Chapter: Obstetrics and Gynecology: Sexually Transmitted Diseases
Syphilis
Syphilis
In the United States, the
incidence of syphilis declined steadily in the 1990s and reached its lowest
rate in 2000. Beginning in 2001, the rate of syphilis began to increase,
especially among men who have sex with men. Rates in women also increased,
although not as steeply. Between 2005 and 2006, the number of reported syphilis
cases increased 11.8%. Between 2001 and 2008, the overall increase in cases of
syphilis was 76%. In addition, after a 14-year decline, the rate of congenital
syphilis increased 3.7% between 2005 and 2006. This increase may relate to the
increase in the rate of syphilis that has occurred in past several years. One
reason suggested for the rise in syphilis rates overall is the increasing use
of nonpenicillin anti-biotics to treat penicillin-resistant gonorrhea; in the
past, penicillin treatment of gonorrhea provided treatment for coexisting
syphilis.
Treponema pallidum, the
causative organism ofsyphilis, is one of a small group of spirochetes that are
vir-ulent in humans. Because this motile
anaerobic spirochete canrapidly invade intact moist mucosa, the most common
sites of entry for women are the vulva, vagina, and cervix. Transplacentalspread
may occur at any time during pregnancy and can result in congenital syphilis.
DIAGNOSIS
Syphilis can be a long-term
disease with several stages. Primary syphilis, the first stage of the disease, is
characterizedby the appearance of a chancre
at the site of entry approximately 10 to 60 days after infection with T.
pallidum. The chancrehas a firm, punched-out appearance and has rolled edges
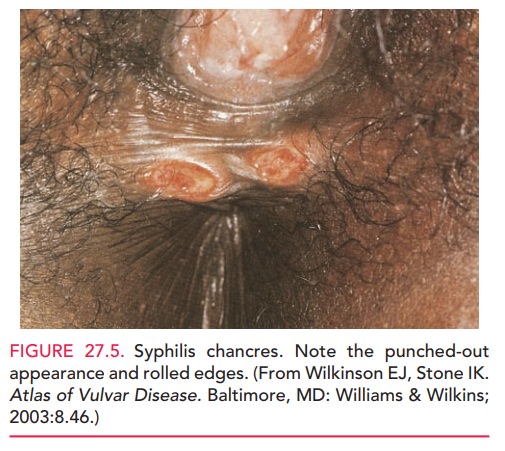
Because it is small
and painless, the chancre may be missed during routine physical examination.
Ade-nopathy or other mild systemic symptoms may also be pre-sent. The chancre
heals spontaneously within 3 to 6 weeks. Serologic-testing results at this
stage of syphilis generally are negative.
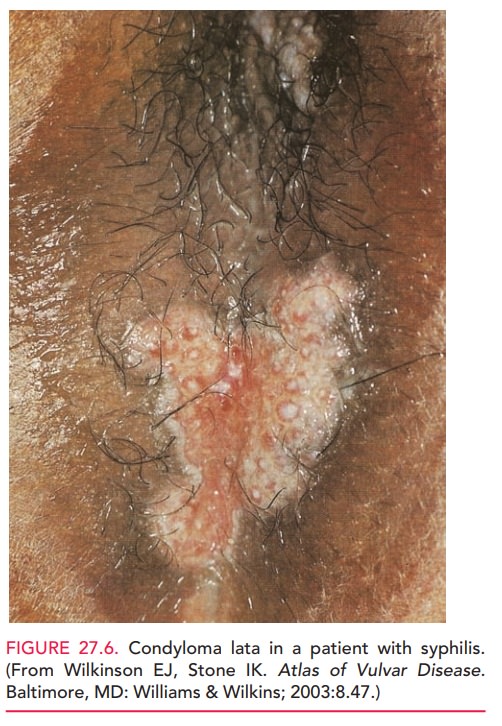
Four to 8 weeks after the primary
chancre appears, manifestations of secondary
syphilis develop. This stage
ischaracterized by a skin rash that often appears as rough, red or brown
lesions on the palms of the hands and soles of the feet. Othersymptoms
include lymphadenopathy, fever, headache, weight loss, fatigue, muscle aches,
and patchy hair loss. Highly infective secondary eruptions, called
mucocuta-neous mucous patches, occur in 30% of patients during this stage. In
moist areas of the body, flat-topped papules may coalesce, forming condyloma
lata (Fig. 27.6). These may be distinguished from venereal warts by their broad
base and flatter appearance.
In
untreated individuals, this stage also resolves sponta-neously in 2 to 6 weeks,
and the disease enters the latent phase.During
the latent stage, the patient has no signs or symp-toms of the disease,
although serologic tests are positive. In the late or tertiary stages of the disease, transmission of the infection is
unlikely, except via blood transfusion or placen-tal transfer. However, severe
damage to the central nervous and cardiovascular systems develop, along with
ophthalmic and auditory abnormalities. Destructive, necrotic, granulo-matous
lesions, called gummas, may develop
1 to 10 years after infection.
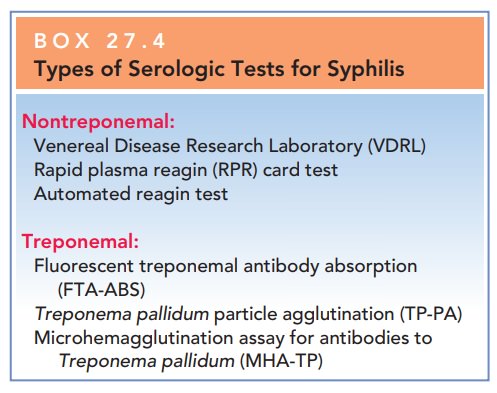
DIAGNOSIS
Syphilis is determined by identifying motile spirochetes on dark-field microscopic examination and direct fluores-cent antibody tests of material from primary or secondary lesions or lymph node aspirates.
Presumptive diagnosis is possible with nontreponemal tests (the Venereal
Disease Research Laboratory [VDRL] and rapid plasma reagin [RPR]) and
treponemal tests (e.g., fluorescent treponemal antibody absorption [FTA-ABS]
and Treponema pallidum particle
agglutination [TP-PA]) [Box 27.4]. The
use of only
Box 27.4
Types of Serologic Tests for Syphilis
Nontreponemal:
Venereal
Disease Research Laboratory (VDRL)
Rapid
plasma reagin (RPR) card test
Automated
reagin test
Treponemal:
Fluorescent
treponemal antibody absorption (FTA-ABS)
Treponema pallidum particle agglutination (TP-PA)
Microhemagglutination
assay for antibodies to
Treponema pallidum (MHA-TP)
A woman
with a positive treponemal testwill usually have this positive result for life,
irrespective of treatment or activity of the disease. When neurosyphilis is
suspected, a lumbar puncture, with a VDRL performed on the spinal fluid, is
required.
TREATMENT
Syphilis is treated with
benzathine penicillin G. The patient should be followed by quantitative VDRL
titers and exam-inations at 3, 6, and 12 months, and should abstain from sexual
intercourse until lesions are completely healed.
Related Topics