Chapter: Ophthalmology: Ocular Motility and Strabismus
Therapy of Concomitant Strabismus
Therapy of Concomitant Strabismus
Therapy of concomitant strabismus in children:
Treatment is generallylong-term. The duration
of treatment may extend from the first months of life to about the age of
twelve. Specific treatments and therapeutic success are determined not only by
the clinical course but also by the child’s overall per-sonality and the
parents’ ability to cooperate. The entire course of treatment may be divided
into three phases with corresponding
interim goals.
1.
The ophthalmologist determines whether the cause of the
strabismus may be treated with eyeglasses (such as hyperopia).
2. If the strabismus cannot be fully corrected
with eyeglasses, the next step in treatment (parallel to prescribing
eyeglasses) is to minimize the risk of amblyopia by occlusion therapy.
3. Once the occlusion therapy has produced sufficient visual acuity in both eyes, the alignment of one or both eyes is corrected by surgery. Late stra-bismus with normal sensory development is an exception to this rule (for further information, see Surgery). The alignment correction is required for normal binocular vision and has the added benefit of cosmetic improvement.
Therapy of concomitant strabismus in adults:
The only purpose of surgeryis cosmetic
improvement. A functional improvement in binocular vision can no longer be
achieved.
Eyeglass Prescription
Where the strabismus is due to a cause that
can be treated with eyeglasses, then eyeglasses can eliminate at least the
accommodative component of the disorder. Often residual strabismus requiring
further treatment will remain despite eyeglass correction.
Treatment and Avoidance of Strabismic Amblyopia
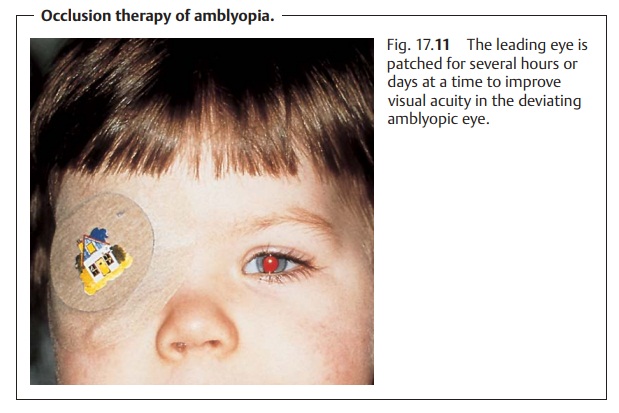
Strict occlusion therapy by eye patching or eyeglass occlusion is the most effective method of avoiding or treating strabismic amblyopia. Primarily theleading eye is patched.
Eye patching:
Severe amblyopia with eccentric fixation requires an eye
patch(Fig. 17.11). Eyeglass
occlusion (see next section) entails the risk that the child might attempt to
circumvent the occlusion of the good eye by looking over the rim of the
eyeglasses with the leading eye. This would compromise the effectiveness of
occlusion therapy, whose purpose is to train the amblyopic eye.

Eyeglass occlusion:
Mild cases of amblyopia usually may be treated success-fully by
covering the eyeglass lens of the leading eye with an opaque material. In such
cases, the child usually does not attempt to look over the rim of the
eyeglasses because the deviating eye has sufficient visual acuity.
Procedure:
The duration of occlusion therapy must be balanced so as to
avoida loss of visual acuity in the leading eye. The leading eye is occluded
for several hours at a time in mild
amblyopia, and for several days at a time in severe amblyopia depending to
the patient’s age. For example, the nondeviat-ing eye in a four-year-old patient is patched for four days while the deviating eye is
left uncovered. Both eyes are then left uncovered for one day. This treat-ment
cycle is repeated beginning on the following day.
Amblyopia must be treated in early childhood.
The younger the child is, the more favorable and rapid the response to treatment
will be. The upper age limit for occlusion therapy is approximately the age of
nine. The earlier therapy is initiated, the sooner amblyopia can be eliminated.
The goal of treatment in infantile strabismus is to achievealternating stra-bismus with
full visual acuity and central
fixation in both eyes. Binocularvision is less important in this setting.
It is not normally developed anyway in patients who develop strabismus at an
early age and cannot be further improved.
Surgery
Surgery in infantile strabismus syndrome:
Surgery should be postponeduntil after
amblyopia has been successfully treated (see previous section). It is also
advisable to wait until the patient has reached a certain age. Adequate
follow-up includes precise measurement of visual acuity at regular intervals in
tests that require the patient’s cooperation, and such cooperation is
diffi-cult to ensure in young patients below the age of four. Surgical
correction in a very young patient prior to successful treatment of amblyopia
involves a risk that a decrease in visual acuity in one eye may go unnoticed
after the stra-bismus has been corrected. However, the child should undergo
surgery prior to entering school so as to avoid the social stigma of
strabismus. In such a case, surgery achieves only a cosmetic correction of strabismus.
Surgery in late strabismus with normal sensory development:
In thiscase, surgery should be performed as
early as possible because the primary goal is to preserve binocular vision,
which is necessarily absent in infantile strabismus syndrome.
Procedure:
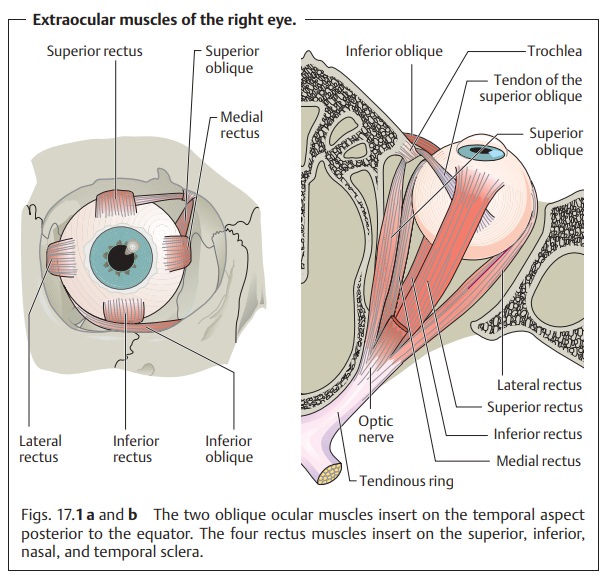
The effect of surgery is less to alter the pull of the
extraocularmuscles than to alter the position of the eyes at rest. Esotropia is corrected by a combined
procedure involving a medial rectus recession and a lateral rectus resection.
The medial rectus is released because its pull is “too strong” (see Fig. 17.1), whereas the lateral rectus is
shorted to increase its pull. The degree of correction depends on the angle of
deviation. Primary oblique muscle
dys-function is corrected by inferior oblique recession and if necessary by
dou-bling the superior oblique to reinforce it. Exotropia is corrected by posteriorly a lateral rectus recession in
combination with a medial rectus resection.
Related Topics