Chapter: Ophthalmology: Ocular Motility and Strabismus
Concomitant Strabismus
Concomitant Strabismus
Definition
Concomitant strabismus differs from paralytic
strabismus in that the angle of deviation remains the same in every direction
of gaze. The deviating eye fol-lows the normal fellow eye at a constant angle.
Epidemiology:
Concomitant strabismus occurs almost exclusively inchildren.
Approximately 5.3 – 7.4% of all children are affected. In 60 – 70% of all
cases, the disorder initially manifests itself within the first two years of
life.
Etiology:
Vision at birth is neither focused nor binocular, and both
sen-sorimotor coordination and binocular vision are very unstable during the
first few years of life. Impairments of
the sensory or motor systems or central pro-cessing of visual perceptions that
occur during this time can disturb thecoordination between the eyes and lead to
strabismus. However, the causes of concomitant strabismus are often unclear.
The following causes have been identified to date:
❖ Genetic factors: Approximately 60% of children with strabismus have afamily
history of increased incidence.
❖ Uncorrected refractive errors are partially responsible for the occurrenceof strabismus.
Children with hyperopia
(farsightedness) tend to have esotropia.
This is because convergence and accommodation are coupled.Children with
hyperopia have to accommodate without
converging when gazing into the distance to compensate for their refractive
error. However, accommodation always triggers a convergence impulse that can
cause esotropia.
❖Insufficient fusion: This can occur in conjunction withanisometropia(unequal refractive power in the two eyes) and aniseikonia (unequal reti-nal image size). It can also occur in heterophoria (latent strabismus) after
one eye has been covered with a bandage for a prolonged period.
❖Unilateral visual impairment: Severe nearsightedness, corneal scarring,lens opacities
(cataract), macular changes, and retinal disorders can cause secondary
strabismus. Retinal causes include
retinoblastoma, Coats’ dis-ease, retinopathy of prematurity, retinal
detachment, or central retinal scarring in congenital toxoplasmosis.
Any initial examination of a patient with
strabismus must invariably include examination of the fundus of both eyes under
mydriasis in addi-tion to examination of the anterior segments of the eye
❖Other possible causes of concomitant strabismus include:
–
Perinatal lesions such as preterm birth and asphyxia.
–
Cerebral trauma and encephalitis.
Pathophysiology:
Deviation of the visual axis of the deviating eye causesobjects
to be projected to noncorresponding points on the retina. One would expect
these patients suffer from constant double vision because the left and right
eyes supply different information to the brain. However, the central nervous
system utilizes two mechanisms to help avoid double vision in con-comitant
strabismus:
1. Suppression: A central inhibiting mechanism suppresses the
visualstimuli from the deviating eye. There are two different types of
suppres-sion:
Central scotoma: This visual field defect occurs when the perceived objectis
projected to the same location on the fovea in both eyes but strabismus causes
the eyes to perceive it as separate objects. As this would cause con-fusion,
the object projected on the fovea of the deviating eye is suppress-ed.
Fixation point scotoma: This visual field defect occurs when the image per-ceived by
the leading eye is projected to a point next
to the fovea in the deviating eye. This results in diplopia as the fixation
point does not lie within the fovea as it would in physiologic sight. The scotoma
occurs at this noncorresponding point next to the fovea to suppress the
diplopia.
2. Sensory adaptation: Inbinocularvision
with the gaze directed straightahead, the fixation point of the deviating eye can fall beyond the fovea. This produces anomalous retinal correspondence as the
fixation point in the nondeviating eye always falls on the fovea. This means that the image created in the deviating
eye is not as sharply focused as the
image in the leading eye and is suppressed.
Amblyopia secondary to suppression.Constant suppression in strabismus inthe form of a central and fixation scotomas can lead to severe amblyopia, especially in children below the age of six. The prospects for successful treat-ment decrease with age, and amblyopia becomes irreversible beyond the age of six to eight.
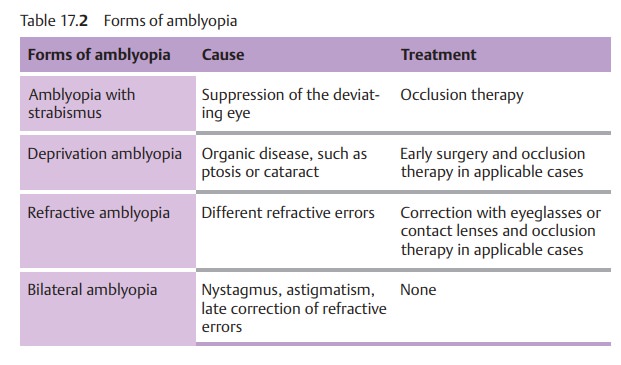
Amblyopia only occurs in
unilateral strabismus. In alternating strabismus, fixation or deviation
alternates between both eyes so that both eyes learn to see. A differential
diagnosis must distinguish amblyopia in stra-bismus from other forms of
amblyopia. These are listed in Table 17.2.
Strabismus occurring before the age of six
will frequently lead to ambly-opia. Early examination and treatment by an
ophthalmologist are crucial.
Related Topics