Chapter: Obstetrics and Gynecology: Common Medical Problems in Pregnancy
Thyroid Disease during pregnancy
THYROID DISEASE
As with diabetes mellitus,
thyroid disease may predate pregnancy or may initially manifest during
pregnancy. Obstetric conditions, such as gestational trophoblastic disease or hyperemesis
gravidarum, may themselves affect thyroid function. All neonates of women with
thyroid dis-ease are at risk for neonatal thyroid dysfunction. For this reason,
the neonate’s pediatrician should be informed about the maternal diagnosis.
Pathophysiology
Thyrotoxicosis
is the condition that results from excessproduction
of and exposure to thyroid hormone from any cause. Hyperthyroidism is thyrotoxicosis caused by hyper-functioning of
the thyroid gland. Graves disease is an auto-immune disease characterized by
abnormal production of thyroid-specific immunoglobulins that either stimulate
or inhibit thyroid function. Exacerbation of the signs and symptoms of
hyperthyroidism is called a thyroid
storm.Hypothyroidism is caused by inadequate thyroid hormoneproduction. Postpartum thyroiditis is an autoimmune
inflammation of the thyroid gland that presents as new-onset, painless
hypothyroidism, transient thyrotoxicosis, or thyrotoxicosis followed by
hypothyroidism within 1 year postpartum.
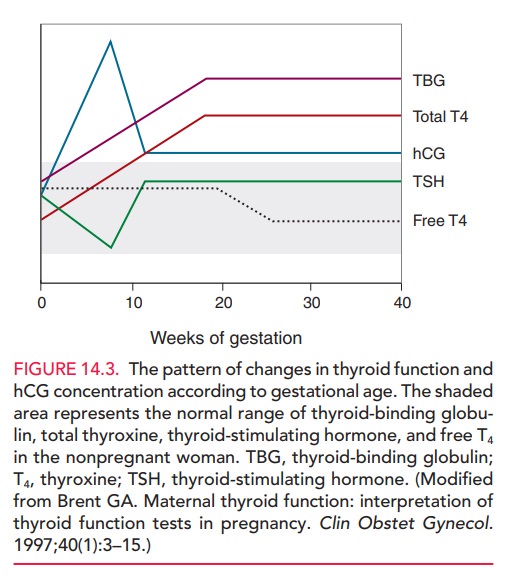
Levels of thyroid-binding hormone
(TBG) normally increase in pregnancy. Test results that change significantly in
pregnancy are those influenced by TBG concentra-tion, including total thyroxine
(TT4), total triiodothy-ronine (TTd) and resin triiodothyronine uptake (TR3U). A
transient increase may also occur in free thyroxine (FT4) and free thyroxine
index (FTI) levels in the first trimester (Fig. 14.3).
Plasma iodide levels decrease
during pregnancy, and this change may cause a noticeable increase in thyroid
gland size (approximately 18% change) in 15% of women. How-ever, in most women,
the thyroid returns to normal size postpartum.
Laboratory Screening
There is
insufficient evidence to warrant routine screening of asymptomatic pregnant
women for hypothyroidism.
Testing should be performed in women with a prior his-tory of thyroid disease or symptoms of thyroid disease. Thyroid function is evaluated by measuring thyroid-stimulating hormone (TSH) levels. TSH does not cross the placenta, so this test is an accurate measure of hor-mone function during pregnancy. In pregnant women suspected of being hyperthyroid or hypothyroid, FT4 and FTI levels should be measured in addition to TSH.
Management of Existing Thyroid Disease in Pregnancy
Hyperthyroidism in pregnancy is
treated with thioamides, specifically propylthiouracil (PTU) and methimazole. Thegoal of treatment during pregnancy is to
maintain the FT4 or FTI in the high normal range using the lowest possible
dosage of thioamides to minimize fetal exposure. Thioamide treat-ment for
Graves disease in pregnancy may suppress fetal and neonatal thyroid function
and has also been associated with fetal goiter. Neonatal hypothyroidism is
usually tran-sient and does not require treatment.
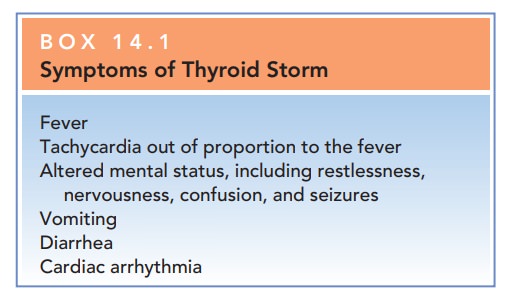
Thyroid
storm is a medical emergency characterized by an extreme hypermetabolic state.
Although rare (it occurs in 1% of pregnancy patients with hyperthyroidism), it
carries a high risk of maternal heart failure. It is
often precipitated by infection,surgery, labor, or delivery. Thyroid storm must
be diag-nosed and treated quickly in order to prevent shock, stupor, and coma
(Box 14.1). Treatment of thyroid storm consists of a standard series of drugs,
each of which plays a role in suppressing thyroid function. The underlying
precipitating event should also be treated. The fetus should be appropri-ately
evaluated with ultrasonography, biophysical profile, or nonstress test,
depending on the gestational age.
Treatment
of hypothyroidism in pregnant women is the same as for nonpregnant women and
involves administration of levothy-roxine at sufficient dosages to normalize
TSH levels. Maternalthyroxine requirements increase in women
with hypothy-roidism diagnosed before pregnancy. Levothyroxine levels should be
adjusted at 4-week intervals until TSH levels are stable. Thereafter, levels
should be checked once per trimester.
Management of Thyroid Disease Diagnosed During and After Pregnancy
Severe nausea and vomiting of pregnancy (hyperemesisgravidarum) may cause biochemical hyperthyroidism, inwhich levels of TSH are undetectable, or FTI levels are elevated, or both. This condition resolves spontaneously by 18 weeks of gestation. Routine measurements of thyroid function are not recommended in patients with hyperemesis gravidarum unless other overt signs of hyperthyroidism are evident.
Postpartum
thyroiditis occurs in 5% of women who have no prior history of thyroid disease.
Postpartum thyroiditisalso may occur after
pregnancy loss and has a 70% risk of recurrence. Almost half of women with
postpartum thyroiditis have hypothyroidism, while the remaining women are
evenly split between thyrotoxicosis and thyro-toxicosis followed by hypothyroidism.
Postpartum thyro-toxicosis usually resolves on its own without treatment. Of
those with hypothyroidism, approximately 40% of women require treatment for
extremely high TSH levels or an increasing goiter size. Only 11% of women
diag-nosed with postpartum hypothyroidism develop perma-nent hypothyroidism.
Related Topics