Geographical Distribution, Habitat, Morphology, Life Cycle, Pathogenesis, Clinical Features, Prevention and Control - Tissue Flagellates - Leishmania donovani | 12th Microbiology : Chapter 8 : Medical Parasitology
Chapter: 12th Microbiology : Chapter 8 : Medical Parasitology
Tissue Flagellates - Leishmania donovani
Tissue Flagellates – Leishmania
donovani
The genus
is named after the scientist Leishman, who first described the parasite in
London in May 1903.
Geographical Distribution
Leishmania
species is found in the Mediterranean, the Middle East, Africa and Asia
including India.
Habitat
Leishmania donovani is an
obligate intracellular parasite of
human and other mammalian hosts. They are always found as intracellular
amastigotes in the reticuloendothelial cells of the spleen, bone marrow, liver,
intestinal mucosa and mesenteric lymph nodes of hosts.
Morphology
The
parasite exists in two forms:
Amastigote: It is the form found in human and other mammalian hosts. They are found inside monocytes, polymorphonuclear
leucocytes or endothelial cells. They are small, round to oval bodies measuring
2–3µm in length (Figure 8.8). They are also known as LD (Leishman donovan)
bodies.
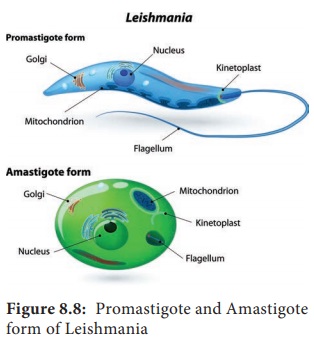
Promastigote: These forms are found in the mid-gut of sand fly and in the culture media. The fully developed promastigotes are long, slender and spindle – shaped. They measure 15µm to 25µm in length and 1.5µm to 3.5µm in breadth. A single nucleus is situated at the centre. The kinetoplast lies near the anterior end. The flagellum is single, delicate and measures 15µm–28µm (Figure 8.8).
Infobits
There are 3 main forms of Leishmaniases - Visceral (also known
as Kala-agar and the most serious form of the disease), cutaneous (the most
common) and mucocutaneous. The disease affects some of the poorest people on
earth, and is associated with malnutrition, population displacement, poor
housing, a weak immune system and lack of financial resources. Leishmaniasis is
linked to environmental changes such as deforestation, building of dams,
irrigation schemes, and urbanization
PKDL occurs in all areas endemic for L.donovani but is commonest
in East Africa and on the Indian subcontinent, where up to 50% and 10% of
patients with kala-azar, respectively develop the condition. The frequency is
reported to be declining in India.
Cutaneous Leishmaniasis
The clinical spectrum of cutaneous leishmaniasis ( oriental
sore) is broad and may mimic that of other skin conditions, such as
staphyloccal or streptococcal infection, mycobacterial ulcer, leprosy, fungal
infection, cancer, sarcoidosis ulcer.
Life – Cycle of Leishmania donovani
Leishmania donovani completes
its life cycle in two different
hosts. The complete life cycle is given in Figure 8.9.
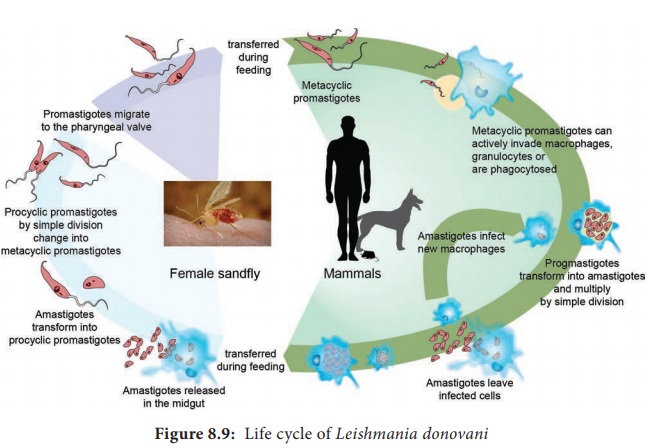
Development in Human
The
parasite is transmitted to human and other vertebrate hosts by the bite of
blood sucking female sandfly. During the blood meal, the sandfly deposists
promastigotes on surface of the skin. These promastigotes are immediately
phagocytosed by fixed macrophages of the host, in which they are transformed
into amastigotes. The amastigotes multiply by binary fission within the
macrophages. As many as 50 to 200 amastigotes may be present inside the
enlarged cell. These are called LD bodies. The rupture of cell releases amastigotes
in large numbers which inturn are free to infect other cells. Free amastigotes
are subsequently carried by circulation. These forms invade monocytes of the
blood and macrophages of the spleen, liver, bone marrow, lymph nodes and other
tissues of the reticuloendothelial cells.
Development in sandfly
Female sandfly during a blood meal ingest free, as well as intracellular amastigotes in the blood. In the mid gut of the sandfly, the amastigotes are transformed within 72 hours to flagellated promastigotes. These promastigotes multiply by binary fission. After a period of 6 to 9 days, these forms migrate from the midgut to the pharynx and buccal cavity of sandfly. Bite of the infected sandfly transmits infection to susceptible persons and the life – cycle is repeated.
Pathogenesis
Leishmania donovani causes
visceral Leishmaniasis. The disease
is also known as Dum – Dum fever, Asian fever, Assam fever, or infantile
splenomegaly. Leishmaniasis is a disease of the reticuloendothelial system. Proliferation
and destruction of reticuloendothelial cells of the internal organs are
responsible for the pathological changes in visceral leishmaniasis.
Spleen,
liver and lymphnodes are enlarged in this condition. Bone marrow is dark red in
colour and shows extensive proliferation of reticuloendothelial cells. Kidney
shows cloudy swelling and is invaded by macrophages parasitized by amastigotes
Clinical Features
Incubation
period: It is usually 3–6 months but can be months or years.
Visceral
Leishmaniasis is a serious and fatal systemic disease. In India, the disease is
called Kala – azar meaning “black disease”.
The
disease is characterized by the presence of fever, hepatosplenomegaly (Figure
8.10) (the simultaneous enlargement of both liver and the spleen),
hypergammaglobulinemia (a condition in which increased levels of a certain
immunoglobulin in blood serum), Leucopenia, Thrombocytopenia (deficiency of
platelets in the blood), Cachexia (a condition that causes extreme weight loss)
with marked anemia, emaciation and loss of weight. Epistaxis (bleeding from
nose) and bleeding from gums are common. In Indian patients, the skin on the
hands, feet, abdomen, around the mouth and fore – head becomes grayish and dark
coloured. This hypo – pigmentation of the skin is unique in Indian patients
giving the disease name Kala – azar.

Post kala
– azar dermal leishmaniasis (PKDL): It is a non – ulcerative lesion of the
skin, which is seen after completion of treatment of the kala – azar. This
condition is characterized by multiple, hypopigmented, erythematous macules
involving the face and trunk (Figure 8.11). In Indian forms, PKDL appears after
a latent period of 2 years and may even persist as long as 20years, creating a
persistent human reservoir of infection.

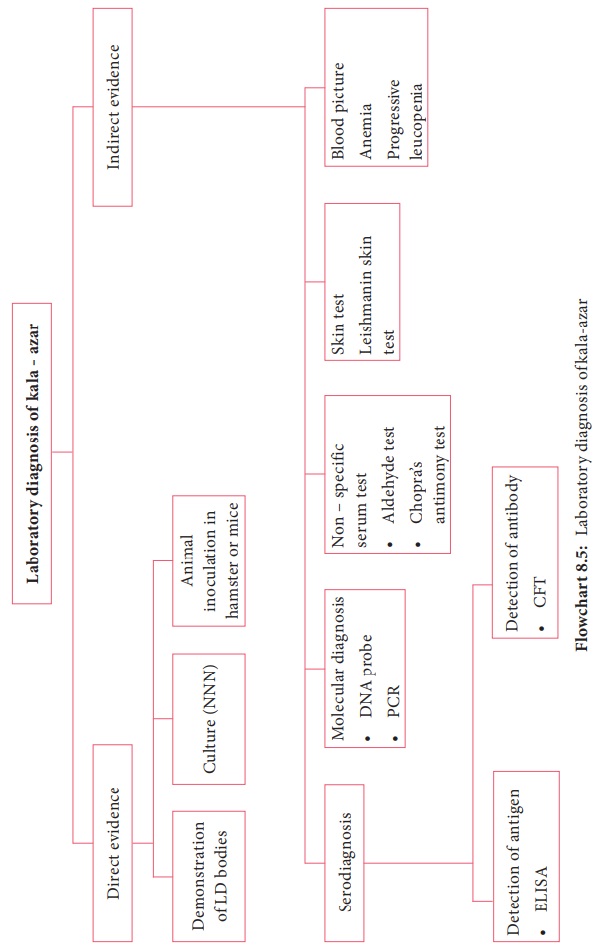
Laboratory diagnosis
Specimens: Aspiration from spleen, bone marrow, lymph node, liver biopsy and peripheral blood. Methods of examination: This includes, microscopy and culture
1. Direct microscopy
The
amastigotes of Leishmania donovani
(known as LD bodies) can be demonstrated in the smears of spleen, bone marrow,
liver, lymph node and peripheral blood stained in Leishman, Giemsa or wright
stains. Splenic aspiration is the most sensitive method to detect LD bodies.
Examination of peripheral blood smear and buffy coat smear is more commonly
used to find LD bodies in the circulating monocytes.
2. Culture
Promastigotes
are found in the culture media. Tissue samples and aspirates are inoculated in
the NNN (Novy–MacNeal–Nicolle) medium for demonstration of promastigotes.
Laboratory
diagnosis of kala – azar is briefly discussed in Flowchart 8.5.
Treatment: Pentavalent antimonials are the drugs of choice. Pentamidine, Amphotericin B and
Miltefosine (oral drug) are recommended.
Prevention and Control
Integrated
insecticidal spraying (DDT and Malathion) to reduce sandfly population.
Reduction
of reservoir by killing all the infected dogs.
Personal
prophylaxis by using anti – sandfly measures like using thick clothes, bed
nets, window mesh or insect repellants and keeping the environment clean.
No
vaccine is available against kala – azar.
Related Topics