Geographical Distribution, Habitat, Morphology, Life Cycle, Pathogenesis, Clinical Features, Laboratory Diagnosis, Prevention and Control - Intestinal Amoeba – Entamoeba histolytica | 12th Microbiology : Chapter 8 : Medical Parasitology
Chapter: 12th Microbiology : Chapter 8 : Medical Parasitology
Intestinal Amoeba – Entamoeba histolytica
Intestinal Amoeba – Entamoeba
histolytica
Geographical Distribution
It is
Worldwide in distribution they are more common in the tropics than elsewhere.
It is found wherever sanitation is poor.
Habitat
Trophozoites
of E.histolytica live in the mucous
and submucous layers of the large intestine of human.
Morphology
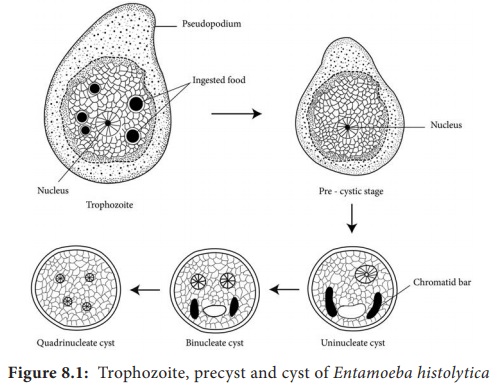
E.histolytica occurs in 3 forms as Trophozoite, Precyst and Cyst.
Trophozoite: It is the growing or feeding stage of the parasite. It is
the only form present in tissues. It has no fixed shape. They vary in size from
18 to 40µ, average being 20 to 30µ. The cytoplasm is usually described as outer
ectoplasm and inner endoplasm (Figure 8.1). The endoplasm contains nucleus,
food vacuoles, erythrocytes, occasionally leucocytes and tissue debris. The
nucleus is characterised by evenly arranged chromatin on the nuclear membrane
and the presence of a small, compact, centrally located karoyosome (It is a DNA
containing body, situated peripherally or centrally within the nucleus).
Trophozoites exhibits active crawling or gliding motility by forming
finger-like projections called Pseudopodia.
The trophozoite reproduce by binary fission in every 8 hours.
Trophozoites survives upto 5 hours at 37°C and are killed by heat, drying and
chemical sterilization. Even if live trophozoites from freshly passed stools
are ingested, they are rapidly destroyed in stomach and cannot initiate
infection. Therefore, the infections is not usually transmitted by
trophozoites.
Precyst
Trophozoites
undergo encystment in the intestinal lumen. Encystment does not occur in the
tissue or in feces outside the body. Precyst is smaller in size about 10 -20 µm
in size. It is round or oval in shape. The endoplasm is free of red blood cells
and other ingested food particles (Figure 8.1). The nuclear structure retains
the characteristics of the trophozoite.
Cyst
Precyst
secretes a highly refractive cyst wall around it and becomes a cyst. A mature
cyst is a quadrinucleate spherical body. The cyst begins as a uninucleate body
but soon divides by binary fission and develops into binucleate and
quadrinucleate bodies (Figure 8.1). The cytoplasm of the cyst is clear and
hyaline (translucent) and the nuclear structure retain the characteristic of
the trophozoites.
The mature quadrinucleate cyst, passed in the
stool, does not undergo any further development and remain alive for several
months in the soil or in environment where they were deposited. The mature
quadrinucleate cysts are the infective forms of the parasite.
Life – Cycle of Entamoeba histolytica
E. histolytica passes its life cycle only in one host, the human.
Infective form: Mature quadrinucleate cyst.
Mode of transmission: Ingestion
of food and water contaminated with
cyst
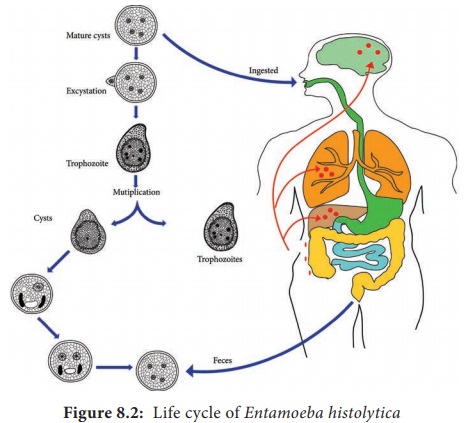
The cysts
that are swallowed along with food and water enter into the alimentary canal.
The cyst wall is resistant to action of gastric juice. The cysts pass through
the stomach undamaged and enters the small intestine (Figure 8.2).
When the cyst reaches caecum or lower part of
the ileum, due to alkaline medium, the cyst wall is damaged by trypsin leading
to excystation.
The amoeba infecting man may be classified according to their
pathogenicity and habitat.
A. Pathogenic Intestinal Amoeba: Entamoeba
histolytica
B. Non pathogenic Mouth Amoeba: Entamoeba
gingivitis Intestinal Amoeba: Entamoeba coli Entamoeba nana
• The
cytoplasm gets detached from the cyst wall and an amoeboid movement appear
causing a tear in the cyst wall, through which quadrinucleate amoeba is
liberated. This stage is called the metacyst.
• The
nuclei in the metacyst immediately undergo division to form 8 nuclei, each of
which gets surrounded by its own cytoplasm to become 8 small amoebulae or
metacystic trophozoites.
• These
metacystic trophozoites are carried to the caecum and colon. They invade the
tissues and lodge in the submucous tissue of the large intestine which is their
normal habitat.
• Trophozoite
grow and multiply by binary fission. The trophozoite phase of the parasite is
responsible for producing the characteristic lesion of amoebiasis
• Some of the trophozoites in colon develop into precystic forms and cysts, which are passed in feces to repeat the cycle.
Pathogenesis
E. histolytica causes intestinal and extra intestinal amoebiasis (Flowchart 8.3).
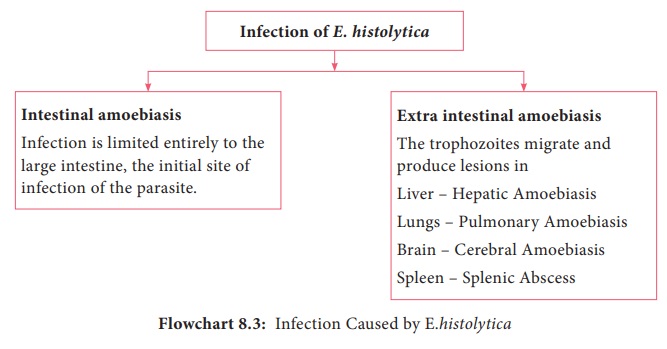
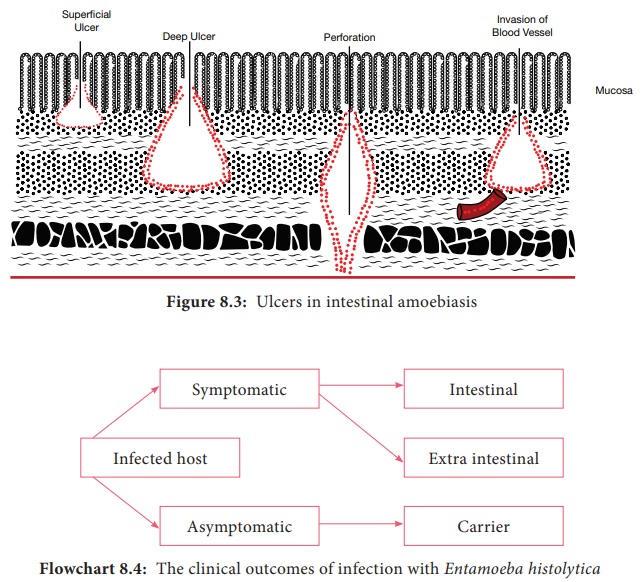
E. histolytica can live in the intestine without causing symptoms. But, they can also cause severe disease. These amoebas may invade the wall of the intestine leading to amoebic dysentery, an illness that causes intestinal ulcers, bleeding, increased mucus production and diarrhoea. The ulcers are strictly confined to the large intestine being most numerous in the caecum and next in the sigmoid-rectal regions. The lesions may be generalized or localised. A typical amoebic ulcer varies from pin’s head to one inch or more in diameter in size. The shape of ulcer may be round or oval. On vertical section, the ulcer appears like flask, with mouth and neck being narrow and base being large and rounded (Figure 8.3 shows the flask – shaped ulcer). The base of ulcer is generally formed by the muscular coat and filled up by the necrotic material. The ulcers generally do not extend deeper than submucosal layer.
Clinical Features
Incubation
period is highly variable, but is generally 4 to 5 days.
A wide
spectrum, from asymptomatic infection (luminal amoebiasis), to invasive
intestinal amoebiasis (dysentery, colitis, appendicitis, toxic mega colon,
amoebomas), to invasive extraintestinal amoebiasis occurs. Flowchart 8.4
classifies the clinical outcomes of infection with Entamoeba histolytica.
Only about 10% to 20% of people who
are infected with E. histolytica
become sick from the infection.
The
typical manifestation of intestinal amoebiasis is amoebic dysentery. The
symptoms are often quite mild and can include loose feaces, stomach pain and
stomach cramping. In acute amoebic dysentery, the symptoms include abdominal
pain, bloody stool, fever, tenderness, rectal tenesmus and hepatomegaly
(enlargement of liver). People affected may develop anemia due to loss of blood.
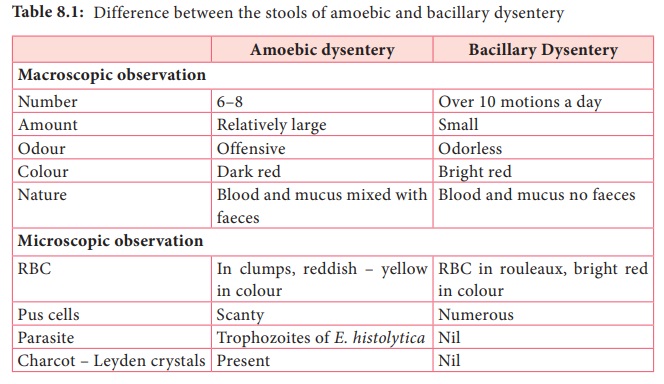
On clinical and laboratory ground, amoebic dysentery should be differentiated
from bacillary dysentery. A Table 8.1 shows the difference between the stools
of amoebic and bacillary dysentery.
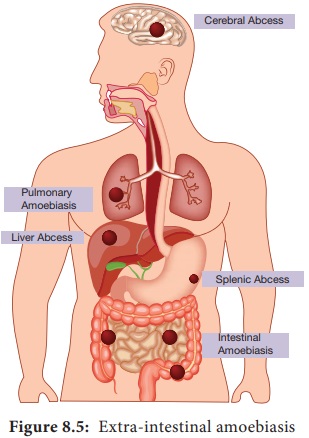
Extra intestinal amoebiasis
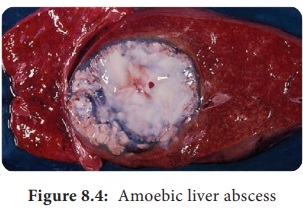
1. Hepatic amoebiasis: This is
the most common form of extra
intestinal invasive amoebiasis. Liver abscess may be multiple or more often
solitary, usually located in the upper right lobe of the liver (Figure 8.4).
Amoebic liver abscess (ALA) contains an odour less and thick chocolate brown pus
called anchovy sauce pus. ALA is associated with an abrupt onset of high fever,
right upper abdominal pain and tenderness. Anorexia (loss of appetite for
food), nausea (the sensation to vomit), vomiting, fatigue (extreme tiredness)
and weight loss are also frequent.
2. Pulmonary Amoebiasis: It is very rare, but this may occur by direct hematogenous spread from the colon. The patient presents with severe chest pain and have dyspnoea (shortness of breath). The sputum of patient is chocolate brown. Amoebic trophozoites may be demonstrated in the sputum.
3. Cerebral
amoebiasis: The condition is
unusual. In cerebral amoebiasis, the abscess is single, small and is located in
the cerebral hemisphere. The patient may die of rupture or involvement of
cerebellam within 12–72 hours. Biopsy of the brain shows the amoebic
trophozoites.
4. Cutaneous
amoebiasis: It can be caused by
perforation of an amoebic abscess or surgical wound infected with amoebae. It
is less frequent condition.
5. Genitourinary Amoebiasis: This condition includes amoebiasis of the
kidney and genital organs. Amoebiasis of the genital organs is a rare
condition. Lesions of amoebiasis is shown in Figure 8.5.
Laboratory Diagnosis
Specimens: Stool is the specimen of choice. Other specimens collected includes blood, rectal exudates
and rectal ulcer tissue collected from the base by endoscopies.
Methods in examination of stool
A. Direct
wet mount examination of stool: Demonstration of mature quadrinucleate cysts or
trophozites in stool is diagnostic of intestinal amoebiasis. The wet mount of
stool is prepared in the saline, iodine or lacto phenol cotton blue.
B. Examination
of stool after concentration: Demonstration ofamoebic cysts by Formalin – ether
is the method of choice
C. Examination of stained stool smears: Staining by
iron haematoxylin, Periodic Acid – Schiff (PAS) stains demonstrate the presence
of both trophozoites and cyst.
Amoebic
liver abscess (ALA): Demonstration of amoebic trophozoites in the aspirated
liver pus establishes the diagnosis of ALA.
Serology: Detection of amoebic antigens in the serum by Enzyme Linked Immunosorbent Assay
(ELISA).
Molecular diagnosis: PCR(Polymerase chain
reaction) is employed to detect amoebic genome in the aspirated liver pus for
the diagnosis of ALA.
Imaging
methods: X – Ray magnetic resonance
imaging (MRI) scan and computerized Axial Tomography (CAT) Scan are the imaging
methods used
Treatment:
Eradication
of amoebae by the use of amoebicidal
drugs and replacement of fluid and electrolyte is the treatment for amoebiasis.
Listed below the drugs used in the treatment for amoebiasis.
• Paramomycin and iodoquinol acts in the intestinal
lumen but not in tissues.
• Emetine, chloroquine are effective in systemic
infection. They act only on trophozoites.
Metronidazole
is the drug of choice which acts as both luminal and tissue amoebicides. It is
low in toxicity and is effective against intestinal as well as extra
-intestinal amoebic infections.
Prevention and Control
• Proper
sanitation is the key to avoid amoebiasis. Washing hands with soap and water
after using the bathrooms and before handling food
• Drinking
safe and boiled water.
• Avoid
eating unwashed fruits and vegetables
• Prevention
of water supplies from faecal contamination.
• Early
rapid detection of diseased people and subsequent treatment with amoebicidal
drugs. No vaccine is available yet against amoebiasis in humans.
Related Topics