Geographical Distribution, Habitat, Human and Mosquito Vectors, Cycle, Pathogenesis, Clinical Manifestations - Sporozoa - Plasmodium | 12th Microbiology : Chapter 8 : Medical Parasitology
Chapter: 12th Microbiology : Chapter 8 : Medical Parasitology
Sporozoa - Plasmodium
Sporozoa - Plasmodium
Protozoan
parasites characterised by the production of spore ŌĆō like oocysts containing
sporozoites were known as sporozoa. The parasites belonging to this group of
protozoa do not possess any special organs of locomotion, such as flagella or
cilia. The medically important parasite of this class that is given in the text
is malarial parasite.
Malaria
It is the
disease condition with seasonal intermittent fevers, chills and shivering. The
name malaria (Mal: bad, aria: air) was given in the 18th century in Italy. The specific
agent of malaria was discovered in RBCŌĆÖs of a patient in 1880 by Alphonse
Laveran. In 1897, Ronald Ross identified the developing stages of malarial
parasites in mosquitoes in Secunderabad, India. This led to various measures
for the control and possible eradication of malaria by mosquito control. Both
Ross (1902) and Laveran (1907) won the Nobel Prize for their discoveries in
malaria
The single most important protozoan disease is malaria, which
causes 1.5 million deaths each year.Different species of malaria parasites can
develop in the same mosquito and such an infected mosquito can transmit the
infection to man giving rise to cases of ŌĆ£mixed infectionŌĆØ the commonest being
P. falciparum with P. vivax.
Infobits
Three basic types of malaria
1. Benign tertian (P. vivax and P.
orale) with a fever every 2nd day (Example: Monday ŌĆō fever, TuesdayŌĆō no fever, Wednesday
ŌĆō fever).
2. Benign quartan (P. malariae) with
a fever every 3rd day. (Example: Monday; fever, Tuesdayno fever, Wednesday ŌĆō no
fever, Thursday ŌĆō fever.
3. Malignant tertian (P. falciparum),
in which the cold stage is less pronounced and the fever stage is more
prolonged and severe. This type of malaria is more dangerous because of the
complications caused by capillary blockage (i.e, convulsion, coma, acute
pulmonary insufficiency and cardic failure). Large numbers of erythrocytes are
parasitized and destroyed, which may result in dark-coloured urine. (black
water fever); intravascular hemolysis, hemoglobinuria, and kidney failure). Two
species of plasmodium, P. vivax and P. ovale, can remain in the liver, if not
treated properly. The organism leave the liver and re-infect erythrocytes,
causing the symptoms.
Causative agents of human malaria:
The
organisms: Four species of Plasmodium cause malaria in humans.
ŌĆó Plasmodium
vivax: (Benign Tertian malaria)
ŌĆó Plasmodium
falciparum: (Malignant tertian
malaria)
ŌĆó Plasmodium
malaria: (Benign Quartan malaria)
ŌĆó Plasmodium
ovale: (Benign tertian malaria)
The two
most common species are P. vivax and P. falciparum, WHO reports (2018) that
falciparum being the most pathogenic of all.
Geographical Distribution
Malarial
parasites are found in all countries. In India, malaria continues to be a major
public health threat.
Habitat
The
malarial parasites infecting man, after passing through a developmental phase
in the parenchyma cells of the liver, reside inside the red blood corpuscles
and are carried by the circulating blood to all the organs.
Vectors
Human
malaria is transmitted by over 60 species of female Anopheles mosquito.
Human malarial parasite ŌĆō Plasmodium falciparum
Of all the
human malaria parasites, P. falciparum is the most highly pathogenic and
responsible for malignant tertian malaria. This is a form of disease which runs
an acute course in non- immune patients and is frequently fatal if untreated.
Life Cycle
The
malaria parasite passes its life cycle in two different hosts and comprises of
two phase as follows,
Definitive host: Female Anopheles mosquito (a
sexual phase of parasite occurs).
Intermediatehost: Human (an
asexual phase of parasite occurs).
Thus,
life cycle of malaria parasite show alternation of generations- asexual and
sexual generation in two different hosts (Figure 8.12).
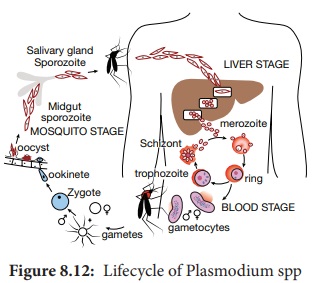
Human Cycle (Asexual Phase ŌĆō Schizogony)
Human infection occurs when the sporozoites (the
infective forms of the parasite are present in the salivary gland of the
mosquito) are injected into blood capillaries when the mosquito feeds on blood
after piercing the skin. The malarial parasite multiplies by division and the
process designated as Schizogony (schizo: to split, gone: generation).
Sporozoites are minute thread-like curved organisms with tapering ends. Measuring 9ŌĆō12┬Ą in length with a central elongated nucleus while, the cytoplasm reveals no pigment as seen with a light microscope. In human, schizogony occurs in two locations. One in the red blood cells (erythrocytic schizogony) and other in the liver cells (pre ŌĆō or exoerythrocytic schizogony).
A. PreŌĆōerythrocytic or Exoerythrocytic schigony
ŌĆó Sporozoits do not directly enter the RBCŌĆÖs to itiate
erythrocytic schizogony, but undergo developmental phase in other human
tissues.
ŌĆó This cycle lasts for about 8 days in Plasmodium
vivax, 6 days in P. falciparum and 9 days in P. ovale This preŌĆōerythrocytic
schizogony occurs within parenchymal cells of the liver.
ŌĆó The Sporozoites, which are elongated spindle ŌĆō
shaped bodies, become rounded inside the liver cells.
ŌĆó They enlarge in size and undergo repeated nuclear
division to form several daughter nuclei, each of which is surrounded by
cytoplasm.
ŌĆó This stage of the parasite is called the
preŌĆōerythrocytic or exoerthrocytic schizont or merozoites.
ŌĆó The
heptocyte is distended by the enlarging schizont and the liver cell nucleus is
pushed to the periphery.
ŌĆó Mature
liver stage schizonts are spherical multinucleate and contain 2000ŌĆō50,000
uninucleate merozoites
ŌĆó These
normally rupture in 6ŌĆō15 days and release thousands of merozoites into the
blood stream.
ŌĆó They do
not return from red blood cells to liver cells.
Plasmodium
vivax and P. ovale ŌĆō parasites in liver tissue are called
hypnozoites.
B. Erythrocyticstage
ŌĆó The merozoites released by preŌĆōerythrocytic
schizonts invade the red blood cells (Parasitaemia).
ŌĆó Merozoites
are pear ŌĆō shaped bodies, about 1.5 ┬Ąm in length.
ŌĆó In the
erythrocyte, the merozoite loses its internal organelles and appears as rounded
body having a vacuole in the center with the cytoplasm pushed to the periphery
and the nucleus at one pole. These forms are called ring forms or young
trophozoites.
ŌĆó The
parasite feeds on the hemoglobin of the erythrocyte. They incompletely
metabolize hemoglobin therefore, hematin ŌĆō globin pigment or haemozoin pigment
is left behind.
ŌĆó The
malaria pigment released when the parasitized cells rupture is taken up by
recticuloendothelial cells.
ŌĆó The ring form develops and becomes irregular in
shape and shows amoeboid motility. This is called the amoeboid form.
ŌĆó When the amoeboid form reaches a certain stage of
development, its nucleus starts dividing by mitosis followed by a division of
cytoplasm to become mature schizonts or merozoites.
ŌĆó A mature schizont contains 8ŌĆō32 merozoites and
haemozoin. The mature schizont bursts releasing the merozoites into the
circulation.
ŌĆó The merozoites invade fresh erythrocytes within which
they go through the same process of development. This cycle is called
erythrocytic schizogony.
ŌĆó The rupture of the mature schizont releases large
quantities of pyrogens. This is responsible for the febrile paroxysms
characterising malaria.
ŌĆó In P. falciparum, erythrocytic schizog-ony
always takes place inside the cap-illaries and vascular regions of internal
organs. Therefore, in these infections, schizonts and merozoites are usually
not seen in the peripheral blood.
C. Gametogony
ŌĆó Some of the merozoites, after a few erythrocytic
cycles do not develop into trophozoites and schizonts but they undergo sexual
differentiation to develop into the gametocytes.
ŌĆó Development of gametocytes takes place within the
internal organs and only the mature forms appear in circulation.
ŌĆó The mature gametocytes inP. falciparum are crescent shaped.
ŌĆó Female gametocytes are generally more numerous
and larger.
ŌĆó Male gametocytes and female gametocytes are
called micro gametocytes and macro gametocytes respectively.
ŌĆó Gametocyte
appears in 10ŌĆō12 days in P. falciparum.
The gametocytes do not cause any clinical illness in the host, but are
essential for transmission of the infection.
ŌĆó A
person who harbors the gametocytes is referred to as a carrier or reservoir.
Infobits
Sir Ronald Ross Institute of Parasitology is a malaria research
institute located in Begumpet, Secunderabad, Hyderabad, India. Established in
1955, the institute is a division of Osmania University. The institute is named
after Sir Ronald Ross, winner of Nobel Prize for Physiology or Medicine, 1902.
Though he was a surgeon by qualification, Ross was attracted towards research
in tropical diseases, especially malaria. During his posting, he worked on his
research from a laboratory in the old Begumpet military hospital building. It
was in this building on 20 August 1897 that he made the discovery of the malarial
parasite inside the body of a mosquito.His study confirmed that mosquitoes were
the carriers of malaria parasite.
Mosquito Cycle (Sexual Cycle ŌĆō Sporogony)
ŌĆó A
Female Anopheles mosquito during its blood ŌĆō meal from an infected person,
sucks up both the sexual and asexual forms of parasite. But, only the mature
sexual forms develop and the rest die.
ŌĆó The gametocytes are set free in the midgut
(stomach) of mosquito and undergo further development
ŌĆó The nuclear material and cytoplasm of the male
gametocyte divides to produce long, actively motile, whip ŌĆō like forms of 8
microgametes. This process is called exflagellation of male gametocytes.
ŌĆó The Exflagellation is completed within 15ŌĆō30
minutes for P. falciparum.
ŌĆó The female gametocyte does not divide but
maturation involves by condensation of nucleus to become the female gamete.
ŌĆó Female gamete is fertilized by one of the
microgametes to produce the zygote. The zygote is formed in 20ŌĆō120 minutes
after the blood meal. The zygote is initially is a non ŌĆō motile round body, but
within 18ŌĆō24 hours, it gradually elongates into a vermicular motile form. This
is called the ookinete.
ŌĆó Ookinete penetrates the epithelial lining of
stomach wall. Their anterior end comes in close contact to the cell membrane by
secretion of some proteolytic substances which causes lysis of cell membrane.
Later, the ookinete come to lie just beneath the basement membrane.
ŌĆó It becomes rounded into a sphere with an elastic
membrane. This stage is called the oocyst. The oocyst increase in size and
undergo numerous nuclear multiplication which develops a large number of sickle
shaped bodies known as sporozoites.
ŌĆó Number of oocysts in the stomach wall varies from
a few to over a hundred
ŌĆó Around the 10th day of infection the oocyst ruptures,
releasing sporozoites in the body cavity of the mosquitos.
ŌĆó Around
the 10th day of infection the oocyst ruptures, releasing sporozoites in the
body cavity of the mosquitos
ŌĆó The
sporozoites are distributed through the circulating fluid into various organs
and tissues of the mosquito except the ovaries.
ŌĆó The
sporozoites have a special affinity towards the salivary glands. The mosquito
at this stage is capable of transmitting infection to man.
Pathogenesis
In
malaria, typical pathological changes are seen primarily in the spleen, liver,
bone marrow, lungs, kidney and brain.
Liver: The liver is enlarged. The organ becomes more firm and pigmented.
Pigments are found in parenchymal cells.
Spleen: The spleen is markedly enlarged. If the infection lasts over a long period, the spleen is
usually grayish, dark brown or even black and is commonly known as ŌĆśague cakeŌĆÖ
Bone
marrow, Lungs, Kidneys and Brain are enlarged and pigmented. They are filled
with parasitized erythrocytes. Anemia is caused by destruction of large number
of red cells by complement mediated and autoimmune hemolysis. It is also due to
the increased clearance of both parasites and parasitized RBCs by the spleen.
Clinical Manifestations
The
incubation period is generally 9ŌĆō14 days but, it can be as short as 7 days. The
most malignant form of malaria is caused by P. falciparum hence, variable clinical syndromes are associated with
falciparum malaria. That include,
1. Prodromal
(initial indication of the onset of disease) period: Non ŌĆō specific symptoms
such as malaise (condition of general weakness or discomfort), myalgia (severe
muscle pain) headache and fatigue (feeling of tiredness) are usually seen
during the prodromal period.
2. Malarial paroxysm (sudden onset of disease): It
is the classical manifestation of acute malaria. It is characterised by fever,
chill and rigor (sudden feelings of cold with shivering).The fever is caused by
rupture of red blood cells that contain malarial parasites. The fever occurs
every 48 hours in falciparum malaria.
3. Anemia (A condition in which the blood does not
have enough healthy Red Blood cells) and
4. Hepatosplenomegaly (simultaneously enlargement
of both the liver and the spleen)
The
symptoms are non ŌĆō specific with headache, pains in back and limbs, anorexia,
nausea and a feeling of chill rather than a distinct cold phase. Hyponatremia
(A condition that occurs when the level of Sodium in the blood is too low)
occur in both uncomplicated and severe malaria.
Infobits
Transfusion Malaria
Malaria can be transmitted by transfusion of blood from infected
donors. First reported in 1911, transfusion malaria is one of the most common
transfusion -transmitted infections today. Blood transfusion can accidentally
transmit malaria, if the donor is infected with malaria. The parasites may
remain viable in blood bank for 1ŌĆō2 weeks. As this condition is induced by
direct infection of red cells by the merozoites. Pre-erythrocytic schizogony
and hypnozoites are absent.
Complications of Severe Falciparum Malaria
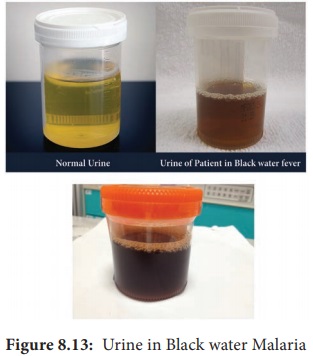
1. Black water fever
The
syndrome is the manifestation of repeated infections of falciparum malaria,
which were inadequately treated with quinine. The condition is associated with
haemoglobinaemia (excess of hemoglobin in the blood plasma) and haemoglobinuria
(excretion of free haemoglobin in the urine). The syndrome is known as black
water fever due to the dark red to brown ŌĆō black appearance of the urine in
this condition (Figure 8.13). It is dark due to presence of free haemoglobin as
methaemoglobin or oxyhaemoglobin in it. Kidney failure is the immediate cause
of death.
2. Cerebral malaria
Cerebral
malaria is the most common presentation of severe malaria in adult. Cerebral
malaria may be sudden in onset. Clinically, the condition manifests with fever
for 4ŌĆō5 days, slowly lapsing into coma, with or without convulsions. It is
marked by a severe headache, high fever even above 180┬░F, and changes in mental
status. Death may occur within few hours. Algid malaria and septicemic malaria
are also other serious complication of falciparum malaria.
3. Pernicious malaria
The term
pernicious malaria is referred to as a series of phenomena that occur during
the course of an in treated P. falciparum
infection within 1 to 3 days.
4. Anaemia: An individual suffering from an attack of malaria, after a few paroxysms becomes temporarily anaemic. The reduction in red blood cells is greater in P. falciparum infection than in infection with P. vivax and P. malariae. This is because P. falciparum invades young and mature erythrocytes and the infection rate of red blood cells is also greater.
HOTS: Which stage is infective in Blood transfusion malaria?
Recrudescence
In P. falciparum and P. malariae infections after the primary attack, sometimes there is
a period of latency, during which there is no clinical illness. But some
parasites persist in some erythrocytes and gradually increase in numbers. Fresh
malarial attacks then develop. It appears after a period of latency usually
within weeks after the primary attacks. Persistence of the erythrocytic cycle
of the parasites are called recrudescences. In P. falciparum infections, recrudescences are seen for 1ŌĆō2 years,
while in P. malariae infection, they
may last for long periods, even upto 50 years.
Infobits
The global technical strategy for malaria 2016-2030 was adopted
by the World health Assembly in May 2015. It provides a comprehensive framework
to guide countries in their efforts to accelerate progress towards malaria
elimination. The strategy sets the target of reducing global malaria incidence
and mortality rates by at least 90% by 2030.
Plasmodium vivax
P. vivax shows a similar life cycle in humans and mosquitoes like that of P. falciparum. Except in P. vivax, a latent tissue stage, the hypnozoites present in the liver parenchyma.
Relapse
in vivax malaria is caused by these hypnozoites. Hypnozoites are the dormant
stages of the parasites. These are single ŌĆō nucleated parasites measuring
4┬ĄmŌĆō6┬Ąm in diameter. These become active and develop into tissue schizonts
after a short period of dormancy. This relapse may occur at intervals up to 3
years or more after the first attack. P.
vivax merozoites invade only young erythrocytes
and the reticulocytes.
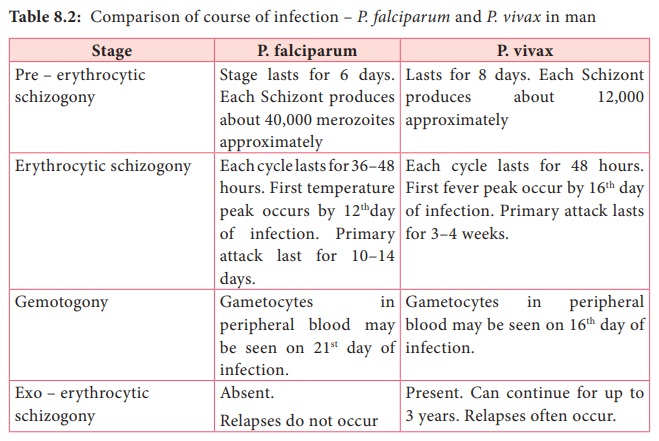
Clinical Manifestations
P. vivax is the most wide spread species causing malaria in man. However, unlike Falicparum malariya is
less sever and death from the condition relatively is less common table 8.2
describes the comparison of course of infection in falciparum malariya with
vivax malaria
laboratory Diagnosis
Diagnosis of malariya includes;
a. Parasitic diagnosis
b. Serodiagnisis and
c. Molecular diagnosis
Parasitic diagnosis ŌĆō Demonstration of parasite by
microscopy
Specimen: Blood
Conventional
light microscopy of stained blood smear is the gold standard for confirmation
of malaria.
Two types
of smears are prepared from the peripheral blood. They are thin and thick
smears (Figure 8.14). Ring forms and gametocytes are most commonly seen in the
peripheral blood smear.
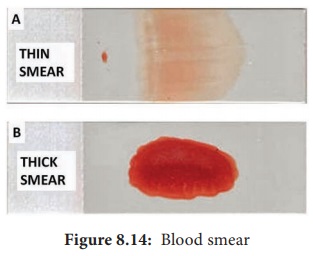
Thin smear
They are
prepared from capillary blood of fingertip and spread over a good quality slide
by a second slide (spreader slide) held at an angle of 30┬░ŌĆō45┬░ from the
horizontal such that a tail is formed
Thin
smears thus prepared are air dried, fixed in alcohol and stained by one of the
Romanowsky stains such as Leishman, Giemsa or JSB (Jaswant singh and
Bhattacharjee) stain.
Thin
smears are used for:
a. Detecting
parasites, and
b. For
determining the species of the infecting parasite.
Thick smear
They are
prepared usually with 3 drops of blood spread over a small area of about 10mm.
The thick film is dried. This smears consist of a thick layer of
dehemoglobinized (lysed) red blood cells. It is not fixed in methanol.
Thick
film is stained similar to thin film. Thick smears have the advantage of
concentrating the parasites and therefore increase the sensitivity of
diagnosis. Thick smears are used for
a. Defecting
parasites,
b.
Quantitating parasitaemia, an
c.
Demonstrating malarial pigments.
Fluoroscence microscopy
The
method is mainly used for mass screening in field laboratory. Fluorescent dyes
like acridine orange is used to stain the blood smears. It stains DNA as
fluorescent green and cytoplasmic RNA as red.
QBC (Quantitative Buffy coat smear)
This is a
sensitive method for detection of malaria parasites. In this method, blood is
collected in a capillary tube coated with fluorescent dye and is subjected to
centrifugation. After centrifugation, the Buffy coat in the centrifuged
capillary tubes is examined under a fluorescent microscope. Acridine orange ŌĆō
stained malaria parasites appear brilliant green.
Serodiagnosis
It is not
helpful in clinical diagnosis. It is used mainly for epidemiological survey and
to identify the infected donors in transfusion malaria. The test used are
indirect haemagglutination (IHA), Indirect fluorescent antibody (IFA) and
Enzyme ŌĆō linked immunosorbent assay (ELISA) for the detection of serum
antibodies.
Rapid
Antigen detection tests kits are available commercially like the dipstick, card
and cassette bearing monoclonal antibody. These tests are based on the
detection of antigens using immune chromatographic methods. These tests can
detect plasmodium in 15 minutes.
Molecular diagnosis
DNA probe
and PCR are highly sensitive methods for the diagnosis of malaria. It is more
sensitive than that of thick blood smear. It is highly species specific.
Other
tests includes the measurement of hemoglobin, total WBC and platelet count in
severe falciparum malaria, urine can be tested for free hemoglobin, if black
water fever is suspected. Blood urea and serum creatinine has to be monitored
for renal failure.
Treatment
The most
commonly used drugs are Chloroquine, Quinine, Pyrimethamine and Doxycycline.
Prevention and Control
The
preventive measures to control malaria mainly depend on treatment of infected
individuals and reducing the transmission of malaria.
The
control measures include the use of insecticides such as DDT (Di chlorodiphenyl
tri chloromethane) or Malathion for controlling the populations of adult
mosquitoes.
Proper
use of mosquito nets, wearing protective clothings and use of mosquito
repellants can prevent the mosquito bite.
Introduction to Helminths
General
characteristics of Helminthic parasite:
1. Helminths are multicellular worms. They are
bilaterally symmetrical animals having 3 germ layers and belong to the kingdom
Metazoa.
2. They are invertebrates characterised by
elongated, flat or round bodies.
3. Helminths
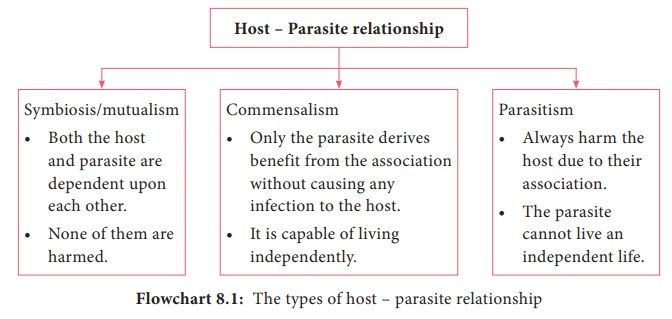
develop through egg, larval and adult stages. Flowchart 8.1 describes the
classification of helminthes.
Related Topics