Chapter: Ophthalmology: Ocular Motility and Strabismus
Ophthalmoplegia and Paralytic Strabismus
Ophthalmoplegia and Paralytic Strabismus
Definitions
Ophthalmoplegia can affect one or more ocular
muscles at the same time. The condition may be partial (paresis, more common) or complete (paralysis, less common). The result is either gaze palsy or
strabismus (paralytic strabismus), depending on the cause (see next section)
and severity.
❖ Gaze palsy: Impairment or failure of coordinated eye movements. Forexample
in cyclovertical muscular palsy, the upward and downward gaze movements are
impaired or absent.
❖ Paralytic strabismus: Strabismus due to:
– Isolated
limited motility in one eye.
– Asymmetrical
limited motility in both eyes.
The angle of deviation does not remain
constant in every direction of gaze (as in concomitant strabismus) but
increases in the direction of pull of the para-lyzed muscle. This is referred
to as an incomitant angle of
deviation.
Etiology and forms of ocular motility disturbances:
Two forms are distin-guished.
❖Congenital ocular motility disturbances may be due to the followingcauses:
–
Prenatal encephalitis.
–
Aplasia of the ocular muscles.
– Birth
trauma.
❖ Acquired ocular motility disturbances may be due to the followingcauses:
–
Diabetes mellitus.
– Multiple
sclerosis.
–
Intracranial tumors.
–
Arteriosclerosis.
–
Central ischemia (apoplexy).
– AIDS.
–
Trauma and other causes.
Ocular motility disturbances are either
neurogenic, myogenic, or due to mechanical causes.
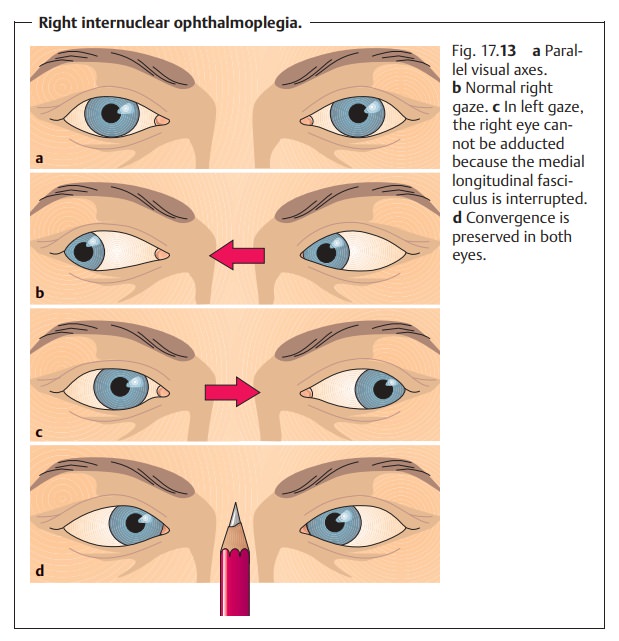
Neurogenic ocular motility disturbances (see also ophthalmoplegia second-ary to
cranial nerve lesions) are distinguished according to the location of the
lesion (Table 17.3):
❖ Lesions of the nerves supplying the ocular muscles.This condition is referredto as an infranuclear ocular motility disturbance
and is the most common cause of paralytic strabismus. The following nerves may
be affected:
– Oculomotor nerve lesions are rare and cause
paralysis of several muscles.
– Trochlear nerve lesions are common and cause
paralysis of the superior oblique.
– Abducent nerve lesions are common and cause
paralysis of the lateral rectus.
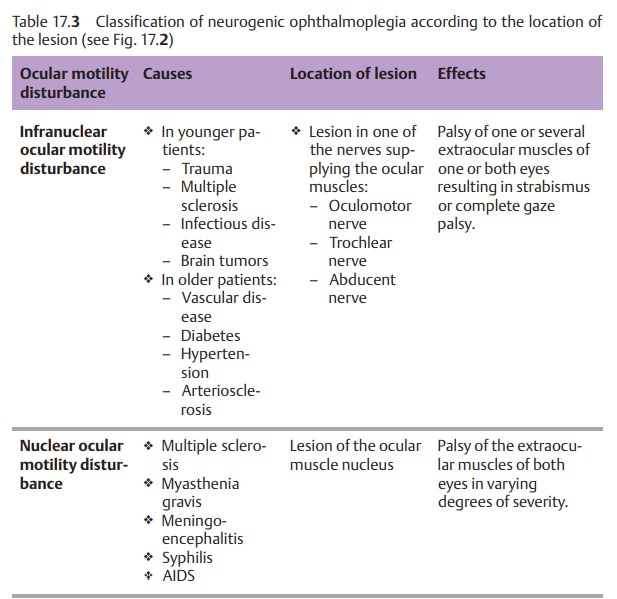
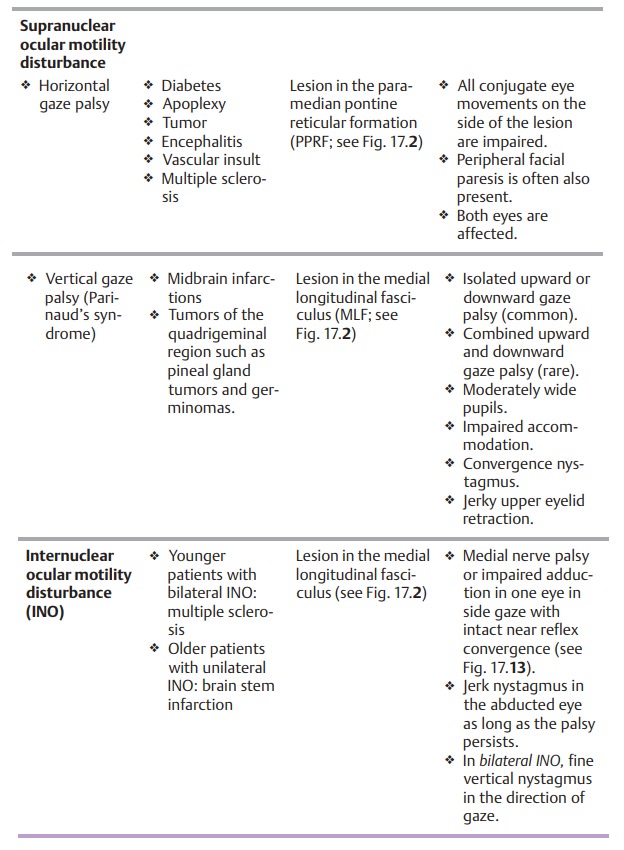
❖ Lesions of the ocular muscle nuclei. This condition is referred to as a nuclear ocular motility disturbance (see Fig. 17.2)
The oculomotor nuclei supply both sides but
the nerves are not close together. Therefore, bilateral palsy suggests a
nuclear lesion, whereas unilateral palsy suggests a lesion of one nerve.
❖ Lesions of the gaze centers. This condition is referred to as a supranuclear ocular motility disturbance (see gaze centers, Fig.
17.2). It very often
causes gaze palsy.
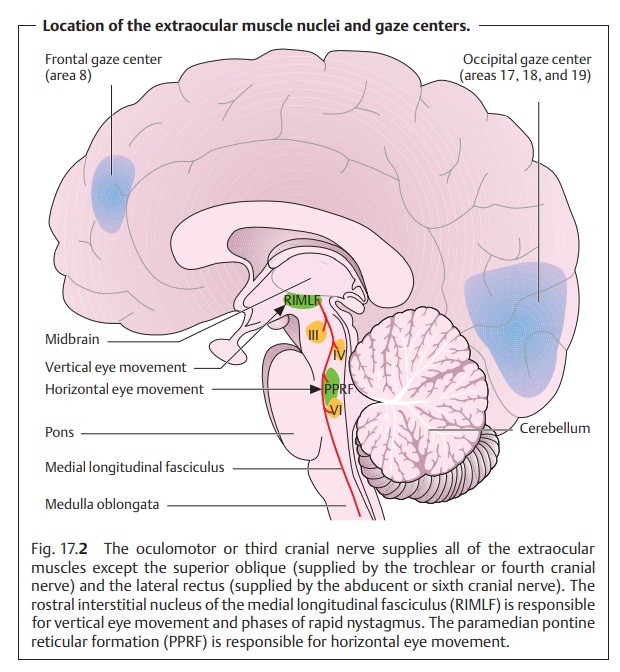
❖Another possible but rare condition is a lesion of the fibers connecting twonuclei. This condition is referred to as an internuclear ocular motility dis-turbance and may occur as a result of a lesion of the medial longitudinal fasciculus (see Figs. 17.2 and 17.13, Internuclear ophthalmoplegia).
Myogenic ocular motility disturbances are rare. These include palsies due tothe
following causes:
❖ Graves’ disease is the most common cause of myogenic ocular motility
dis-turbances. Because it alters the contractility and ductility of the ocular
muscles, it can result in significant motility disturbances.
❖ Ocular myasthenia gravis is a disorder of neuromuscular transmissioncharacterized by the presence of acetylcholine receptor antibodies. Typi-cal symptoms of ocular myasthenia gravis include fluctuating weaknessthat is clearly attributable to any one cranial nerve. The weakness typically increases in severity during the course of the day with fatigue. Important diagnostic aids include the following tests.
– Simpson test: The patient is asked to gaze
upward for one minute. Gradual drooping of one of the patient’s eyelids during
the test due to fatigue of the levator palpebrae strongly suggests myasthenia
gravis.
– Tensilon (edrophonium chloride) test: This
test is used to confirm the diagnosis. The patient is given 1 – 5 mg of
intravenous Tensilon (edro-phonium chloride). Where myasthenia gravis is
present, the paresis will disappear within a few seconds. (Refer to a textbook
of neurology for a detailed description of this test.)
❖Chronic progressive external ophthalmoplegia (CPEO) is a usually bilateral,gradually progressive
paralysis of one or more extraocular muscles. In the final stages it results in
complete paralysis of both eyes. Because the paral-ysis is symmetric the patient
does not experience strabismus or double vision.
❖ Ocular myositis is inflammation of one or more extraocular muscles.
Thepathogenesis is uncertain. Ocular motility is often limited not so much in
the direction of pull of the inflamed muscle as in the opposite direction.
While there is paresis of the muscle, it is characterized primarily by
insufficient ductility. Often additional symptoms are present, such as pain
during eye movement.
Mechanical ocular motility disturbances include palsies due to the followingcauses:
❖ Fractures. In a blowout fracture for example, the fractured floor of the
orbitcan impinge the inferior rectus and occasionally the inferior oblique.
This can interfere with upward gaze and occasionally produce strabismus.
❖ Hematomas.
❖Swellingin the orbit or facial bones, such as can occur in an orbital
abscessor tumor.
Symptoms:
Strabismus:Paralysis of one or more ocular muscles can cause itsrespective
antagonist to dominate. This results in a typical strabismus that allows which
muscle is paralyzed to be determined (see Diagnostic con-siderations). This is
readily done especially in abducent or trochlear nerve palsy as the abducent
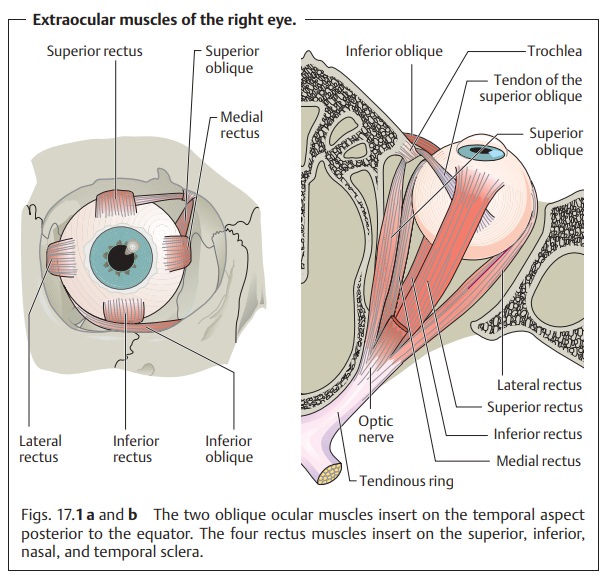
nerve and the trochlear nerve each supply only one extraocular muscle (see Fig.
17.1).
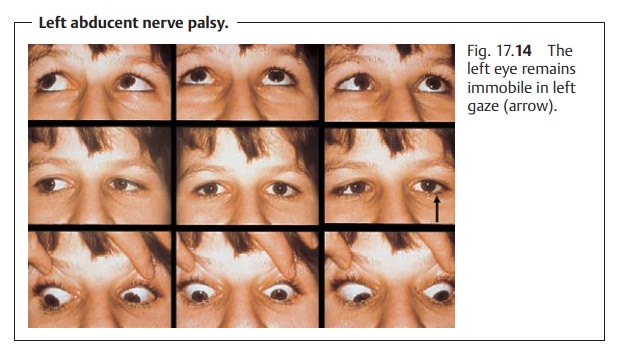
Example: abducent nerve palsy (Fig. 17.14). A
lesion of the abducent nerve par-alyzes the lateral rectus so that the eye can
no longer by abducted. This
paraly-sis also causes the muscle’s antagonist, the medial rectus, to dominate.
Because this muscle is responsible for adduction,
the affected eye remains medially rotated.
Gaze palsy. Symmetrical paralysis of one or more muscles of both eyes
limitsocular motility in a certain direction. For example, vertical gaze palsy or Pari-naud’s syndrome, which primarily occurs
in the presence of a pineal glandtumor, involves a lesion of the rostral
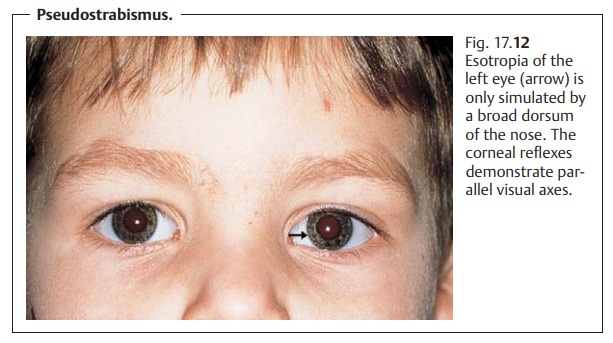
interstitial nucleus of the medial longi-tudinal fasciculus (see Fig. 17.12). Paralysis of all extraocular muscles leads to complete gaze palsy. Gaze palsy
suggests a supranuclear lesion, i.e., a lesion in the gaze centers. Examination
by a neurologist is indicated in these cases.
Double vision.Loss of binocular coordination between the two eyes due toophthalmoplegia leads to double vision. Normal vision may be expected in patients with only moderate paresis. As the onset of paresis is usually sudden, double vision is the typical symptom that induces patients to consult a physician. Some patients learn to suppress one of the two images within a few hours, days, or weeks. Other patients suffer from persistent double vision. Children usually learn to suppress the image quicker than adults.
Causes.Double vision occurs when the image of the fixated object only
fallson the fovea in one eye while falling on a point on the peripheral retina
in the fellow eye. As a result, the object is perceived in two different
directions and therefore seen double (Fig. 17.15a and b). The double
image of the deviating eye is usually somewhat out of focus as the resolving
power of the peripheral retina is limited. Despite this, the patient cannot
tell which is real and which is a virtual image and has difficulty in reaching
to grasp an object.
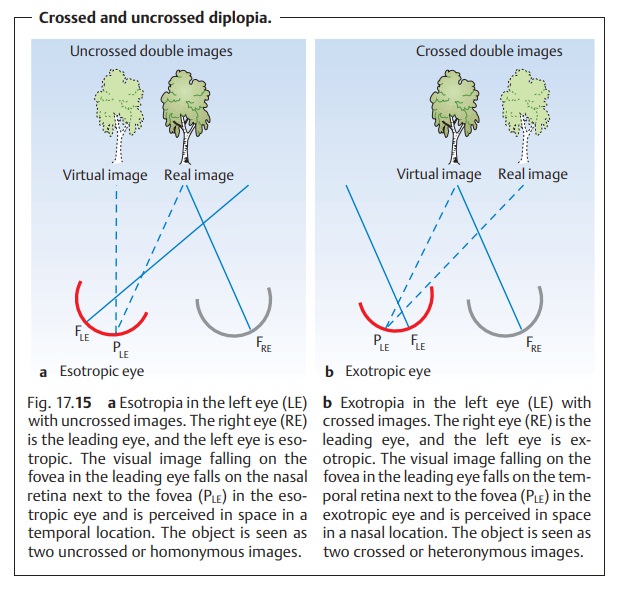
The distance
between the double images is greatest in ophthalmoplegia in the original
direction of pull of the affected muscle.
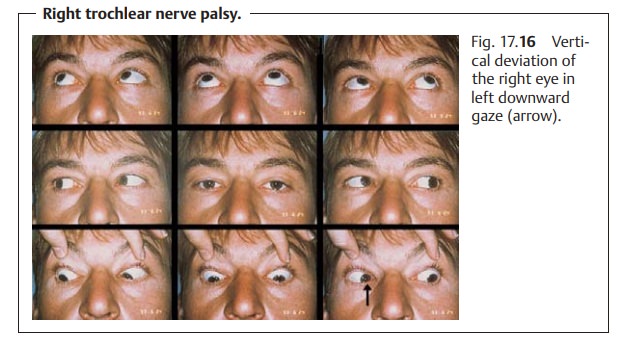
Example: trochlear nerve palsy (Fig. 17.16). The superior oblique supplied bythe trochlear nerve is
primarily an intorter and depressor in adduction (see Table 17.1); it is also an abductor when the
gaze is directed straight ahead. Therefore, the limited motility and upward
deviation of the affected eye is most apparent in depression and intorsion as
when reading. The distance between the double images is greatest and the
diplopia most irritating in this direction of gaze, which is the main direction
of pull of the paralyzed superior oblique.
Compensatory head posture.The patient can avoid diplopia only by attempt-ing to avoid using the paralyzed muscle. This is done by assuming a typical compensatory head posture in which the gaze lies within the binocular visual field; the patient tilts his or her head and turns it toward the shoulder opposite the paralyzed eye.
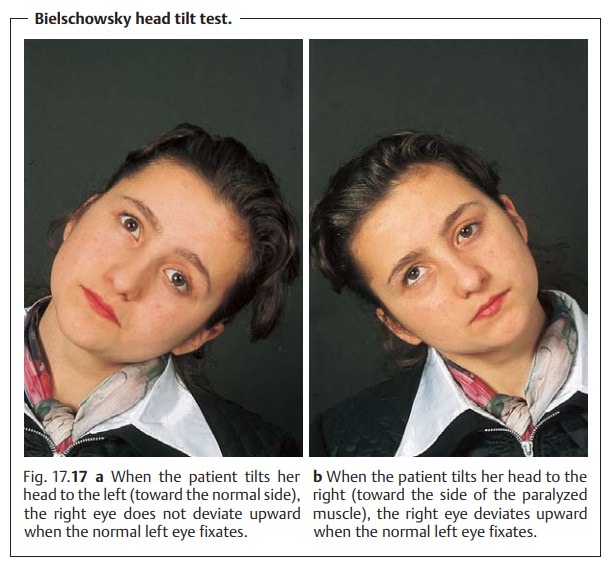
The Bielschowsky
head tilt test uses this posture to confirm the diagnosis of trochlear or
fourth cranial nerve palsy (Fig. 17.17). In this test, the examiner tilts the patient’s head toward
the side of the paralyzed eye. If the patient then fixates with the normal eye,
the paralyzed eye will deviate. When the patient’s head is tilted toward the
normal side, there will be no vertical devia-tion (see Diagnostic
considerations for further diagnostic procedures).
Ocular torticollis.The compensatory head posture in trochlear nerve palsy isthe
most pronounced and typical of all cranial nerve palsies. Congenital trochlear nerve palsy can lead to what is known as
ocular torticollis.
Incomitant angle of deviation.The angle of deviation in paralytic strabismusalso varies with the direction of gaze and is not constant as in concomitant strabismus. Like the distance between the double images, the angle of devia-tion is greatest when the gaze is directed in the direction of pull of the paralyzed muscle. The angle of deviation may be classified according to the which eye fixates.
– A primary
angle of deviation is the angle of deviation when fixating with the normal
eye. This angle is small.
– A secondary
angle of deviation is the angle of deviation when fixating with the
paralyzed eye. This angle is large.
The secondary angle of deviation is always
larger than the primary angle. This is because both the paralyzed muscle and
its synergist in the fellow eye receive increased impulses when the paralyzed
eye fixates. For example when the right eye fixates in right abducent nerve
palsy, the left medial rectus will receive increased impulses. This increases
the angle of deviation.
Cranial nerve palsies:
The commonest palsies are those resulting
fromcranial nerve lesions. Therefore, this section will be devoted to examining
these palsies in greater detail than the other motility disturbances listed
under Etiology. It becomes evident from the examples of causes listed here that
a diagnosis of ophthalmoplegia will always require further diagnostic
procedures (often by a neurologist) to confirm or exclude the presence of a
tumor or a certain underlying disorder such as diabetes mellitus.
Abducent nerve palsy:
Causes: The main causes of this relatively common palsy include vascular
dis-ease (diabetes mellitus, hypertension, or arteriosclerosis) and
intracerebral tumors. Often a tumor will cause increased cerebrospinal fluid
pressure, which particularly affects the abducent nerve because of its long
course along the base of the skull. In children,
these transient isolated abducent nerve pal-sies can occur in infectious
diseases, febrile disorders, or secondary to inocu-lations.
Effects: The lateral rectus is paralyzed, causing its antagonist, the
medial rec-tus, to dominate. Abduction is impaired or absent altogether, and
the affected eye remains medially rotated (see Fig. 17.14). Horizontal homonymous (uncrossed) diplopia is present (see
Fig. 17.15). The images are farthest
apart in abduction.
Example: right abducent nerve palsy.
❖ Compensatory head posture with right tilt.
❖ Esotropia when the gaze is directed straight
ahead.
❖Largest angle of deviation and distance between
images in right gaze.
❖ No angle of deviation or diplopia in left
gaze.
Retraction syndrome (special form of abducent nerve palsy):
Causes: Retraction syndrome is a congenital unilateral motility
disturbanceresulting from a lesion to the abducent nerve acquired during
pregnancy.
Effects: The lateral rectus is no longer supplied by the abducent nerve
but byfibers from the oculomotor nerve that belong the medial rectus. This has
several consequences. As in abducent
nerve palsy, abduction is limited and
slight esotropia is usually present. In
contrast to abducent nerve palsy, the globe recedes into the orbital cavity
when adduction is attempted. This
nar-rows the palpebral fissure. This retraction
of the globe in attempted adduction results from the simultaneous outward
and inward pull of two antagonists on the globe because they are supplied by
the same nerve (oculomotor nerve).
Trochlear nerve palsy:
Causes: The commonest cause is trauma; less common causes include
vascu-lar disease (diabetes mellitus, hypertension, and arteriosclerosis).
Trochlear nerve palsy is a relatively common phenomenon.
Effects: The superior oblique is primarily an intorter and a depressor in
adduc-tion. This results in upward vertical deviation of the paralyzed eye in
adduc-tion and vertical strabismus (see Fig. 17.16). Patients experience vertical diplopia; the images are farthest
apart in depression and intorsion. Compen-satory head posture is discussed in
the section on symptoms. Diplopia is absent in elevation.
Oculomotor nerve palsy:
Causes:
❖ Complete oculomotor nerve palsy: Every intraocular and almost
everyextraocular muscle is affected, with loss of both accommodation and
pupil-lary light reaction. The failure of the parasympathetic fibers in the
oculo-motor nerve produces mydriasis. Ptosis is present because the levator
pal-pebrae is also paralyzed. The paralyzed eye deviates in extorsion and
depression as the function of the lateral rectus and superior oblique is
pre-served. Patients do not experience diplopia because the ptotic eyelid covers
the pupil.
❖ Partial oculomotor nerve palsy:
– External oculomotor nerve palsy (isolated
paralysis of the extraocular muscles
supplied by the oculomotor nerve; see Fig. 17.1) is character-ized by deviation in extorsion
and depression. If the ptotic eyelid does not cover the pupil, the patient will
experience diplopia.
– Internal oculomotor nerve palsy is isolated
paralysis of the intraocular muscles
supplied by the oculomotor nerve. This is characterized by loss of
accommodation (due to paralysis of the ciliary muscle) and mydria-sis (due to
paralysis of the sphincter pupillae). Patients do not ex-perience diplopia as
there is no strabismic deviation (see also tonic pupil and Adie syndrome).
Combined cranial nerve palsies. The third, fourth, and sixth cranial nervescan be simultaneously
affected, for example in a lesion at the apex of the orbi-tal cavity or in the cavernous sinus. Clinical
suspicion of combined lesion may be supported by a corneal sensitivity test as
the ophthalmic division of the trigeminal nerve, which provides sensory supply
to the cornea, courses through the cavernous sinus. Where there is loss of
corneal sensitivity, whether the lesion is located in the cavernous sinus must
be determined.
Diagnosis of ophthalmoplegia:
Examination of the nine diagnostic posi
The patient is asked to follow the movements ofthe examiner’s
finger or a pencil with his or her eyes only. The six cardinal directions of
gaze (right, upper right, lower right, left, upper left, lower left) provide
the most information; upward and downward movements are per-formed with several
muscles and therefore do not allow precise identification of the action of a
specific muscle. Immobility of one eye when the patient attempts a certain
movement suggests involvement of the muscle responsible for that movement.
The Bielschowsky head tilt
test is performed only
where trochlear nerve palsy is suspected (see symptoms).
Measuring the angle of deviation.Measuring this angle in the nine diagnos-tic directions of gaze provides information about the severity of the palsy, which is important for surgical correction. This is done using a Harms tangent table (Fig. 17.18).
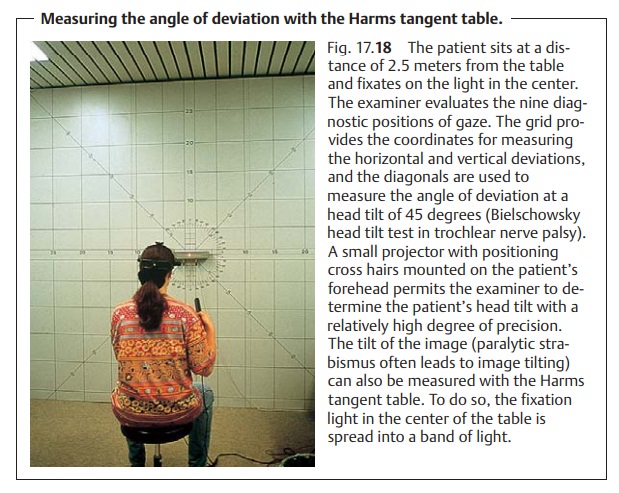
In addition to the vertical and horizontal
graduations of the Maddox’s cross, the Harms table also has diagonals. These
diagonals permit the examiner to measure the angle of deviation even in
patients with a com-pensatory head tilt, such as can occur in trochlear nerve
palsy.
Differential diagnosis:
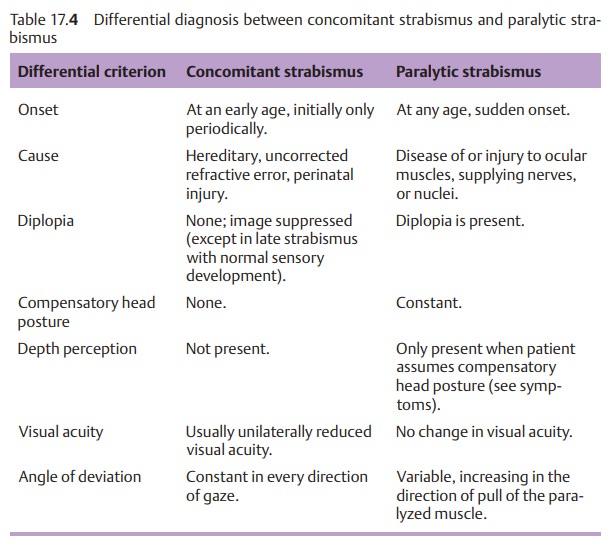
Table 17.4shows
the most important differencesbetween paralytic strabismus and concomitant
strabismus.
Treatment of ophthalmoplegia:
Surgery for paralytic strabismus should bepostponed for at least one year to allow for possible spontaneous remission. Preoperative diagnostic studies to determine the exact cause are indicated to permit treatment of a possible underlying disorder, such as diabetes mellitus. Severe diplopia may be temporarily managed by alternately patching the eyes until surgery. Alternatively, an eyeglass lens with a prism correction for the paralyzed eye may be used to compensate for the angle of deviation and eliminate diplopia. Eyeglasses with nonrefracting lenses may be used for patients who do not normally wear corrective lenses. Prism lenses may not always be able to correct extreme strabismus. If surgery is indicated, care must be taken to correctly gauge the angle of deviation.
The goal
of surgery is to eliminate diplopia in the normal visual field, i.e., with head
erect, in both near and distance vision. It will not be possible to surgically
eliminate diplopia in every visual field.
Procedure: Theantagonist of the
respective paralyzed musclecan beweakenedby
recession. Resecting or doubling the paralyzed muscle can additionally reduce
the angle of deviation.
Strabismus surgery for ophthalmoplegia is
possible only after a one-year regeneration period.
Related Topics