Chapter: Essentials of Anatomy and Physiology: The Urinary System
Tubular Reabsorption - Formation of Urine
TUBULAR REABSORPTION
Tubular reabsorption takes place from the renal tubules into the peritubular capillaries. In a 24-hour period, the kidneys form 150 to 180 liters of filtrate, and normal urinary output in that time is 1 to 2 liters. Therefore, it becomes apparent that most of the renal filtrate does not become urine. Approximately 99% of the filtrate is reabsorbed back into the blood in the peritubular capillaries. Only about 1% of the filtrate will enter the renal pelvis as urine.
Most reabsorption and secretion (about 65%) take place in the proximal convoluted tubules, whose cells have microvilli that greatly increase their surface area. The distal convoluted tubules and collecting tubules are also important sites for the reabsorption of water (Fig. 18–4).
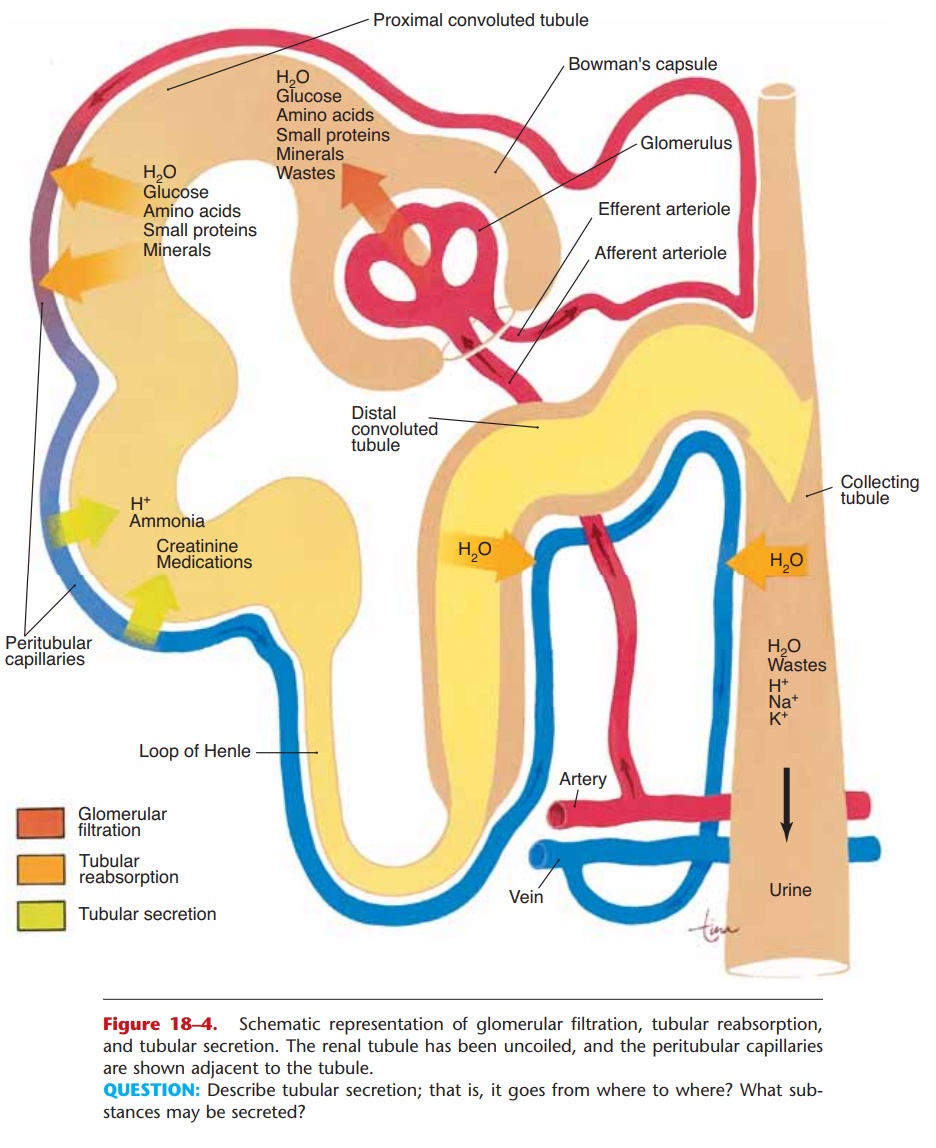
Figure 18–4. Schematic representation of glomerular filtration, tubular reabsorption, and tubular secretion. The renal tubule has been uncoiled, and the peritubular capillaries are shown adjacent to the tubule.
QUESTION: Describe tubular secretion; that is, it goes from where to where? What sub-stances may be secreted?
Mechanisms of Reabsorption
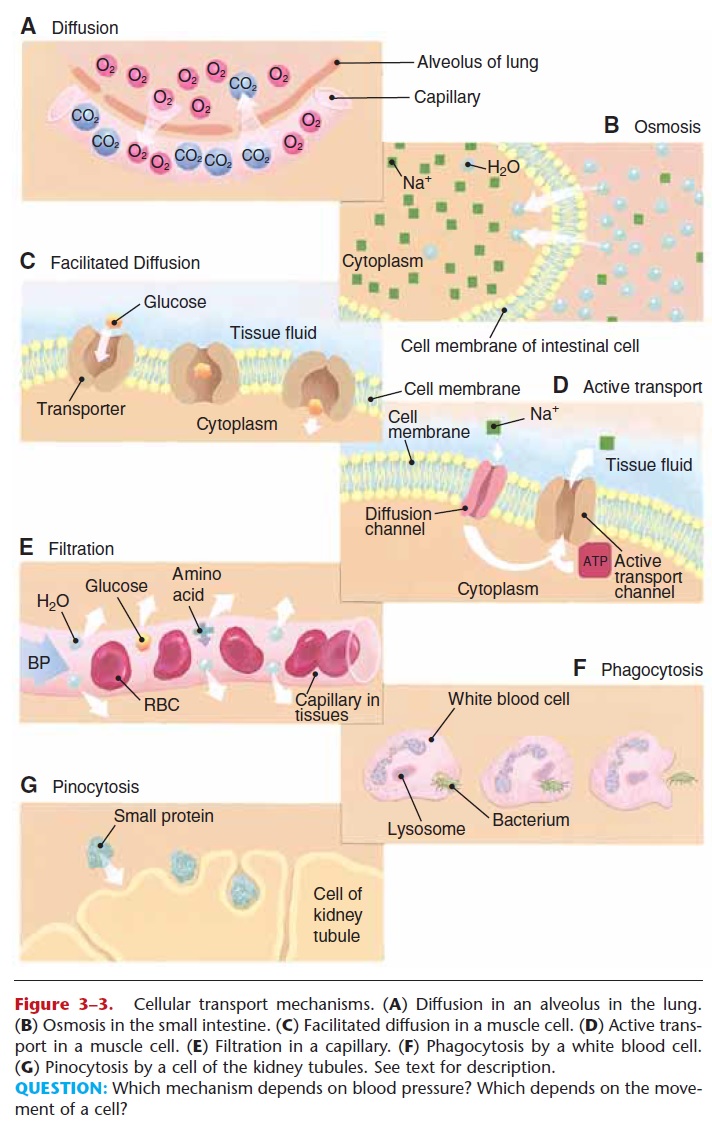
1. Active transport—the cells of the renal tubule use ATP to transport most of the useful materials from the filtrate to the blood. These useful materials include glucose, amino acids, vitamins, and positive ions.
For many of these substances, the renal tubules have a threshold level of reabsorption. This means that there is a limit to how much the tubules can remove from the filtrate. For example, if the filtrate level of glucose is normal (reflecting a normal blood glucose level), the tubules will reabsorb all of the glucose, and none will be found in the urine.
What happens is this: The number of glucose transporter molecules in the membranes of the tubule cells is sufficient to take in the number of glucose molecules passing by in the filtrate. If, however, the blood glucose level is above normal, the amount of glucose in the filtrate will also be above normal and will exceed the threshold level of reabsorption. The number of glucose molecules to be reabsorbed is more than the number of the transporter molecules available to do so. In this sit-uation, therefore, some glucose will remain in the filtrate and be present in urine.
The reabsorption of Ca12 ions is increased by parathyroid hormone (PTH). The parathyroid glands secrete PTH when the blood calcium level decreases. The reabsorption of Ca12 ions by the kidneys is one of the mechanisms by which the blood calcium level is raised back to normal.
The hormone aldosterone, secreted by the adre-nal cortex, increases the reabsorption of Na+ ions and the excretion of K+ ions. Besides regulating the blood levels of sodium and potassium, aldosterone also affects the volume of blood.
2. Passive transport—many of the negative ions that are returned to the blood are reabsorbed following the reabsorption of positive ions, because unlike charges attract.
3. Osmosis—the reabsorption of water follows the reabsorption of minerals, especially sodium ions. The hormones that affect reabsorption of water are discussed in the next section.
4. Pinocytosis—small proteins are too large to be reabsorbed by active transport. They become adsorbed to the membranes of the cells of the prox-imal convoluted tubules. The cell membrane then sinks inward and folds around the protein to take it in (see Fig. 3–3 for depictions of this and the other transport mechanisms). Normally all proteins in the filtrate are reabsorbed; none is found in urine.
Related Topics