Chapter: Surgical Pathology Dissection : The Cardiovascular, Respiratory System
The Explanted Heart: Surgical Pathology Dissection
Heart, Heart Valves, and Vessels
The Explanted Heart
The
examination of hearts explanted from heart transplant recipients provides a
unique opportunity to study cardiac pathology. Moreover, in some instances it
influences posttransplant therapy and prognosis.
The
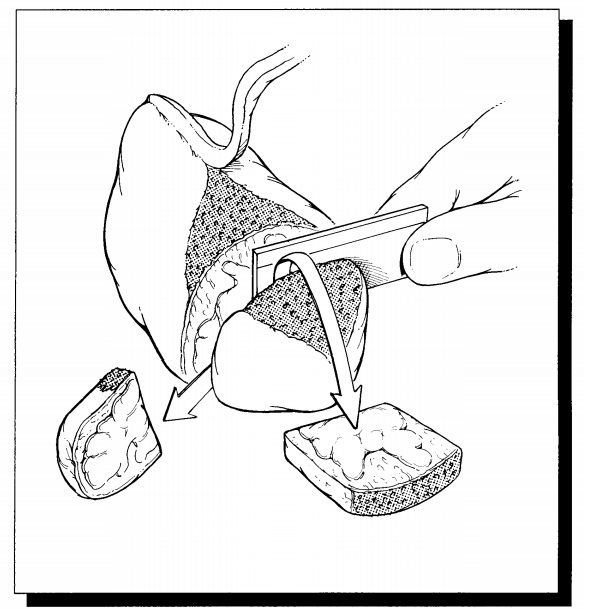
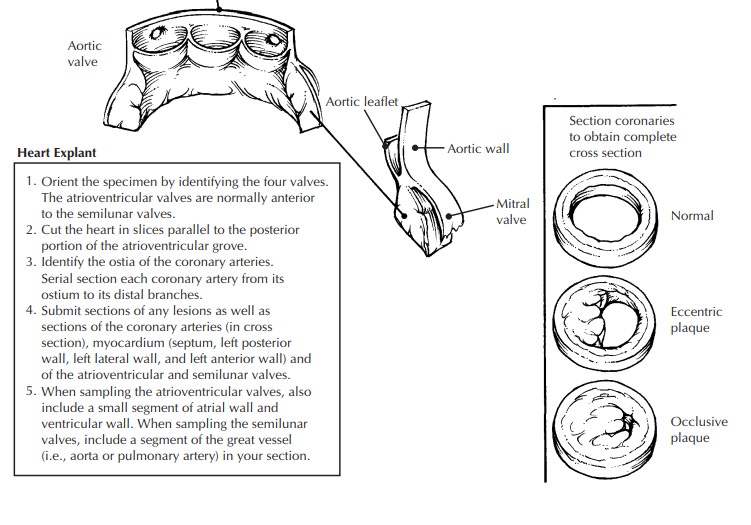
specimen should be emptied of clotted blood and weighed before examination.
Document the general shape (globular or normal) and consistency (firm or
floppy) of the heart, and identify the major structures (ventricles, atria,
pulmonary artery, root of the aorta). In most instances the atria are partially
or completely missing, and this should be recorded. The pulmonary artery and
valve as well as the aortic root and valve may be intact or partially torn
during the resection of the heart. Document the anatomy. Do the great vessels
emerge from the heart in their normal anatomic location? If you suspect a
congenital heart disease, you should work carefully with the clinician and
review appropriate preoperative imaging, as the clinical history guides your
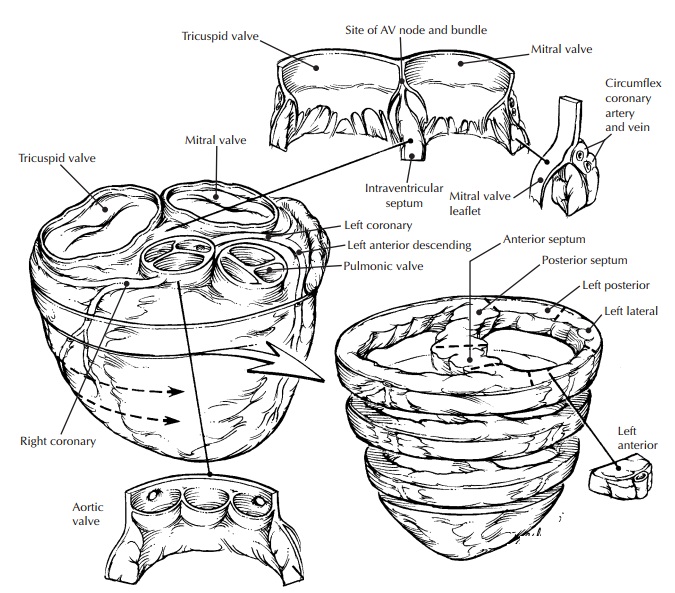
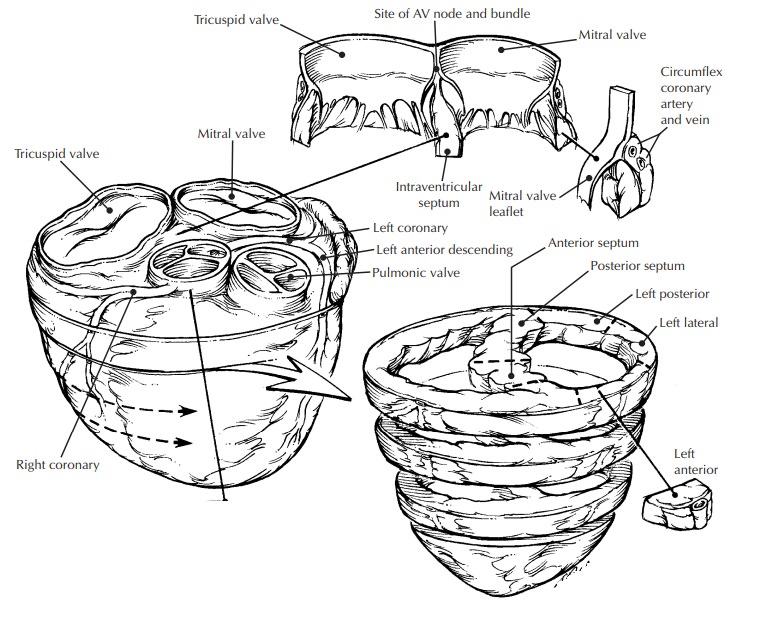
dissection. Further examination of the heart is simplified if you approach the
three layers of the heart (epicardium, myocardium, endocardium), the valves,
and the coronary vessels systematically.
Start
with the epicardium. Examination of the external surface of the heart should
document the presence or absence of petechiae, adhesions (fibrous or
fibrinous), scar (focal or extensive), calcification, and grafts (vascular or
synthetic material).
If
grafts are present, document their location and the status of the anastomoses.
Grossly examine the valves as best you can before sectioning the heart.
Document any thrombi or vegetations. In most instances transverse sectioning of
the heart at 1-cm intervals from the apex to just below the atrioventricular
apparatuses allows the diagnosis of hypertrophy and/or dilatation, and it demonstrates
the greatest surface area of the sectioned myocardium. Examine the myocardium
carefully. The size and location of recent or remote infarcts, focal punctate
lesions, hemorrhages, fibrosis, or frank necrosis should be noted. Examination
of the myocardium should be guided by the patient’s clinical history, as some
pathologic conditions affect specific areas of the heart. For example,
sarcoidosis tends to begin in the basal portion of the heart close to the
atrioventricular apparatus; on the other hand, right ventricular dysplasia
affects the right ventricular free wall during early stages and spreads to the
left ventricle late in the disease. Next, turn your attention to the
endocardium and valves. Are the endocardial surfaces smooth, or are focal lesions
noted? Examine the atrioventricular and semilunar valves, as described later
under Heart Valves. Lastly, the coronary arteries can be examined. Do this
systematically. Start at the orifice of the left main coronary artery and
serially section the vessel proceeding down the left anterior descending and
left circumflex arteries as far as possible. Similarly, section the right
coronary artery from its orifice to its distal branches. Document the course of
these vessels. Are they in their normal anatomic location? As described in
detail under Arteries and Veins, examine the lumen of each vessel for thrombi;
examine the intima for evidence of intimal proliferation, hemorrhage, or
atheromatous plaques; and document the location and percentage narrowing caused
by any lesions. For example, your report could include “there is 90% stenosis
of the left anterior descending coronary arteries just proximal to the take-off
of the first diagonal branch.” It is not uncom-mon to receive specimens with
one or more metal stents within the coronaries. If stents are present, describe
their presence and location. Section the vessel close to the stent and inspect
its lumen. Sectioning through the stents is not feasible in common pathology
practice.
The
heart can now be sampled. Samples of myocardium for electron microscopy should
always be procured. Also in modern pathology practice, pieces of each ventricle
should be frozen in optimal controlled temperature (OCT) com-pound and also
snap-frozen for any molecular diagnostic test that may be needed later.
Sections submitted in formalin for histopathologic exami-nation should include
a minimum of four sec-tions of the ventricles (interventricular septum,
anterior wall, lateral wall, and posterior wall); a section of any valve lesions;
a section of the mitral and aortic valves; and representative sec-tions of each
of the coronary arteries. The section of the anterior wall can often be taken
to include the left anterior descending coronary artery. Sample any additional
area showing gross patho-logic changes. Examination of the atrioventricu-lar
conduction system is often possible, whereas in most instances examination of
the sinoatrial node is not. It is easy to sample the conduction system if
needed (see The Conducting System). Remember that atherosclerosis and some
valve lesions can be quite calcified, and therefore decal-cification should be
performed as necessary.
Related Topics