Chapter: Medicine Study Notes : Infectious Diseases
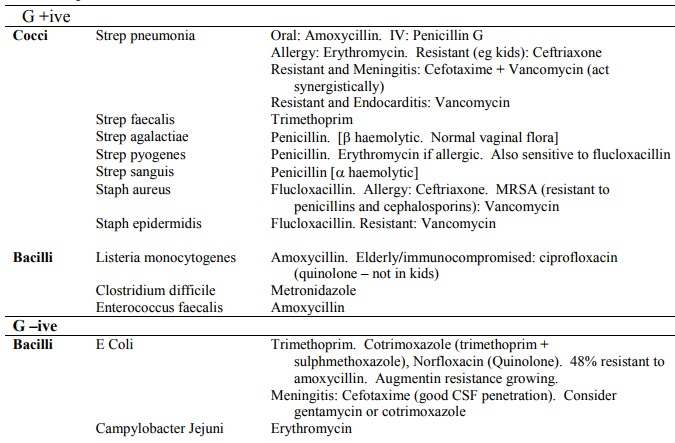
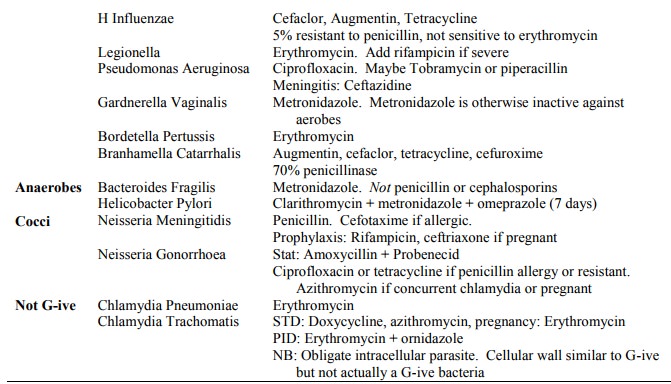
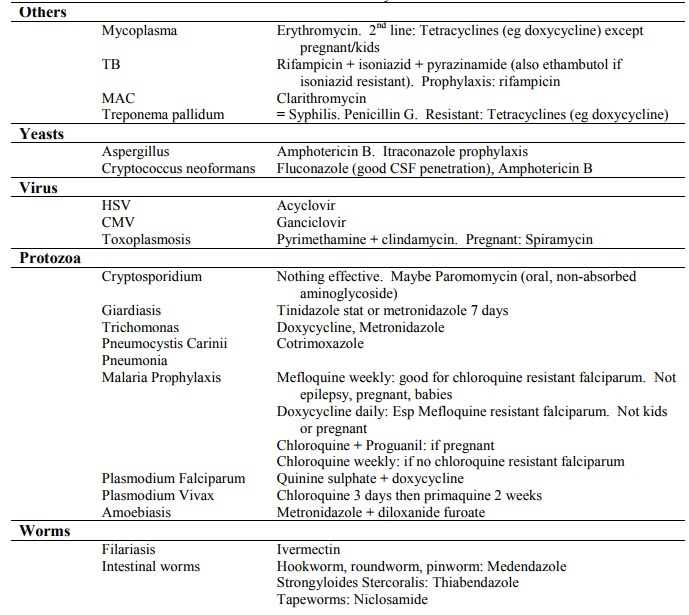
Antibiotic Treatment
Antibiotic Treatment
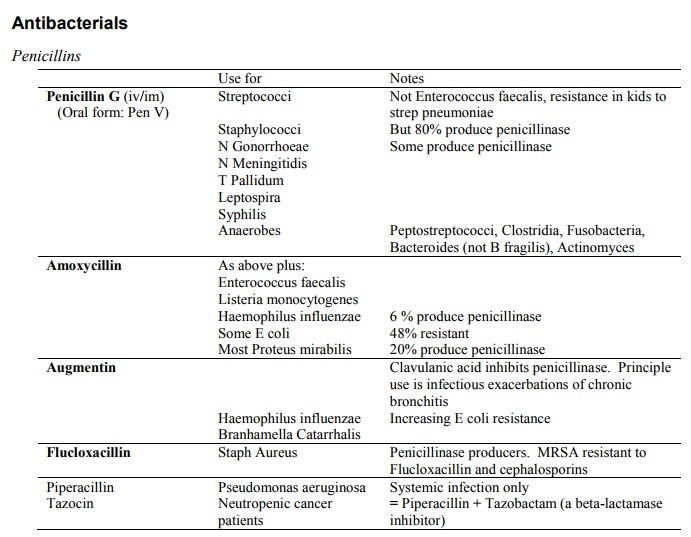
Summary
Macrolides
·
Effective against:
o Staph aureus (up to 10% resistance in community strains)
o Streptococci (not E faecalis)
o Anaerobes (only moderately effective against B fragilis)
o Mycoplasma pneumoniae
o Chlamydia pneumoniae
o Chlamydia trachomatis (but tetracycline is the drug of choice)
o Campylobacter jejuni
·
Ineffective against:
o H influenzae
o No CSF penetration
·
Indications:
o Treatment of susceptible bacteria if penicillin allergy
o Atypical pneumonia (eg Mycoplasma, Chlamydia or Legionella)
o Campylobacter
o Chlamydia infection in pregnant women
Erythromycin
·
New analogues:
o Roxithromycin (Rulide)
o Clarithromycin (Klaricid): Treatment of MAC, especially in AIDS patients
o Azithromycin (Zithromax): Single dose treatment for STD‟s caused by
Chlamydia trachomatis or
o N. gonorrhoeae (especially in pregnancy)
Vancomycin
·
G+ive wonder drug – active
against G+ive only
· Indications:
o Systemic infections caused by MRSA or MRSE (Epidermidis), or infected Hickman lines in cancer patients
o Infective Endocarditis due to Strep or Staph with penicillin allergy
o Clostridium difficile colitis (by mouth). First line is metronidazole
·
Otto and nephrotoxic
·
Teicolpanin: similar drug, active
against some Vancomycin Resistant Enterococci (VRE)
Rifampicin
·
Always used in combination
(except meningitis prophylaxis)
·
Active against M. Tb, Staph
aureus, Legionella
·
Indications:
o TB (in combination)
o Severe Staph aureus infections (eg infective endocarditis) in
combination
o Severe legionella pneumonia (in combination with erythromycin)
o Prophylaxis against N meningitides or HIB
Aminoglycosides
·
Active against all coliform
bacilli (eg E Coli), pseudomonas, staphylococci
·
Inactive against: streptococci,
anaerobes
·
Indications: G- sepsis, perforated
appendix
· Drugs:
o Gentamicin
o Tobramycin: more active against pseudomonas
o Amikacin: reserved for Gentamycin resistant bugs
·
Spectinomycin: N gonorrhoeae
(penicillinase producers)
·
Otto and nephrotoxic
Cotrimoxazole
·
= Trimethoprim + Sulphamethoxazole
·
Broad spectrum: Staph, Strep,
many coliforms (not Pseudomonas), HIB, Pneumocystis, Brucella
· Indications: Acute infectious exacerbations of chronic bronchitis, PCP in AIDS
·
Trimethoprim on its own is the standard
treatment against community acquired UTI (E Coli, Klebsiella, Proteus, Strep faecalis)
Quinolones
· Broad spectrum oral antibiotic
· Active against: most coliforms, pseudomonas aeruginosa (main use), Staphs (including MRSE and MRSA), N gonorrhoeae, HIB, Branhamella catarrhalis (good), Salmonella, Shigella, Yersinia, Campylobacter
· Poor activity against Anaerobes, streptococci
·
Can damage growth cartilage Þ not
licensed for children
·
Indications:
o Norfloxacin: resistant UTIs
o Ciprofloxacin: Mainly pseudomonas
Tetracyclines
·
Eg doxycycline (once a day on full stomach), very common in treatment
of STIs
·
Active against Staphs, Streps,
Coliforms, HIB
·
Other indications:
o Syphilis and Gonorrhoea if penicillin allergy
o Mycoplasma pneumoniae
·
Contraindications: young
children, pregnancy, renal failure (except doxycycline)
Metronidazole
·
= Flagyl
· Active against all anaerobes (eg B fragilis)
· Inactive against aerobes (excl Gardnerella vaginalis, causing bacterial vaginosis, where it is drug of choice)
·
Active against Protozoa:
Trichomonas vaginalis, Giardia lamblia
Other
· Fucidin: active against Staph Aureus, must be used in conjunction with, eg Flucloxacillin. Use in bone/joint infections
·
Chloramphenicol: for infections
caused by Burkholderia cepacia
Antifungals
·
Nystatin (topical): vaginal or oral
candida
·
Miconazole (topical): Candida and
dermatophytes (except scalp or nails)
· Terbinafine (oral) Dermatophyte infections of scalp or nails (has superseded Griseofulvin)
· Itraconazole (oral): Dermatophyte infections of scalp or nails, prophylaxis in Candida and Aspergillus in immunocompromised
·
Fluconazole (Oral/IV): active against yeasts
(candida, cryptococcus). Good CSF penetration (eg Cryptococcal meningitis)
· Amphotericin B (IV): Very good but side effects, including nephrotoxicity
Antivirals
·
Acyclovir: active against HSV and VZV
(less active)
·
Ganciclovir: CMV in immunocompromised
patients. Bone marrow suppression ® neutropenia
Related Topics