Chapter: Obstetrics and Gynecology: Common Medical Problems in Pregnancy
Asthma during pregnancy
ASTHMA
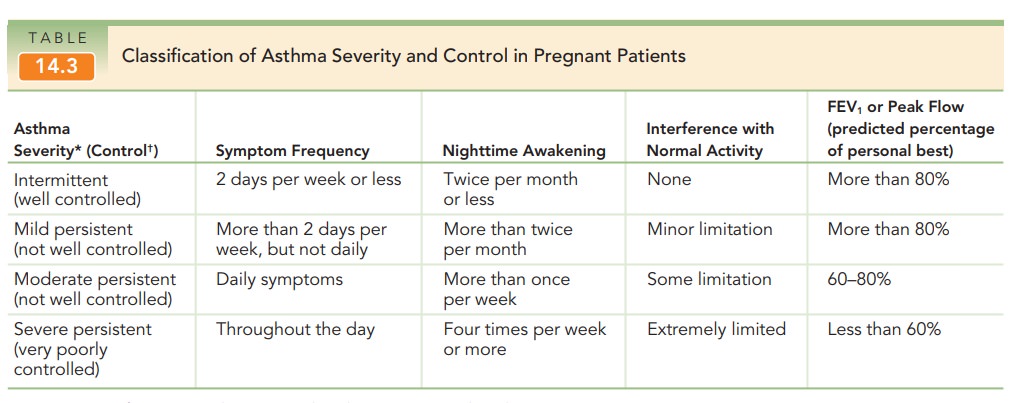
Asthma is a restrictive-airways disease that is encounteredin approximately 4% to 8% of pregnant patients. The effectsof pregnancy on asthma are variable—in general, about one third of patients worsen, one third improve, and the remaining one third are unchanged. Women with mild or moderateasthma usually have excellent maternal and fetal outcomes (Table 14.3). However, suboptimal control of asthma dur-ing pregnancy may be associated with increased maternal or fetal risk. Decreased FEV1 (forced expiratory volume in the first second of expiration) is associated with increased risk of low birth weight and prematurity.
Pregnant
patients with asthma, even those with mild or well-controlled disease, should
be monitored with PEFR or FEV1 testing as well as by close symptom
observation.
Routine evaluation of pulmonary
function in pregnant women with persistent asthma is recommended. Serial
ultrasound examinations and antenatal fetal testing should be considered for
women who have moderate or severe asthma during pregnancy beginning at 32 weeks
of ges-tation or for women recovering from a severe asthma exacerbation
The
ultimate goal of asthma therapy in pregnancy is main-taining adequate
oxygenation of the fetus by preventing hypoxic episodes in the mother. Inhaled
corticosteroid therapy, par-ticularly budesonide, is the first-line controller
treatment for persistent asthma during pregnancy. Inhaled albuterol is the
recommended rescue therapy. In thestep-care ther-apeutic approach, the
number and dosage of medications areincreased with increasing asthma severity. Once
control ofsymptoms is achieved, a “step-down” approach is usually implemented
in the nonpregnant patient. In pregnant pa-tients, it may be prudent to
postpone a reduction in a ther-apy that is effectively controlling a patient’s
asthma until after the birth. Patients should be instructed to identify and control
or avoid factors, such as allergens and irritants, par-ticular tobacco smoke.
Management of a severely
asthmatic pregnant patient is similar to that of a nonpregnant patient.
Evaluation con-sists of measurement of pulmonary function and arterial blood
gases. Treatment may include administration of sup-plemental oxygen, treatment
with nebulized β-agonists,
corticosteroids (oral or intravenous), or intubation. Women who are currently receiving or recently have taken systemic
corticosteroids should receive intravenous administration of corticosteroids
during labor and for 24 hours after delivery to prevent adrenal crisis.
Related Topics