Chapter: Obstetrics and Gynecology: Common Medical Problems in Pregnancy
Fetal Morbidity and Mortality in Pregestational and Gestational Diabetes
Fetal Morbidity and Mortality in Pregestational and Gestational
Diabetes
Infants
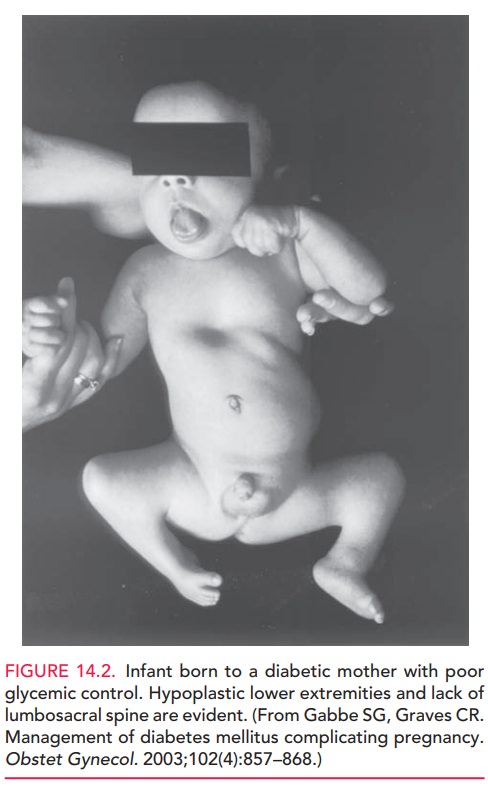
of mothers with diabetes are at a six-fold increased risk of congenital
anomalies over the 1% to 2% baseline risk of all patients. The most
commonly encountered anomalies arecardiac and limb deformities. Sacral agenesis is a unique but rare
anomaly for this group (Fig. 14.2).
The risk of spontaneous abortion is similar in patients with well-controlled diabetes and in patients without dia-betes, but the risk is significantly increased for the patients with diabetes if glucose control is poor.
There is also an in-creased risk
of intrauterine fetal demise and stillbirth, especially when diabetic control
is inadequate. Because of this potentiallydevastating outcome, beginning at
approximately 30 to 32 weeks of gestation, various antepartum fetal tests may
be initiated to monitor fetal health (see “Antepartum Fetal Monitoring”
sections below).
Infections occur more frequently
in mothers with diabetes. The glucose-rich urine is an excellent environ-ment
for bacterial growth; the risk of urinary tract infec-tion (UTI) and
pyelonephritis is approximately double that of nondiabetic pregnant patients.
Patients should be told to promptly report any symptoms that suggest infection
so that identification and treatment can be initiated.
Excessive
fetal growth, or macrosomia (usually
defined as a fetal weight in excess of either 4000 or 4500 g), is more common
in pregnant patients with diabetes because of the fetal metabolic effects of
increased glucose transfer across the placenta. However,
intrauterine growth restriction can also occur due to uteroplacental
insufficiency. For these reasons, serial ultrasonography is often performed to
follow fetal growth. When the estimated fetal weight by ultrasound late in
pregnancy is greater than 4500 g, cesarean delivery is often recommended to
avoid the risk of fetopelvic dis-proportion, shoulder dystocia, and other birth
trauma as-sociated with large infants.
Another
complication of pregnancy in patients with dia-betes is an increase in amniotic
fluid volume greater than 2000 mL, a condition known as hydramnios or polyhydram-nios. Encountered
in approximately 10% of mothers withdiabetes, the increases in amniotic fluid
volume and uter-ine size are associated with an increased risk of placental
abruption and preterm labor, as well as postpartum uter-ine atony. This
condition is monitored while serial ultra-sonography is performed for fetal
growth, at which time the amount of amniotic fluid can be evaluated.
Neonatal
hypoglycemia is often encountered in in-fants of women with
diabetes. It results from the sudden change in the maternal-fetal glucose
balance, in which an increased maternal glucose crossing the placenta is coun-tered
by an increase in fetal production of insulin. However, when the maternal
supply of glucose is removed, this higher level of insulin can cause
significant neonatal hypoglycemia. In addition, these newborns are subject to
an increased incidence of neonatal hyperbilirubinemia, hypocalcemia, and
polycythemia.
Infants of mothers with diabetes
also tend to have an increased frequency of respiratory distress syndrome. The
usual tests of lung maturity may be less predictive for these infants (see
respiratory - next section ).
Related Topics