule to reduce the number of visits,
immunisation certificates on enrolment at school/early childhood centre.
· Surveillance: Generally poor systems
o Disease surveillance: notifications, discharge and mortality database,
outbreak investigations, disease modelling
·
Coverage surveillance: registers
and periodic surveys
·
Adverse event surveillance
·
Cold-chain monitoring
Vaccination Practice
· Practical vaccination standards:
o Ensure correct storage and transport: maintain the „cold chain‟ at 2 – 8 C. Eg have dedicated fridge and check its minimum and maximum temperature daily
o Check vaccines due for each patient: either age groups (neonates, children, adolescents, adults, elderly) or specific exposure situations (occupational, travel, post-exposure)
o Discuss and obtain informed consent: Written consent only required for
children if care giver not present
o Check contra-indications
o Administer vaccine
o Manage adverse reactions:
§ Observe for 20 minutes afterwards
§ Local or systemic reactions (fever, rash, joint pains): symptoms of immune activation. Offer Paracetamol. Especially whole cell pertussis. MMR may be followed about 7 – 10 days later by a 2 – 3 day fever and rash (but the vaccine is not infectious)
§ Anaphylaxis: Distinguish from fainting (which is common). Treatment:
ABC, Adrenaline
§ 1:1000 IM injection, 0.01 ml/kg, O2
§ Report to centre for Adverse Reaction Monitoring if serious (includes
persistent screaming > 3 hours and > 5 cm swelling at injection site),
but also convulsions, meningitis within 30 days
o Manage records: practice notes, HBL claim record and immunisation
certificate for parents
·
Anti-immunisation views:
o Risks outweigh benefits: some diseases now rare and specific vaccines have serious side effects
o Alternative health views: disease part of growing up (so was death!) and
natural infection develops immune system
o Plus a variety of beliefs/values that will be hard to shift
o Main reasons for non-immunisation is „passive rejecters‟ – don‟t get
around to it
·
Contraindications:
o Acute illness or fever > 38 C: defer vaccine. Otherwise will blame the illness on the
vaccine!
o Living with an immune suppressed person: use IPV rather than OPV
o Reaction to previous dose: encephalopathy with 7 days of DTP vaccines or immediate severe allergic reaction. If true anaphylaxis seek specialist advice
o Immune suppression: don‟t give live vaccine. Likely to have reduced response to inactivated vaccines
o Pregnancy: theoretical risk from live virus vaccines
o If in doubt, refer to a paediatrician
·
False contraindications:
o Mild illness, URTI, fever < 38.5 C
o Asthma, hay fever, eczema
o Prematurity and low birth weight in an otherwise healthy child – these especially need vaccination
o Previous clinical history of illness: no harm done from vaccinating and
many clinically diagnosed cases of an illness are in fact something else
o On antibiotics, inhaled or low dose steroids
o Stable neurological conditions (cerebral palsy, Down)
Currently Vaccine Schedule
·
Current Vaccination Schedule from
February 2002:
o Covers Hep B, Diphtheria (child dose = D, adult dose = d – smaller),
Tetanus, acellular Pertussis, Polio (now all intravenous = IPV, not oral), Hib,
Measles, Mumps, Rubella
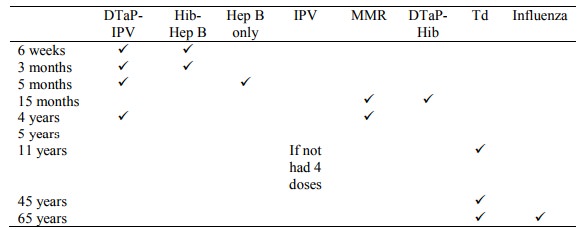
o For unimmunised adults:
§ Give jabs over same timeframe
§ Don‟t need HIB, don‟t give paediatric dose of diphtheria (too big) and
more inclined to use
§ IPV
·
Additional vaccination in
specific age groups:
o Neonates:
§ Babies of HBsAg +ive mothers: Hepatitis B immune globulin (HBIG) and vaccine at birth, vaccine at 6 weeks, 3 months and 5 months. Also offer vaccination to household and sexual contacts.
§ BCG if possible Tb exposure
o Women of child bearing age who are susceptible to Rubella should be
offered MMR
o Adults: Td (after injury and at 45 and 65 – used to be 10 yearly) +
annual influenza
o Elderly: annual influenza + pneumococcal (5 yearly)
·
Specific exposure situations:
o Splenectomy: Pneumococcal vaccine
o Occupational: Health care workers
(eg Hep B) or HAV to food workers
o Travel: See Topic: Travel Medicine
·
Future Developments:
o Inclusion of Varicella Zoster and pneumococcal for children
o Research into Group B meningococcal (currently 10 year epidemic, 250
cases per year), Rotavirus and RSV, non-infectious diseases including cancer
Vaccine Preventable Diseases
·
Measles and Pertussis are the
main ones still happening that we shouldn‟t have
· Hepatitis B:
Transmission:
o Body fluids (blood, semen), including transfusion & contaminated needles
o Mother to baby (vertical transmission): 95% risk of infection –
vaccinate at birth and give Anti-HBs – immune globulin
o Organ transplant
o Child to child (horizontal transmission). Must get into blood – e.g.
grazes, stubbed toes. Very resilient virus. Children are most likely to have
asymptomatic seroconversion
· Diphtheria:
o Corynebacterium diphtheriae ® respiratory and cutaneous infection (grey membrane on throat). Exotoxin causes cardiac toxicity and ascending paralysis. Spread by nasal droplets
o 1 imported case in last 20 years.
Till 1945 killed 100 babies a year.
High is USSR in 90s.
o Vaccine: inactivated diphtheria toxoid, boosters every 10 years. > 80% efficacy
· Tetanus:
o Clostridium tetani from soil and animal faeces ® muscular rigidity due to neurone specific toxin, 10% mortality
o 3 notifications per year (old ladies in the garden). Common in environment Þ no herd
immunity
o Vaccine: Inactivated toxoid, boosters every 10 years, 100% efficacy
· Pertussis:
·
Bordetella Pertussis = Whooping
Cough
·
Treatment: if < 4 weeks
duration: erythromycin. Doesn‟t
impact illness after paroxysmal phase is established, but will ¯
infectivity
·
Admit if under 6 months and/or
cyanosis or apnoea in paroxysms
·
Polio:
o Enterovirus spread by faeces and saliva
o Presentation:
§ Usually asymptomatic or mild (fever, headache, nausea, vomiting
§ Only 1% of infected get severe clinical disease: severe muscle pain,
neck and back stiffness ® flaccid paralysis
o Last wild virus infection in 1962.
Occasional imported and vaccine associated cases
o Vaccine:
§ Live oral polio (OPV) > 90% protection after 3 doses. < 1% of recipients develop diarrhoea, headache or muscle pains. 1 in 2.5 million recipients or close contacts develop paralysis (more common in immunosuppressed) = Vaccine Associated Polio Paralysis (VAPP)
§ Inactivated polio vaccine (IPV) for immunocompromised (will be used more
widely when it can be combined with other jabs)
· Haemophilus influenzae type B (HIB):
·
Caused by Haemophilus Influenza
Type B
·
Incidence ~ 20 cases pa (dropped from
160 in 1992 prior to vaccination)
·
Presentation:
o Incubation for 2 – 4 days
o Acute, febrile illness, toxic looking child
o Snore, mouth always open, drooling, prefers to sit upright. Soft
inspiratory stridor, louder expiratory stridor
o No cough (cf croup)
·
Management:
o Blood cultures
o Intubate first, then give iv antibiotics (if given first, pain ® panic ® respiratory arrest)
o Cefotaxime 25 – 50 mg/kg/8hr iv (max 2g) due to penicillin
resistance
o Amoxycillin 50 mg/kg/4 hr iv (max 2g) if penicillin sensitive
·
Other illnesses caused by H
Influenzae type B:
· Measles:
· Highly contagious paramyxovirus spread by coughing and nasal droplets
·
Treatment: Supportive, antibiotics
for 2ndary infection
·
Complications:
o Otitis media (10%)
o Pneumonia (1 – 5%)
o Encephalitis (0.1%): 15% die and 25% left severely disabled. 1 in
100,000 develop the fatal grey matter degenerative disorder Subacute Sclerosing
Panencephalitis (SSPE)
· Vaccine:
o Live attenuated virus. Now MMR2 given at 4 years to time between epidemics and address 2 – 5% chance of primary vaccine failure in first dose
o Mild fever, malaise or rash develops in about 1% 7 – 10 days after
vaccination
o 1 in 1 million develop encephalitis (1,000 fold less likely than if
infected with wild virus)
o Contraindicated during pregnancy and in immunocompromised hosts
· Mumps:
·
Contagious paramyxovirus spread
by saliva and droplets
·
~ 80 notified cases per
annum. Used to be 3 – 4 year epidemics, now
longer
·
Presentation:
o Incubation 2 – 3 weeks
o 70% develop fever and swelling and tenderness of salivary glands
o 15% have aseptic meningitis
o 0.2% develop encephalitis
o 20% of post-pubertal males have painful orchitis
o Case fatality is 0.02% - usually from encephalitis
· Infective 1 week before and after parotid swelling starts
·
Rubella:
o Togavirus spread by nasal droplets
o Presentation:
§ Incubation 2 – 3 weeks
§ Fever, headache, mild conjunctivitis, erythematous maculo-papular rash,
lymphadenopathy (especially posterior triangle), arthritis, arthralgia
§ 50% develop the rash and lymphadenopathy
§ 50% of adolescents and adults have arthralgia or even frank arthritis
§ 1 in 5,000 have encephalitis
o Complications:
§ Congenital rubella syndrome: 90% of embryos of mothers infected in 1st trimester will abort or have major abnormalities (severely retarded, seizures, deafness, cardiac defects). Frequent problems after birth
§ Rate of congenital rubella is 5 times the US rate
o ~ 60 notifications per annum (1600 in 1995)
o Vaccine:
§ 98 % protective
§ To protect the unborn child only – relies on herd immunity. Need to vaccinate guys as well otherwise they will maintain a population reservoir which women with vaccine failure will catch
§ 5% of adolescents and adults have arthralgia and 1% have non-infectious
rash
§ Contra-indicated in pregnancy and immunosuppressed
·
Influenza:
o Virus types A (H3N2 and H1N1) and B
o Causes Fever, rigors, headache, myalgia, protraction. Estimated 400 deaths per annum.
o Vaccine: inactivated subunit vaccine for new strains (resulting from
„antigenic drift‟). 60 –90% effective. Contraindicated if egg allergy
o Pandemics result from „antigenic shift‟
·
Tb: BCG: See Mycobacteria,
·
Pneumococcal Disease:
See Streptococcus Pneumoniae
·
Varicella Zoster: See Infectious
Diseases,
Related Topics