Chapter: Obstetrics and Gynecology: Common Medical Problems in Pregnancy
Hematologic Disease: Anemia
HEMATOLOGIC DISEASE
Anemia
The plasma and cellular
composition of blood change sig-nificantly during pregnancy, with the expansion
of plasma volume proportionally greater than that of the red blood cell mass.
On average, there is a 1000-mL increase in plasma volume and a 300-mL increase
in red-cell volume (a 3:1 ratio). Because the hematocrit (Hct) reflects the
pro-portion of blood made up primarily of red blood cells, Hct demonstrates a
“physiologic” decrease during pregnancy; therefore, this decrease is not
actually an anemia.
Anemia in
pregnancy is generally defined as an Hct less than 30% or a hemoglobin of less
than 10 g/dL.
The direct fetal consequences of
anemia are minimal, although infants born to mothers with iron deficiency may
have diminished iron stores as neonates. The maternal consequences of anemia
are those associated with any adult anemia. If anemia is corrected, the woman
with an ade-quate red-cell mass enters labor and delivery better able to
respond to acute peripartum blood loss and to avoid the risks of blood or blood
product transfusion.
IRON-DEFICIENCY ANEMIA
Iron-deficiency
anemia is by far the most frequent type ofanemia seen in
pregnancy, accounting for more than 90% of cases. Because the iron content of
the standard American diet and the endogenous iron stores of many American
women are not sufficient to provide for the increased iron requirements of
pregnancy, the National Academy of Sciences recommends 27 mg of iron
supplementation (present in most prenatal vitamins) daily for pregnant women.
Most prescription prenatal vitamin/mineral prepa-rations contain 60 to 65 mg of
elemental iron.
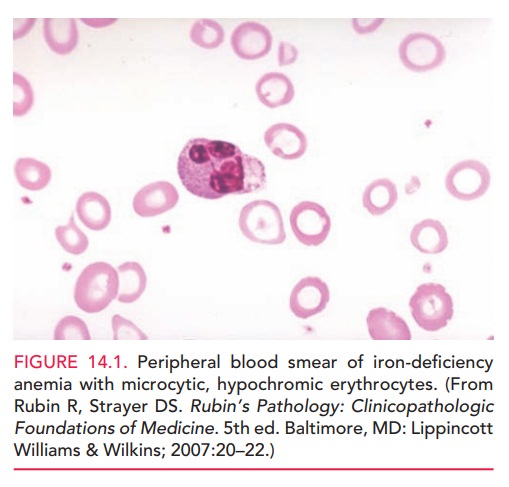
All pregnant women should be
screened for iron-deficiency anemia. Severe iron-deficiency anemia is
charac-terized by small, pale erythrocytes (Fig. 14.1) and red-cell indices
that indicate a low mean corpuscular volume and low mean corpuscular hemoglobin
concentration. Addi-tional laboratory studies usually demonstrate decreased
serum iron levels, an increased total iron-binding capacity, and a decrease in
serum ferritin levels. A recent dietary history is obviously important,
especially if pica (the con-sumption of non-nutrient substances such as starch,
ice, or dirt) exists. Such dietary compulsions may contribute to iron
deficiency by decreasing the amount of nutritious food and iron consumed.
Treatment of iron-deficiency
anemia generally requires an additional 60 to 120 mg of elemental iron per day,
in ad-dition to the iron in the prenatal vitamin/mineral prepa-ration. Iron
absorption is facilitated by or with vitamin C supplementation or ingestion
between meals or at bed-time on an empty stomach. The response to therapy is
first seen as an increase in the reticulocyte count approximately 1 week after
starting iron therapy. Because of the plasma expansion associated with
pregnancy, the Hct may not increase significantly, but rather stabilizes or
increases only slightly.
FOLATE DEFICIENCY
Adequate intake of folic acid (folate) has been found to reduce the risk of neural tube defects (NTDs) in the fetus
The first occurrence of NTDs may
be reduced by as much as 36% if women of reproductive age consume 0.4 mg of
folate daily both before conception and during the first trimester of
pregnancy. The Recommended Daily Dietary Allowance for folate for pregnant
women is 0.6 mg. Folate deficiency is especially likely in multiple gestations
or when patients are taking anticonvulsive medications. Women with a history of
a prior NTD-affected pregnancy or who are being treated with anticonvulsive
drugs may reduce the risk of NTDs by more than 80% with daily intake of 4 mg of
folate in the months in which conception is attempted and for the first
trimester of pregnancy.
Folate is found in green leafy vegetables and is now an added supplement in cereal, bread, and grain prod-ucts. These supplements are designed to enable women to easily consume 0.4 mg to 1 mg of folate daily. Prescription prenatal vitamin/mineral preparations contain 1 mg of folic acid.
OTHER ANEMIAS
The hemoglobinopathies are a heterogenous group of single-gene
disorders that includes the structural hemoglo-bin variants and the
thalassemias. Hereditary
hemolyticanemias are also rare causes of anemia in pregnancy.Some examples
are hereditary spherocytosis, an autosomal dominant defect of the erythrocyte
membrane; glucose 6-phosphate dehydrogenase deficiency; and pyruvate kinase
deficiency.
Related Topics